Sunday Poster Session
Category: Small Intestine
P2021 - A Case of Intense Pruritus in the Setting of Invasive Mucinous Adenocarcinoma of the Ampulla of Vater
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AK
Alishbah Khan, BS
University of Texas at Tyler School of Medicine
Tyler, TX
Presenting Author(s)
Alishbah Khan, BS1, ChiAyrsh Ford, DO, BS2, Abdelrazig Suliman, MD3
1University of Texas at Tyler School of Medicine, Tyler, TX; 2University of Texas at Tyler Health Science Center, Tyler, TX; 3University of Texas, Tyler, TX
Introduction: Ampullary cancer, a rare form of cancer that originates from the ampulla of Vater, is a unique condition, accounting for only 0.2% of gastrointestinal cancers. We discuss a case of a patient who, despite the rarity of this cancer, presented to the ER with intense pruritus and was found to have invasive mucinous adenocarcinoma of the ampulla, leading to biliary and pancreatic duct obstruction.
Case Description/
Methods: A 62-year-old female with a history of coronary artery disease s/p CABG and a remote history of tobacco and alcohol use presented with complaints of nausea, vomiting, abdominal pain, dark urine, jaundice, and 20 lbs of weight loss over the past year. Full-body intense pruritus prompted her to come to the ER. CT scan of the abdomen/pelvis with contrast showed 3x1.3x2.4 cm low attenuation neoplasm at the pancreatic head and ampulla, resulting in an abrupt cut off of the common bile and pancreatic duct. Labs were notable for elevated liver enzymes, alkaline phosphatase, and direct bilirubin. Her CA 19-9 was 37, and CEA was 3.1. GI was consulted for EGD and EUS with biopsy. Surgery and oncology were consulted after the biopsy revealed invasive adenocarcinoma in the pancreatic head and adenomatous epithelium with high-grade dysplasia from the ampulla of Vater. She subsequently underwent ERCP with stent placement and pancreaticoduodenectomy. Whipple pathology showed invasive mucinous adenocarcinoma arising from the duodenum, invading through the muscularis propria and into the adjacent pancreatic head. Our patient with pT4pN0 stage 2 malignancy was safely discharged 11 days after admission a with resolution of most of her initial symptoms.
Discussion: Our patient initially experienced emotional distress and was reluctant to undergo diagnostic testing. The value of a multidisciplinary team in providing comprehensive care and patient support, along with the crucial role of empathetic communication, was learned. These factors ultimately led our patient to agree to a biopsy and Whipple procedure, which significantly improved her pruritus. Further outpatient workup consists of a CT scan of the chest, an outpatient PET scan, and obtaining circulating tumor DNA. Oncology recommended testing for microsatellite instability/ mismatch repair deficiency to be assessed on the tumor; if testing is positive, adjuvant chemotherapy with either FOLFOX or CAPOX was discussed. Since being discharged, our patient has followed up with surgery and is due to follow up with oncology.
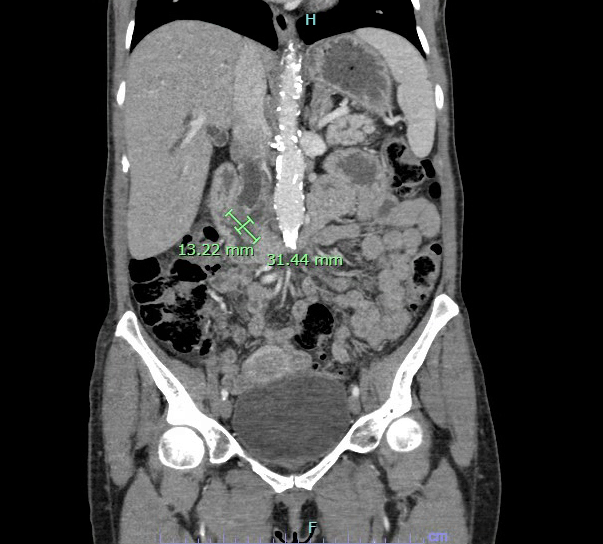
Figure: CT scan of the abdomen/pelvis with contrast showing 3x1.3x2.4 cm low attenuation neoplasm at the pancreatic head and ampulla, resulting in an abrupt cut off of the common bile duct and pancreatic duct.
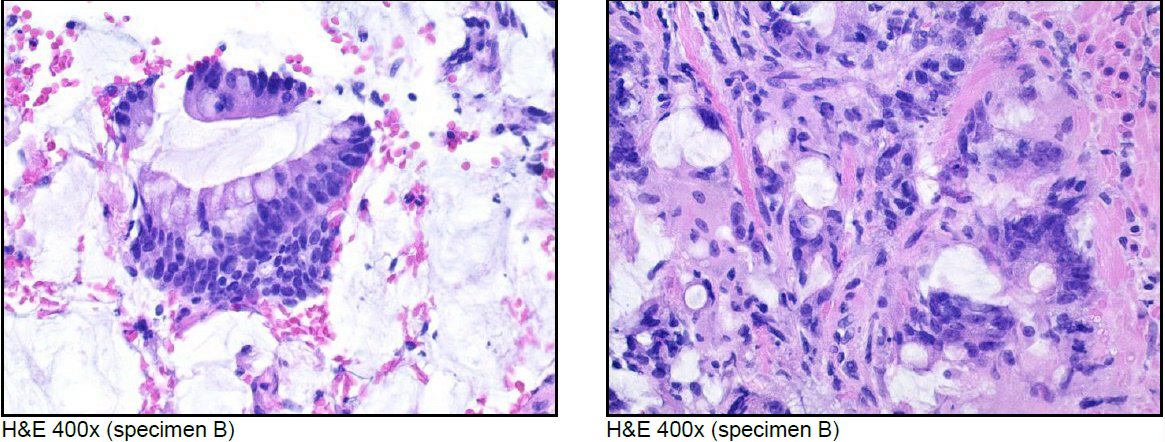
Figure: These tissue specimens represent tissue from the pancreatic head mass, indicating invasive adenocarcinoma.
Disclosures:
Alishbah Khan indicated no relevant financial relationships.
ChiAyrsh Ford indicated no relevant financial relationships.
Abdelrazig Suliman indicated no relevant financial relationships.
Alishbah Khan, BS1, ChiAyrsh Ford, DO, BS2, Abdelrazig Suliman, MD3. P2021 - A Case of Intense Pruritus in the Setting of Invasive Mucinous Adenocarcinoma of the Ampulla of Vater, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Tyler School of Medicine, Tyler, TX; 2University of Texas at Tyler Health Science Center, Tyler, TX; 3University of Texas, Tyler, TX
Introduction: Ampullary cancer, a rare form of cancer that originates from the ampulla of Vater, is a unique condition, accounting for only 0.2% of gastrointestinal cancers. We discuss a case of a patient who, despite the rarity of this cancer, presented to the ER with intense pruritus and was found to have invasive mucinous adenocarcinoma of the ampulla, leading to biliary and pancreatic duct obstruction.
Case Description/
Methods: A 62-year-old female with a history of coronary artery disease s/p CABG and a remote history of tobacco and alcohol use presented with complaints of nausea, vomiting, abdominal pain, dark urine, jaundice, and 20 lbs of weight loss over the past year. Full-body intense pruritus prompted her to come to the ER. CT scan of the abdomen/pelvis with contrast showed 3x1.3x2.4 cm low attenuation neoplasm at the pancreatic head and ampulla, resulting in an abrupt cut off of the common bile and pancreatic duct. Labs were notable for elevated liver enzymes, alkaline phosphatase, and direct bilirubin. Her CA 19-9 was 37, and CEA was 3.1. GI was consulted for EGD and EUS with biopsy. Surgery and oncology were consulted after the biopsy revealed invasive adenocarcinoma in the pancreatic head and adenomatous epithelium with high-grade dysplasia from the ampulla of Vater. She subsequently underwent ERCP with stent placement and pancreaticoduodenectomy. Whipple pathology showed invasive mucinous adenocarcinoma arising from the duodenum, invading through the muscularis propria and into the adjacent pancreatic head. Our patient with pT4pN0 stage 2 malignancy was safely discharged 11 days after admission a with resolution of most of her initial symptoms.
Discussion: Our patient initially experienced emotional distress and was reluctant to undergo diagnostic testing. The value of a multidisciplinary team in providing comprehensive care and patient support, along with the crucial role of empathetic communication, was learned. These factors ultimately led our patient to agree to a biopsy and Whipple procedure, which significantly improved her pruritus. Further outpatient workup consists of a CT scan of the chest, an outpatient PET scan, and obtaining circulating tumor DNA. Oncology recommended testing for microsatellite instability/ mismatch repair deficiency to be assessed on the tumor; if testing is positive, adjuvant chemotherapy with either FOLFOX or CAPOX was discussed. Since being discharged, our patient has followed up with surgery and is due to follow up with oncology.
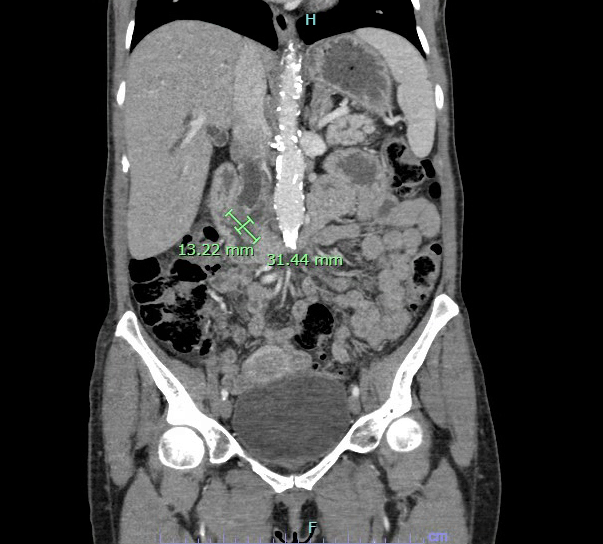
Figure: CT scan of the abdomen/pelvis with contrast showing 3x1.3x2.4 cm low attenuation neoplasm at the pancreatic head and ampulla, resulting in an abrupt cut off of the common bile duct and pancreatic duct.
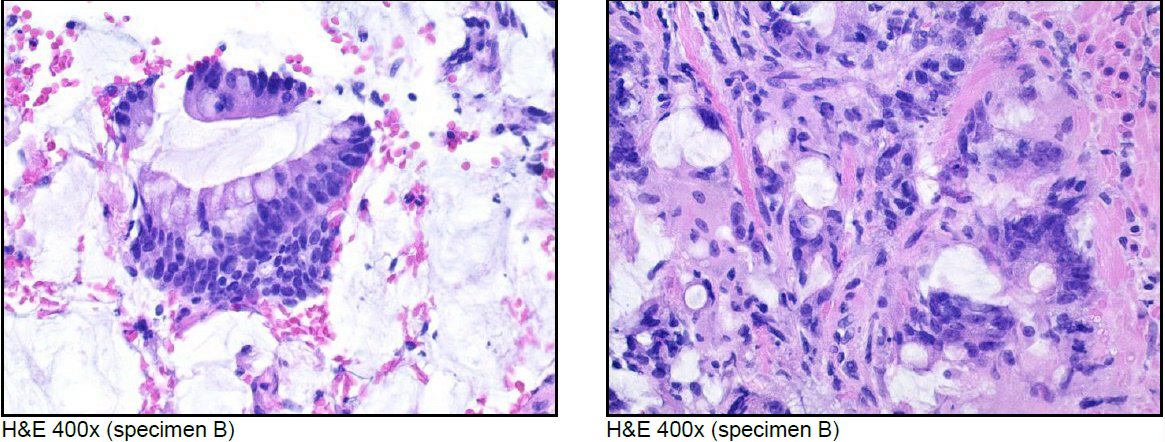
Figure: These tissue specimens represent tissue from the pancreatic head mass, indicating invasive adenocarcinoma.
Disclosures:
Alishbah Khan indicated no relevant financial relationships.
ChiAyrsh Ford indicated no relevant financial relationships.
Abdelrazig Suliman indicated no relevant financial relationships.
Alishbah Khan, BS1, ChiAyrsh Ford, DO, BS2, Abdelrazig Suliman, MD3. P2021 - A Case of Intense Pruritus in the Setting of Invasive Mucinous Adenocarcinoma of the Ampulla of Vater, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
