Sunday Poster Session
Category: Small Intestine
P2019 - Gas Under the Radar: Pneumatosis Intestinalis Without Ischemia in Crohn’s Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jalal Samhoun, MD
Florida Atlantic University Charles E. Schmidt College of Medicine
Boca Raton, FL
Presenting Author(s)
Jalal Samhoun, MD1, Charles Vallejo, DO1, Allison Chin, MD2, Hasan Ilyas, MD1, Zoilo K. Suarez, MD1, Todd Eisner, MD1
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL
Introduction: Pneumatosis intestinalis (PI) is the presence of gas in the bowel wall, classically an ominous radiographic sign of mesenteric ischemia or perforation. However, PI can also occur in benign conditions. It is a rare finding in inflammatory bowel disease (IBD). We present an 85-year-old man with long-standing Crohn’s disease (CD) on infliximab who developed small bowel PI mimicking a surgical abdomen but ultimately required no surgery.
Case Description/
Methods: An 85-year-old man with long-standing Crohn’s disease on infliximab underwent CT enterography for chronic weight loss, which revealed small-bowel PI. The patient had a long history of CD on infliximab and 18 months of unexplained weight loss. A computed tomography (CT) enterography revealed pneumatosis in the small intestine (Figure 1 & 2). Notably, a prior capsule endoscopy became retained at a jejunal stricture and was retrieved via double-balloon enteroscopy. On initial exam he was well-appearing, with stable vital signs, a soft non-tender abdomen, and normal serum lactate. In light of these benign findings and a recent Clostridioides difficile infection, a conservative non-operative approach was taken without antibiotics. Two weeks later, he returned with mild abdominal pain and fever. Repeat imaging showed persistent PI but no portal venous gas or other signs of ischemia. He improved with bowel rest, corticosteroids, and antibiotics, and was discharged without surgical intervention.
Discussion: This case illustrates that not all PI in Crohn’s disease indicates a need for emergent surgery. While PI often raises concern for bowel infarction requiring immediate operation, management should be individualized. Patients without peritoneal signs, hemodynamic instability, or metabolic acidosis can frequently be managed conservatively, consistent with reports of benign PI in CD managed non-operatively. Conversely, pneumatosis involving the small bowel combined with portal venous gas is a high-risk scenario associated with poor outcomes, often necessitating surgical intervention. In our patient, the absence of red flag signs justified watchful management, and his prompt improvement on steroids suggests an inflammatory rather than ischemic etiology for the pneumatosis. Even in an elderly, immunosuppressed Crohn’s patient, PI can radiographically mimic perforation, yet a cautious, evidence-guided approach may avert unnecessary surgery.
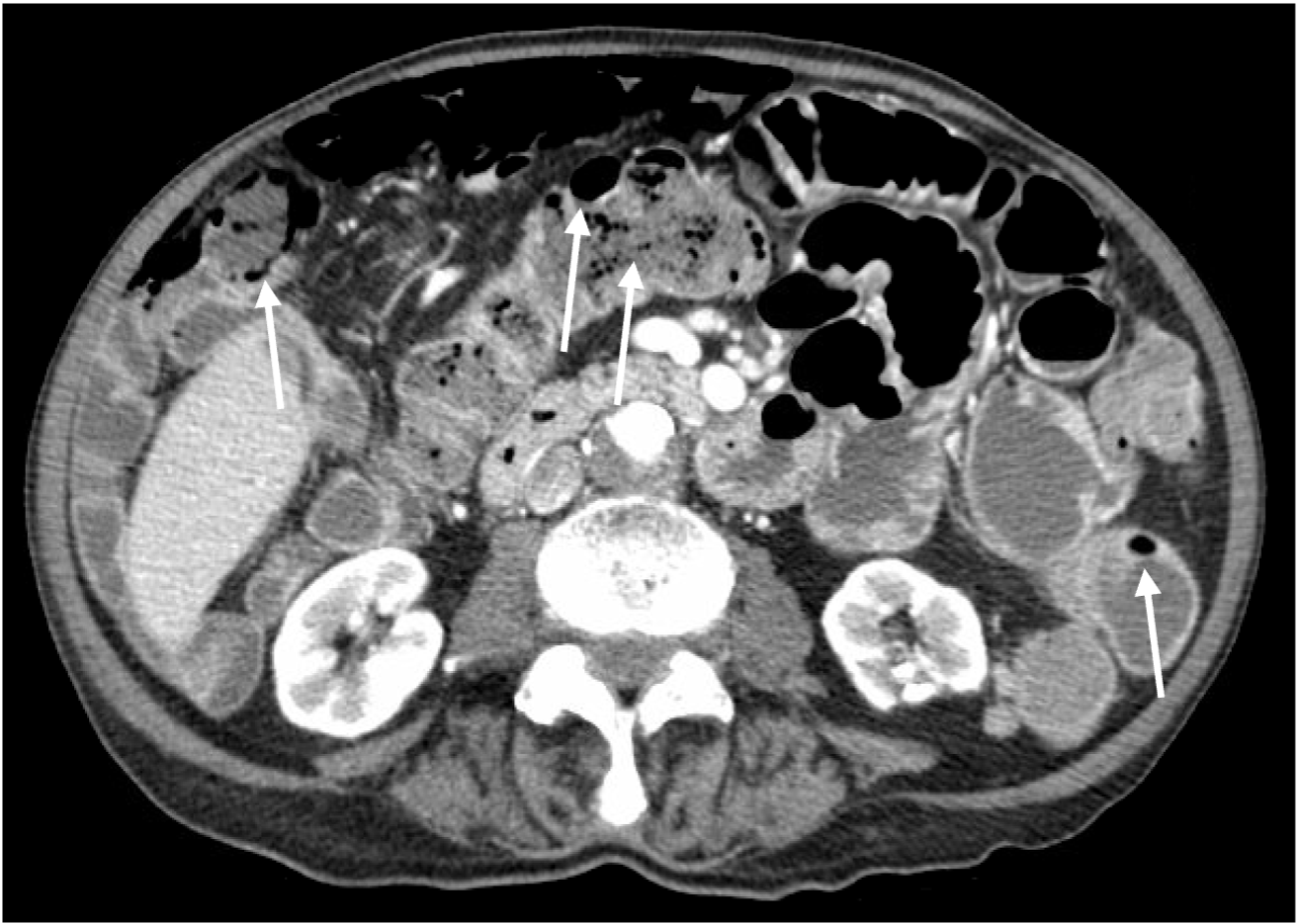
Figure: Figure 1. Coronal CT image demonstrating extensive pneumatosis intestinalis of the small bowel, characterized by multiple air-filled cystic lucencies within the bowel wall (white arrows). No portal venous gas or evidence of bowel ischemia is observed.
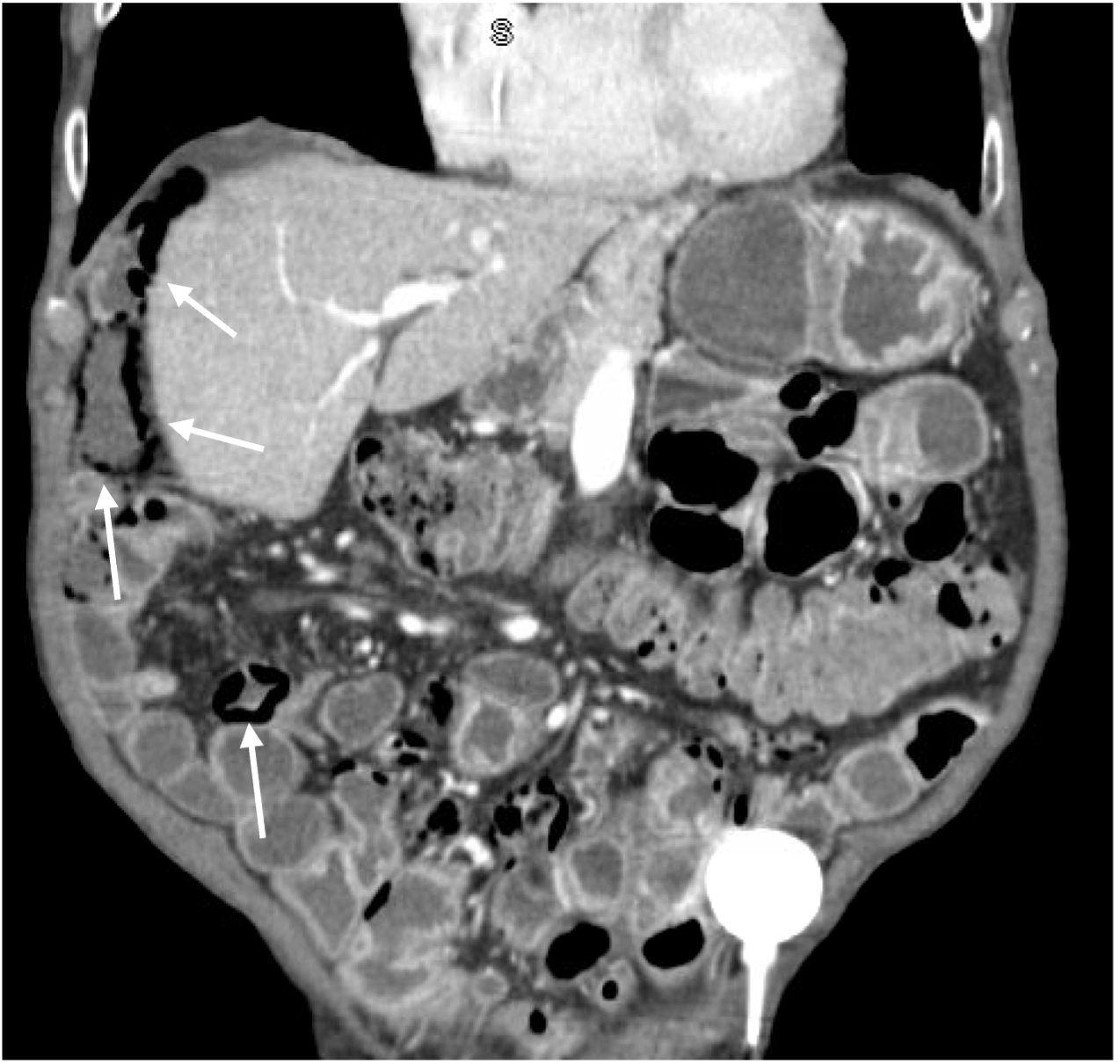
Figure: Figure 2. Axial CT scan highlighting extensive pneumatosis intestinalis of the small bowel, demonstrated by multiple air-filled cystic spaces within the bowel wall (white arrows). No portal venous gas or evidence of bowel ischemia is observed.
Disclosures:
Jalal Samhoun indicated no relevant financial relationships.
Charles Vallejo indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
Hasan Ilyas indicated no relevant financial relationships.
Zoilo Suarez indicated no relevant financial relationships.
Todd Eisner indicated no relevant financial relationships.
Jalal Samhoun, MD1, Charles Vallejo, DO1, Allison Chin, MD2, Hasan Ilyas, MD1, Zoilo K. Suarez, MD1, Todd Eisner, MD1. P2019 - Gas Under the Radar: Pneumatosis Intestinalis Without Ischemia in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL
Introduction: Pneumatosis intestinalis (PI) is the presence of gas in the bowel wall, classically an ominous radiographic sign of mesenteric ischemia or perforation. However, PI can also occur in benign conditions. It is a rare finding in inflammatory bowel disease (IBD). We present an 85-year-old man with long-standing Crohn’s disease (CD) on infliximab who developed small bowel PI mimicking a surgical abdomen but ultimately required no surgery.
Case Description/
Methods: An 85-year-old man with long-standing Crohn’s disease on infliximab underwent CT enterography for chronic weight loss, which revealed small-bowel PI. The patient had a long history of CD on infliximab and 18 months of unexplained weight loss. A computed tomography (CT) enterography revealed pneumatosis in the small intestine (Figure 1 & 2). Notably, a prior capsule endoscopy became retained at a jejunal stricture and was retrieved via double-balloon enteroscopy. On initial exam he was well-appearing, with stable vital signs, a soft non-tender abdomen, and normal serum lactate. In light of these benign findings and a recent Clostridioides difficile infection, a conservative non-operative approach was taken without antibiotics. Two weeks later, he returned with mild abdominal pain and fever. Repeat imaging showed persistent PI but no portal venous gas or other signs of ischemia. He improved with bowel rest, corticosteroids, and antibiotics, and was discharged without surgical intervention.
Discussion: This case illustrates that not all PI in Crohn’s disease indicates a need for emergent surgery. While PI often raises concern for bowel infarction requiring immediate operation, management should be individualized. Patients without peritoneal signs, hemodynamic instability, or metabolic acidosis can frequently be managed conservatively, consistent with reports of benign PI in CD managed non-operatively. Conversely, pneumatosis involving the small bowel combined with portal venous gas is a high-risk scenario associated with poor outcomes, often necessitating surgical intervention. In our patient, the absence of red flag signs justified watchful management, and his prompt improvement on steroids suggests an inflammatory rather than ischemic etiology for the pneumatosis. Even in an elderly, immunosuppressed Crohn’s patient, PI can radiographically mimic perforation, yet a cautious, evidence-guided approach may avert unnecessary surgery.
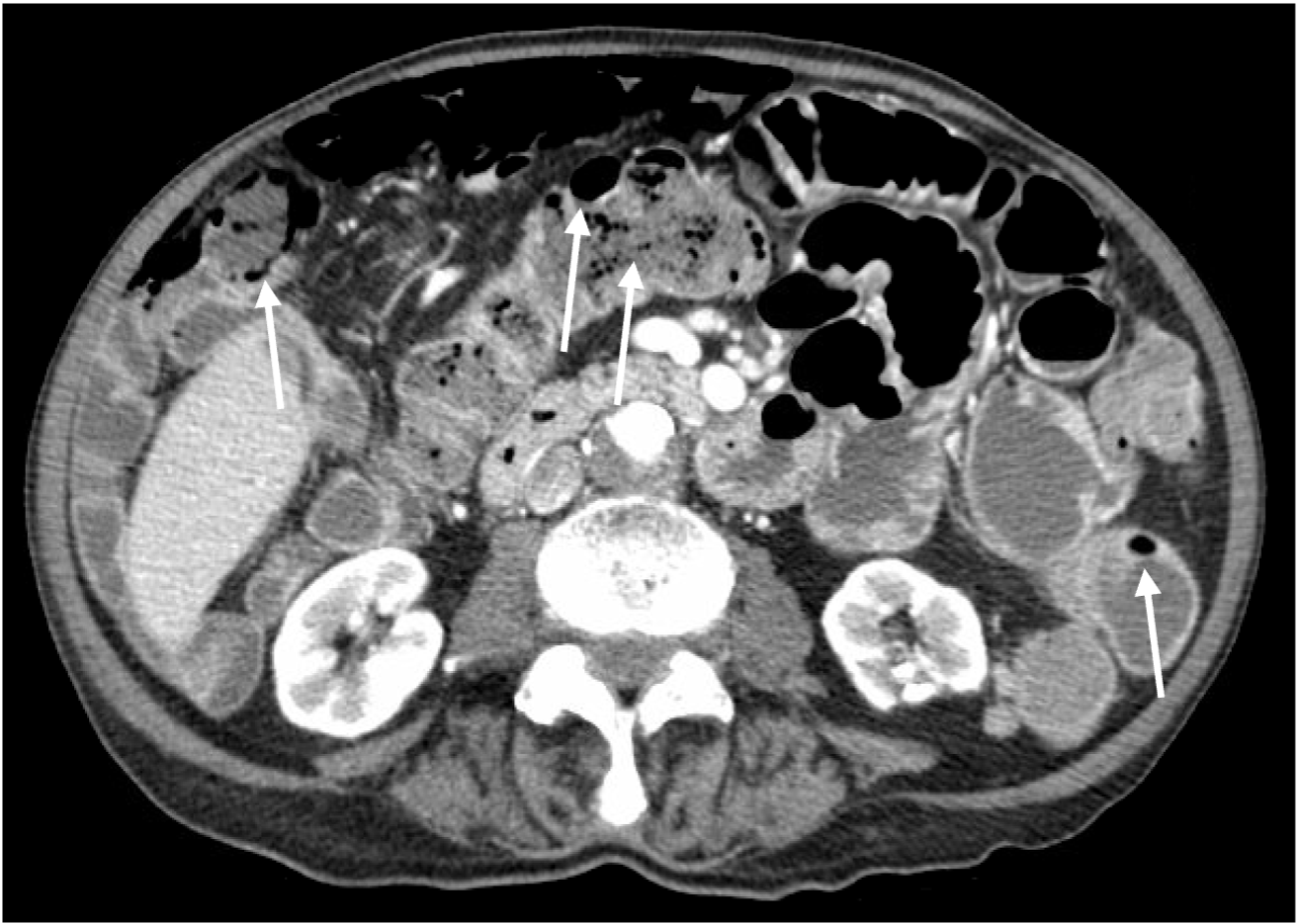
Figure: Figure 1. Coronal CT image demonstrating extensive pneumatosis intestinalis of the small bowel, characterized by multiple air-filled cystic lucencies within the bowel wall (white arrows). No portal venous gas or evidence of bowel ischemia is observed.
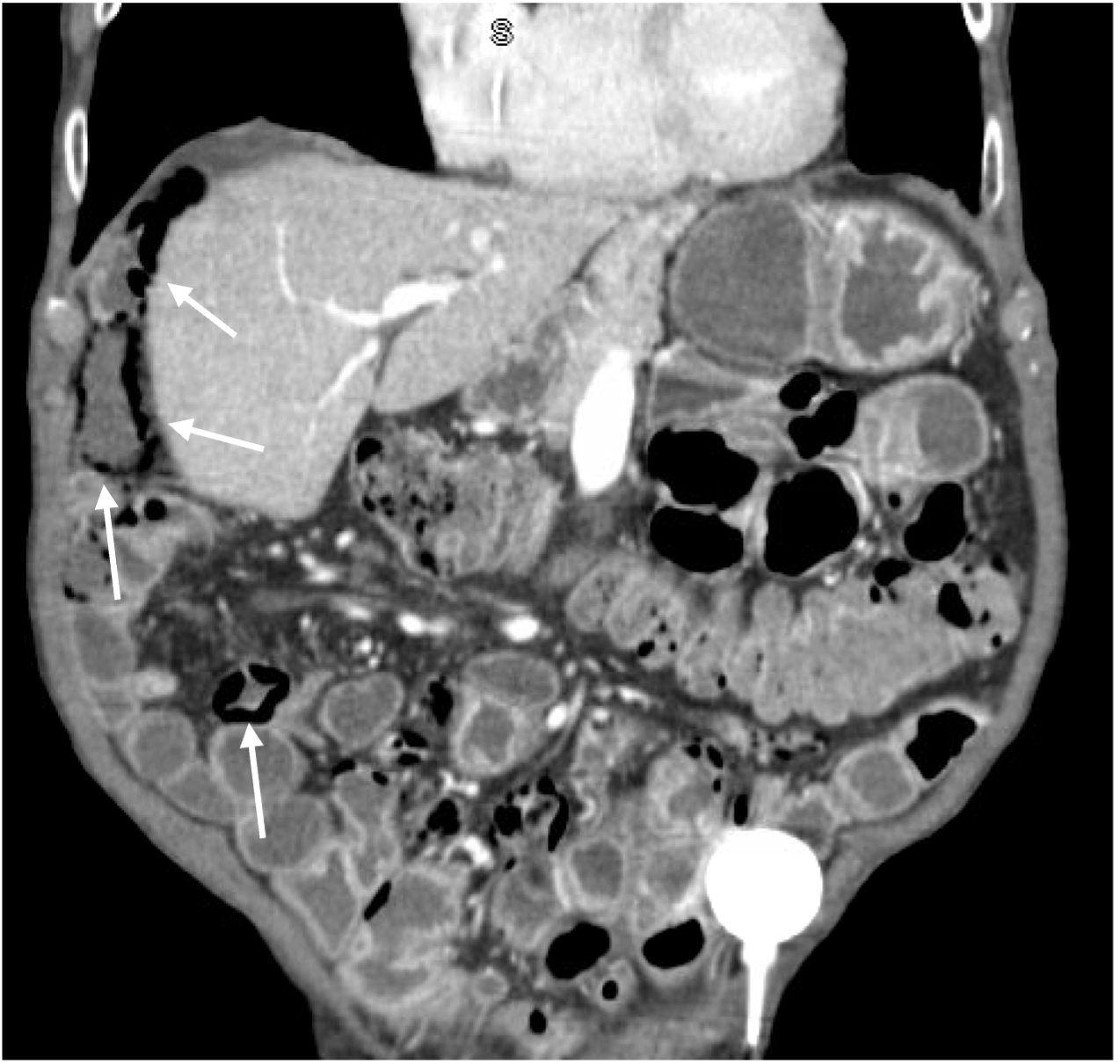
Figure: Figure 2. Axial CT scan highlighting extensive pneumatosis intestinalis of the small bowel, demonstrated by multiple air-filled cystic spaces within the bowel wall (white arrows). No portal venous gas or evidence of bowel ischemia is observed.
Disclosures:
Jalal Samhoun indicated no relevant financial relationships.
Charles Vallejo indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
Hasan Ilyas indicated no relevant financial relationships.
Zoilo Suarez indicated no relevant financial relationships.
Todd Eisner indicated no relevant financial relationships.
Jalal Samhoun, MD1, Charles Vallejo, DO1, Allison Chin, MD2, Hasan Ilyas, MD1, Zoilo K. Suarez, MD1, Todd Eisner, MD1. P2019 - Gas Under the Radar: Pneumatosis Intestinalis Without Ischemia in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
