Sunday Poster Session
Category: Small Intestine
P2020 - Unusual Cause of Intestinal Perforation and Pneumobilia from Thyme Root Ingestion with Successful Endoscopic Treatment
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kaleb Lucas, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Kaleb Lucas, MD1, Agazi Gebreselassie, MD2
1Sinai Hospital, Baltimore, MD; 2Woodholme GI associates, Clarksville, MD
Introduction: This case will discuss the presentation of a 47 year old female patient presenting with acute abdominal pain and found to have an atypical foreign body ingestion on esophagogastroduodenoscopy (EGD), with resolution of symptoms after foreign body extraction.
Case Description/
Methods: A 47 year old female presented to the emergency department with concern for abdominal pain that had been persistent for 4 days. The pain began in her epigastrium and then migrated to the right upper quadrant. She also endorses episodes of nausea and vomiting. She describes having abdominal upset over the past several years, and notes particularly bothersome indigestion after eating greasy foods or when she eats too fast. She does endorse occasional reflux, although no worse than usual. Denies use of NSAIDs. She reports having an upper and lower endoscopy at an outside clinic about a year ago and was told that findings were normal. She denies undergoing any procedures, such as an ERCP, previously. Her liver enzymes and bilirubin are within normal limit.
CT scan of the abdomen/pelvis with contrast on admission noting marked thickening of the third portion of the duodenum and proximal jejunum, pneumobilia with a mildly distended common bile duct, probable small gallstones and mild gallbladder thickening, hepatic hemangioma, and enlarged fibrous uterus.
Decision was made to proceed with EGD.
Discussion: The patient was brought to the endoscopy unit and placed in the left lateral position for examination. The gastroscope was then advanced into the duodenum. Endoscopic findings were notable for diffuse edema of the second and third parts of the duodenum with narrowing of the lumen, and a foreign body (thyme root) was seen in the third part of the duodenum which was deeply impacted to the duodenal wall, causing a deep ulcer. The foreign body was gently removed with a forceps to the stomach, followed by Roth Net after applying a protective hood to the gastroscope. The small bowel mucosa beyond the edematous part was normal. The procedure was completed with withdrawal of the endoscope, no immediate post-procedural complications were observed. The patient was discharged 2 days after EGD with resolution of her symptoms and normalization of CT scan.
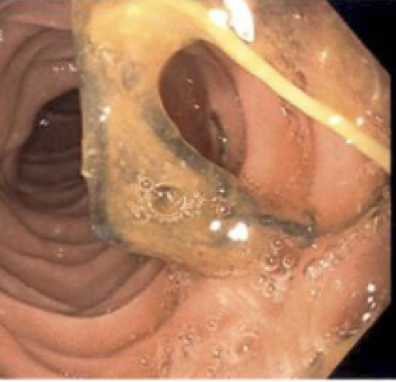
Figure: Thyme root embedded in duodenal wall
Disclosures:
Kaleb Lucas indicated no relevant financial relationships.
Agazi Gebreselassie indicated no relevant financial relationships.
Kaleb Lucas, MD1, Agazi Gebreselassie, MD2. P2020 - Unusual Cause of Intestinal Perforation and Pneumobilia from Thyme Root Ingestion with Successful Endoscopic Treatment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sinai Hospital, Baltimore, MD; 2Woodholme GI associates, Clarksville, MD
Introduction: This case will discuss the presentation of a 47 year old female patient presenting with acute abdominal pain and found to have an atypical foreign body ingestion on esophagogastroduodenoscopy (EGD), with resolution of symptoms after foreign body extraction.
Case Description/
Methods: A 47 year old female presented to the emergency department with concern for abdominal pain that had been persistent for 4 days. The pain began in her epigastrium and then migrated to the right upper quadrant. She also endorses episodes of nausea and vomiting. She describes having abdominal upset over the past several years, and notes particularly bothersome indigestion after eating greasy foods or when she eats too fast. She does endorse occasional reflux, although no worse than usual. Denies use of NSAIDs. She reports having an upper and lower endoscopy at an outside clinic about a year ago and was told that findings were normal. She denies undergoing any procedures, such as an ERCP, previously. Her liver enzymes and bilirubin are within normal limit.
CT scan of the abdomen/pelvis with contrast on admission noting marked thickening of the third portion of the duodenum and proximal jejunum, pneumobilia with a mildly distended common bile duct, probable small gallstones and mild gallbladder thickening, hepatic hemangioma, and enlarged fibrous uterus.
Decision was made to proceed with EGD.
Discussion: The patient was brought to the endoscopy unit and placed in the left lateral position for examination. The gastroscope was then advanced into the duodenum. Endoscopic findings were notable for diffuse edema of the second and third parts of the duodenum with narrowing of the lumen, and a foreign body (thyme root) was seen in the third part of the duodenum which was deeply impacted to the duodenal wall, causing a deep ulcer. The foreign body was gently removed with a forceps to the stomach, followed by Roth Net after applying a protective hood to the gastroscope. The small bowel mucosa beyond the edematous part was normal. The procedure was completed with withdrawal of the endoscope, no immediate post-procedural complications were observed. The patient was discharged 2 days after EGD with resolution of her symptoms and normalization of CT scan.
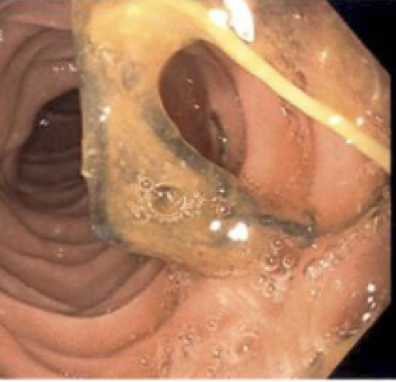
Figure: Thyme root embedded in duodenal wall
Disclosures:
Kaleb Lucas indicated no relevant financial relationships.
Agazi Gebreselassie indicated no relevant financial relationships.
Kaleb Lucas, MD1, Agazi Gebreselassie, MD2. P2020 - Unusual Cause of Intestinal Perforation and Pneumobilia from Thyme Root Ingestion with Successful Endoscopic Treatment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
