Sunday Poster Session
Category: Small Intestine
P2010 - A Rare Case of Giant Duodenal Polyp
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD, Eric Zhao, MD, Juan Sigala Lozano, MD, Waldemar Niklinski, MD, Vikram Kotwal, MD
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Brunner’s gland adenomas (BGAs) are rare benign duodenal tumors arising from submucosal Brunner’s glands, which secrete alkaline mucus for mucosal protection. Most BGAs are small and asymptomatic, but larger lesions ( >2 cm) may cause gastrointestinal bleeding or anemia. We report a case of a giant BGA presenting with melena and severe iron deficiency anemia, managed successfully with endoscopic resection.
Case Description/
Methods: A 52-year-old man with hyperlipidemia presented with exertional dyspnea and melena for one month. He denied NSAID or anticoagulant use. Labs showed microcytic anemia (hemoglobin 5.3 g/dL, ferritin 4 ng/mL, transferrin saturation 6.5%). After receiving three units of packed red blood cells and IV pantoprazole, hemoglobin rose to 8.0 g/dL. Esophagogastroduodenoscopy revealed mild gastric erosions and a large, 5 cm pedunculated polyp in the second portion of the duodenum. Patient underwent subsequent endoscopy for polyp removal, where 3 mL of epinephrine (1:10,000) was injected into the polyp base. Hemostasis was secured with four hemoclips, followed by snare cautery polypectomy. Due to the polyp’s large size, retrieval through the pylorus required use of a 4-wire stone extraction basket. Further resistance at the upper esophageal sphincter necessitated overtube-assisted extraction. Histopathology confirmed Brunner’s gland adenoma with lobulated nests of bland Brunner’s glands separated by fibrous septa. Gastric biopsies were positive for Helicobacter pylori and treated with concomitant therapy. At follow-up, the patient reported full resolution of symptoms, and hemoglobin improved to 11.1 g/dL.
Discussion: This case illustrates that large BGAs can cause occult GI bleeding and iron deficiency anemia. Due to their submucosal origin, superficial biopsies may be non-diagnostic, requiring complete resection for definitive diagnosis. Endoscopic management is a safe, minimally invasive alternative to surgery, even for large lesions, when appropriate hemostatic techniques and retrieval strategies are used. Though the link between H. pylori and BGAs remains speculative, co-detection may warrant eradication. Long-term outcomes following resection are excellent, with low recurrence and no proven malignant potential.
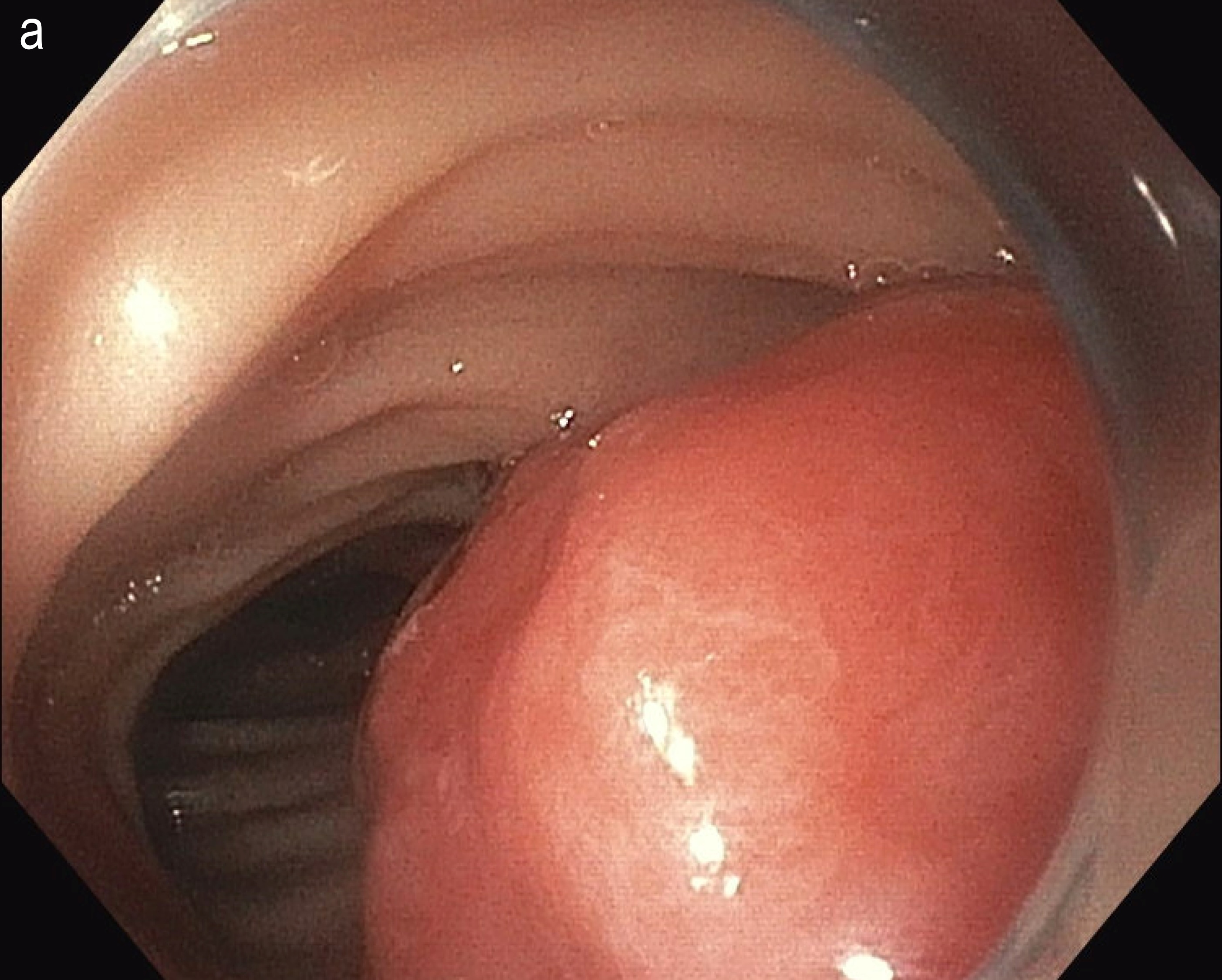
Figure: Figure 1. Duodenal polyp on upper endoscopy
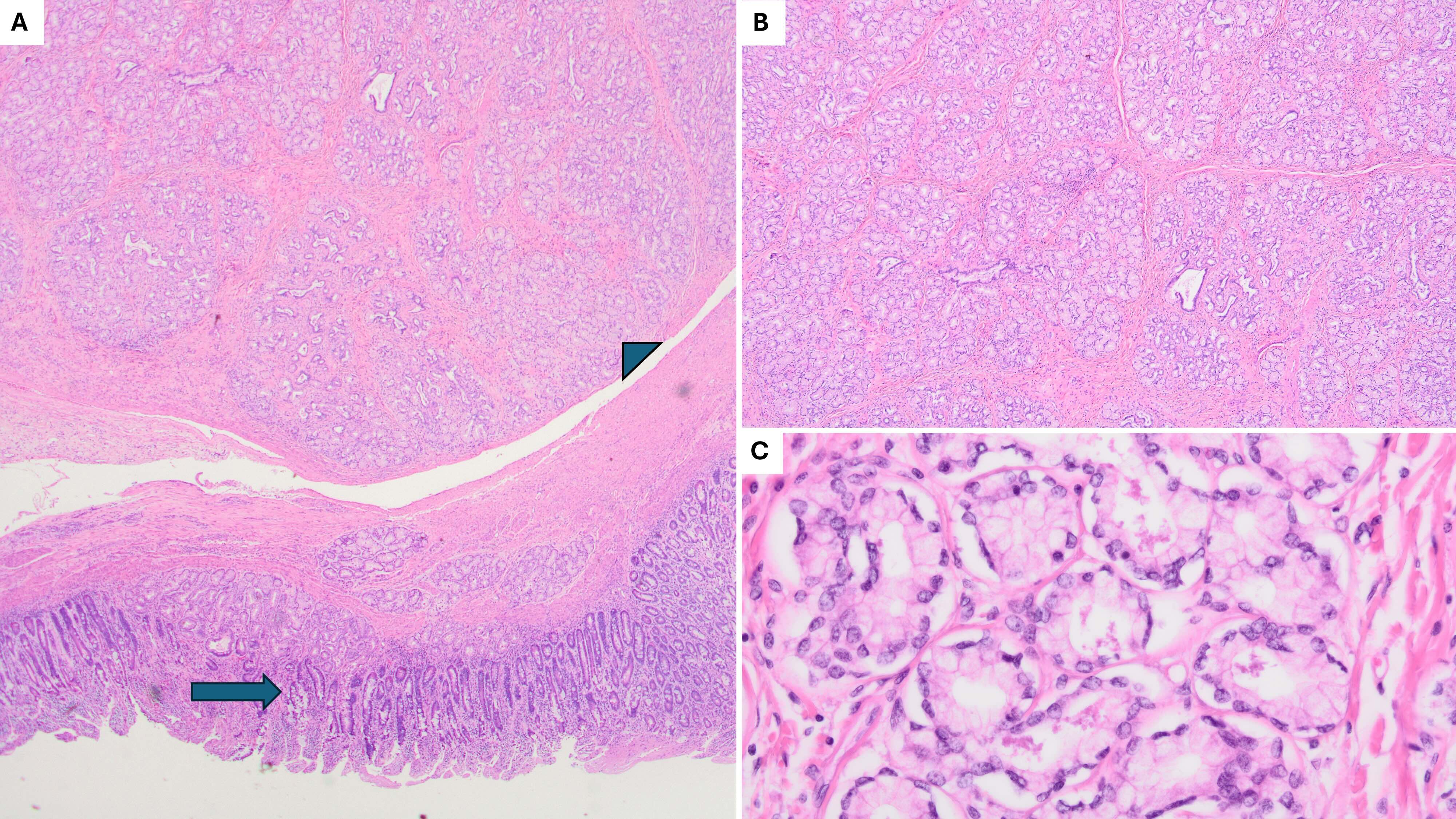
Figure: Figure 2. Brunner gland adenoma on histopathology: (A) 40x H&E stain showing unremarkable intestinal mucosa (arrow) and submucosa expanded by nodules of Brunner’s glands (arrowhead), (B) 200x H&E stain showing Brunner’s glands in lobulated nests, separated by thin fibrous bands and smooth muscle, (C) 400x H&E stain showing Brunner’s glands with cuboidal cells with round to flat basal nuclei and foamy cytoplasm and minimal intervening stroma. H&E, hematoxylin and eosin.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Eric Zhao indicated no relevant financial relationships.
Juan Sigala Lozano indicated no relevant financial relationships.
Waldemar Niklinski indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Abhin Sapkota, MD, Eric Zhao, MD, Juan Sigala Lozano, MD, Waldemar Niklinski, MD, Vikram Kotwal, MD. P2010 - A Rare Case of Giant Duodenal Polyp, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Brunner’s gland adenomas (BGAs) are rare benign duodenal tumors arising from submucosal Brunner’s glands, which secrete alkaline mucus for mucosal protection. Most BGAs are small and asymptomatic, but larger lesions ( >2 cm) may cause gastrointestinal bleeding or anemia. We report a case of a giant BGA presenting with melena and severe iron deficiency anemia, managed successfully with endoscopic resection.
Case Description/
Methods: A 52-year-old man with hyperlipidemia presented with exertional dyspnea and melena for one month. He denied NSAID or anticoagulant use. Labs showed microcytic anemia (hemoglobin 5.3 g/dL, ferritin 4 ng/mL, transferrin saturation 6.5%). After receiving three units of packed red blood cells and IV pantoprazole, hemoglobin rose to 8.0 g/dL. Esophagogastroduodenoscopy revealed mild gastric erosions and a large, 5 cm pedunculated polyp in the second portion of the duodenum. Patient underwent subsequent endoscopy for polyp removal, where 3 mL of epinephrine (1:10,000) was injected into the polyp base. Hemostasis was secured with four hemoclips, followed by snare cautery polypectomy. Due to the polyp’s large size, retrieval through the pylorus required use of a 4-wire stone extraction basket. Further resistance at the upper esophageal sphincter necessitated overtube-assisted extraction. Histopathology confirmed Brunner’s gland adenoma with lobulated nests of bland Brunner’s glands separated by fibrous septa. Gastric biopsies were positive for Helicobacter pylori and treated with concomitant therapy. At follow-up, the patient reported full resolution of symptoms, and hemoglobin improved to 11.1 g/dL.
Discussion: This case illustrates that large BGAs can cause occult GI bleeding and iron deficiency anemia. Due to their submucosal origin, superficial biopsies may be non-diagnostic, requiring complete resection for definitive diagnosis. Endoscopic management is a safe, minimally invasive alternative to surgery, even for large lesions, when appropriate hemostatic techniques and retrieval strategies are used. Though the link between H. pylori and BGAs remains speculative, co-detection may warrant eradication. Long-term outcomes following resection are excellent, with low recurrence and no proven malignant potential.
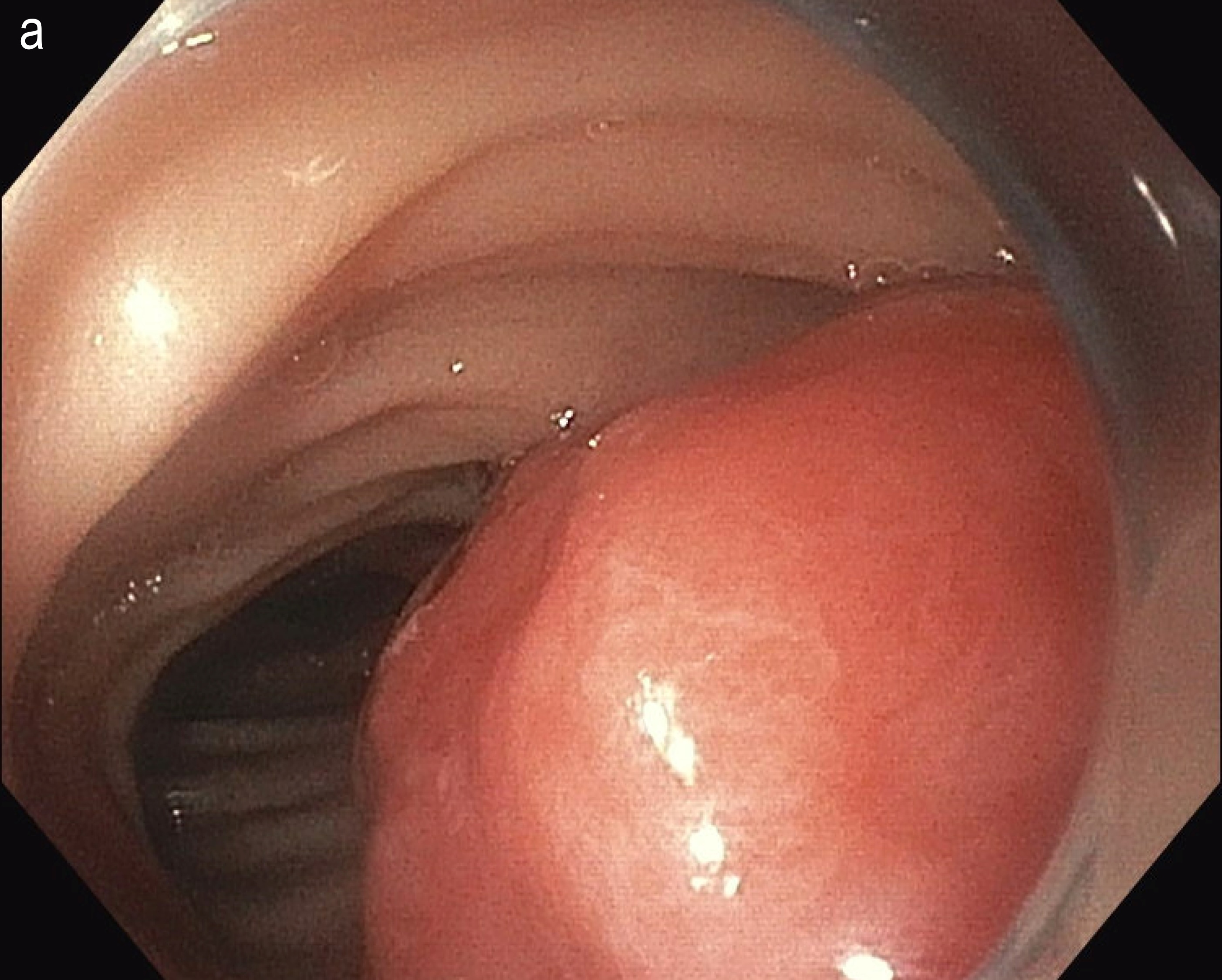
Figure: Figure 1. Duodenal polyp on upper endoscopy
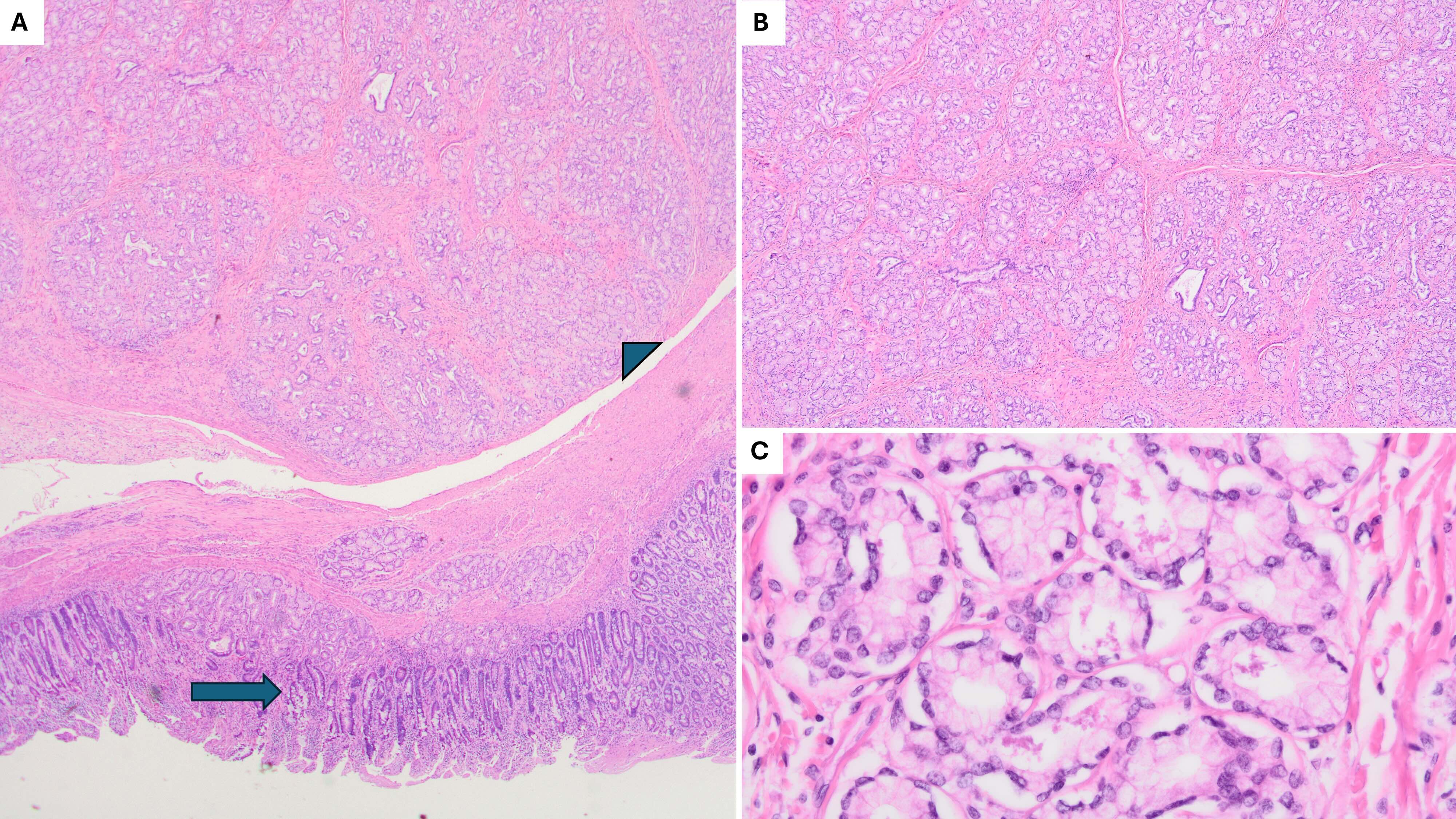
Figure: Figure 2. Brunner gland adenoma on histopathology: (A) 40x H&E stain showing unremarkable intestinal mucosa (arrow) and submucosa expanded by nodules of Brunner’s glands (arrowhead), (B) 200x H&E stain showing Brunner’s glands in lobulated nests, separated by thin fibrous bands and smooth muscle, (C) 400x H&E stain showing Brunner’s glands with cuboidal cells with round to flat basal nuclei and foamy cytoplasm and minimal intervening stroma. H&E, hematoxylin and eosin.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Eric Zhao indicated no relevant financial relationships.
Juan Sigala Lozano indicated no relevant financial relationships.
Waldemar Niklinski indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Abhin Sapkota, MD, Eric Zhao, MD, Juan Sigala Lozano, MD, Waldemar Niklinski, MD, Vikram Kotwal, MD. P2010 - A Rare Case of Giant Duodenal Polyp, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
