Sunday Poster Session
Category: Stomach and Spleen
P2096 - Gastric Mucosal Hyperplasia in the Setting of Long-Term Proton Pump Inhibitor Use Mimicking Submucosal Tumor
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Bolla, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Rishi Bolla, MD1, Prasad Kulkarni, MD, FACG2, Jeffrey Gill, MD2, Jennifer Reed, MD2, Alexander Somwaru, MD2, Martin Zloty, MD2, Robert Lucaj, MD2, Wojciech Blonski, MD, PhD, FACG2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Long-term proton pump inhibitor (PPI) use has been known to cause various changes in the gastric mucosa, including hypertrophy. The mechanism of these changes is not fully understood; however, they are mostly considered benign. Here we present a case in which a patient with long-term PPI use was found to have thickened gastric mucosa resembling a submucosal tumor.
Case Description/
Methods: A 72-year-old male with history of long segment non-dysplastic Barrett’s esophagus (BE) and long-term PPI use ( >15 years) presented with a two-week history of nausea, vomiting, abdominal pain, and diarrhea. He had surveillance esophagogastroduodenoscopy (EGD) four years ago which showed BE without dysplasia. Computed tomography (CT) showed mass-like thickening of the fundus of the stomach with a hypertrophied blood vessel. EGD revealed C2M4 non-dysplastic BE, a 3cm hiatal hernia, and a submucosal mass in the fundus. Follow up endoscopic ultrasound (EUS) showed a dilated mucosa up to 20mm, but no vascular abnormality and no submucosal or muscularis propria abnormality. Biopsy revealed benign gastric tissue with negative immunohistochemical stain for Helicobacter pylori. A diagnosis of Menetrier’s disease was considered. Therefore, a repeat EGD was performed and 2 large pieces of the lesion were removed via endoscopic mucosal resection. Pathology revealed benign oxyntic gastric mucosa with gland hyperplasia, which seems to suggest long-term PPI use as the cause. The patient finally underwent positron emission tomography-CT (PET-CT) one month later which revealed no worrisome hypermetabolic activity within the thickened folds at the gastric fundus or in the rest of the stomach. No hypermetabolic foci concerning for malignancy were found throughout the remainder of the body either. His symptoms eventually subsided.
Discussion: The patient’s chief complaint along with the CT findings lead to multiple EGD and EUS evaluations of the ultimately benign gastric mucosal hypertrophy, followed by a normal PET-CT. It was this unique combination of factors that resulted in such a thorough workup, and it underscores the latent effects of PPIs, a class of medications that are so commonly used.
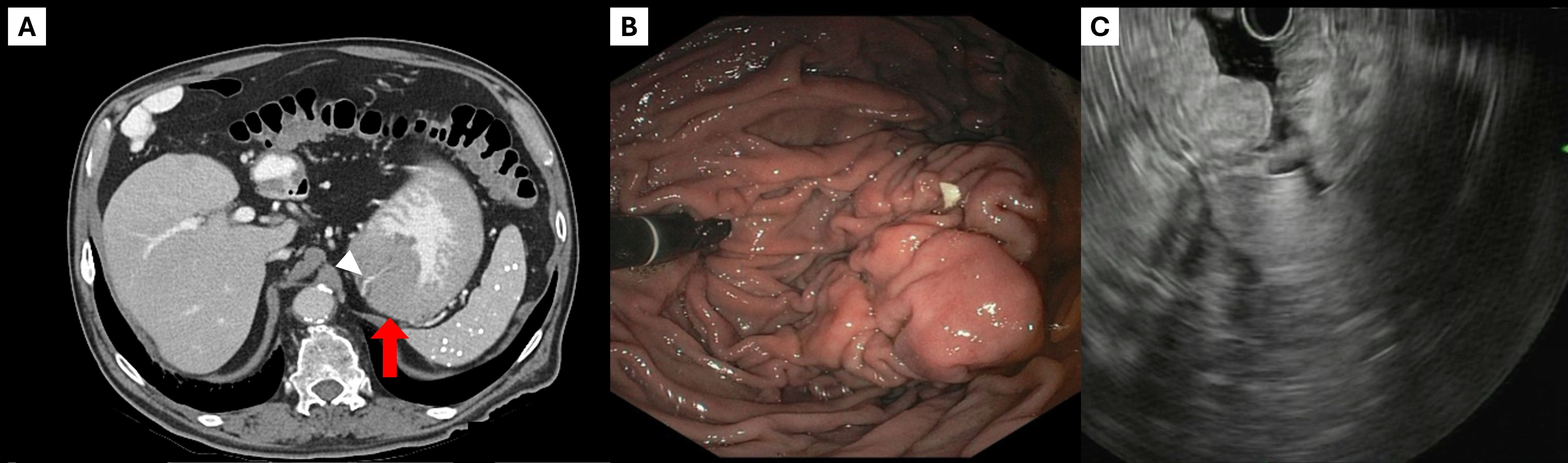
Figure: Figure 1: A) Contrast-enhanced axial CT image showing mass-like thickening in the gastric fundus (arrow). B) EGD retroflexion shows mass concerning for submucosal tumor. C) EUS image showing thickened gastric mucosa without vascularity or submucosal abnormality.
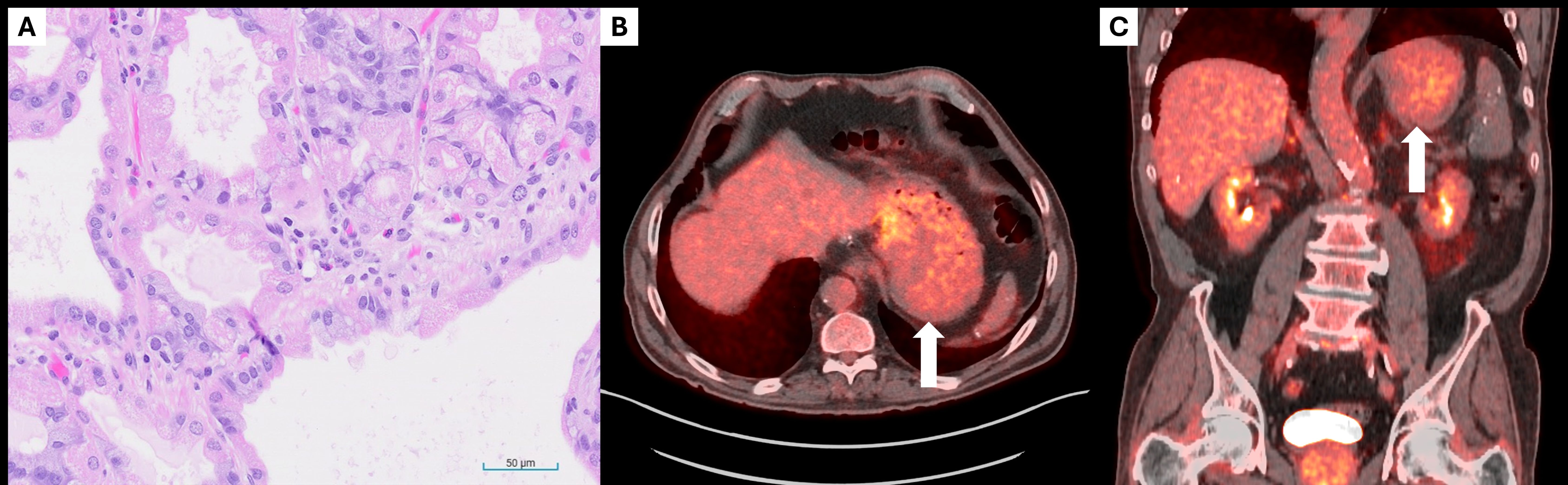
Figure: Figure 2: A) Biopsy sections showing dilated oxyntic glands lined by parietal, chief and mucinous cells. The foveolar compartment is relatively normal. B) Axial PET-CT image and C) coronal PET-CT image showing physiologic activity corresponding to prominent gastric folds (arrows). No worrisome focal activity within gastric fundus.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Prasad Kulkarni indicated no relevant financial relationships.
Jeffrey Gill indicated no relevant financial relationships.
Jennifer Reed indicated no relevant financial relationships.
Alexander Somwaru indicated no relevant financial relationships.
Martin Zloty indicated no relevant financial relationships.
Robert Lucaj indicated no relevant financial relationships.
Wojciech Blonski indicated no relevant financial relationships.
Rishi Bolla, MD1, Prasad Kulkarni, MD, FACG2, Jeffrey Gill, MD2, Jennifer Reed, MD2, Alexander Somwaru, MD2, Martin Zloty, MD2, Robert Lucaj, MD2, Wojciech Blonski, MD, PhD, FACG2. P2096 - Gastric Mucosal Hyperplasia in the Setting of Long-Term Proton Pump Inhibitor Use Mimicking Submucosal Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Long-term proton pump inhibitor (PPI) use has been known to cause various changes in the gastric mucosa, including hypertrophy. The mechanism of these changes is not fully understood; however, they are mostly considered benign. Here we present a case in which a patient with long-term PPI use was found to have thickened gastric mucosa resembling a submucosal tumor.
Case Description/
Methods: A 72-year-old male with history of long segment non-dysplastic Barrett’s esophagus (BE) and long-term PPI use ( >15 years) presented with a two-week history of nausea, vomiting, abdominal pain, and diarrhea. He had surveillance esophagogastroduodenoscopy (EGD) four years ago which showed BE without dysplasia. Computed tomography (CT) showed mass-like thickening of the fundus of the stomach with a hypertrophied blood vessel. EGD revealed C2M4 non-dysplastic BE, a 3cm hiatal hernia, and a submucosal mass in the fundus. Follow up endoscopic ultrasound (EUS) showed a dilated mucosa up to 20mm, but no vascular abnormality and no submucosal or muscularis propria abnormality. Biopsy revealed benign gastric tissue with negative immunohistochemical stain for Helicobacter pylori. A diagnosis of Menetrier’s disease was considered. Therefore, a repeat EGD was performed and 2 large pieces of the lesion were removed via endoscopic mucosal resection. Pathology revealed benign oxyntic gastric mucosa with gland hyperplasia, which seems to suggest long-term PPI use as the cause. The patient finally underwent positron emission tomography-CT (PET-CT) one month later which revealed no worrisome hypermetabolic activity within the thickened folds at the gastric fundus or in the rest of the stomach. No hypermetabolic foci concerning for malignancy were found throughout the remainder of the body either. His symptoms eventually subsided.
Discussion: The patient’s chief complaint along with the CT findings lead to multiple EGD and EUS evaluations of the ultimately benign gastric mucosal hypertrophy, followed by a normal PET-CT. It was this unique combination of factors that resulted in such a thorough workup, and it underscores the latent effects of PPIs, a class of medications that are so commonly used.
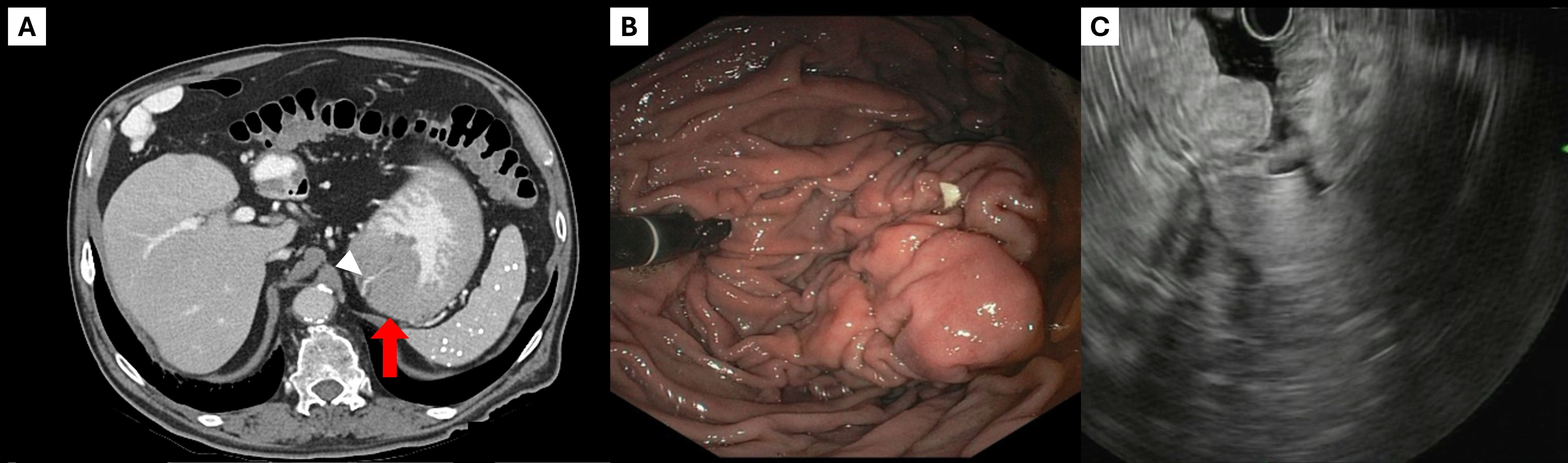
Figure: Figure 1: A) Contrast-enhanced axial CT image showing mass-like thickening in the gastric fundus (arrow). B) EGD retroflexion shows mass concerning for submucosal tumor. C) EUS image showing thickened gastric mucosa without vascularity or submucosal abnormality.
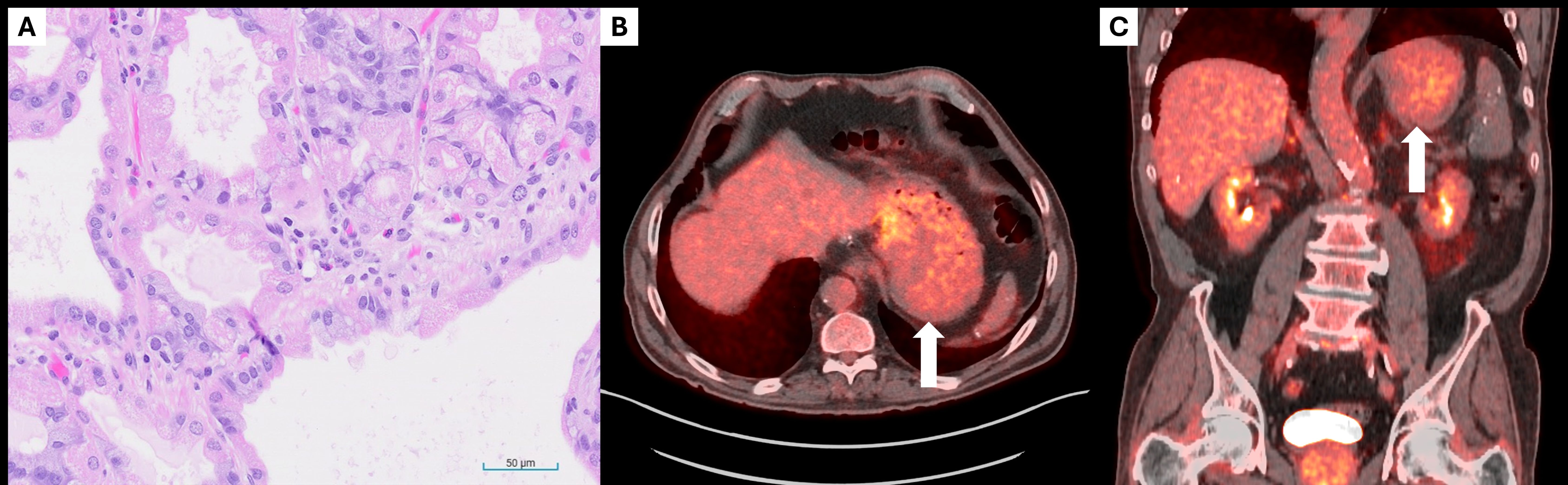
Figure: Figure 2: A) Biopsy sections showing dilated oxyntic glands lined by parietal, chief and mucinous cells. The foveolar compartment is relatively normal. B) Axial PET-CT image and C) coronal PET-CT image showing physiologic activity corresponding to prominent gastric folds (arrows). No worrisome focal activity within gastric fundus.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Prasad Kulkarni indicated no relevant financial relationships.
Jeffrey Gill indicated no relevant financial relationships.
Jennifer Reed indicated no relevant financial relationships.
Alexander Somwaru indicated no relevant financial relationships.
Martin Zloty indicated no relevant financial relationships.
Robert Lucaj indicated no relevant financial relationships.
Wojciech Blonski indicated no relevant financial relationships.
Rishi Bolla, MD1, Prasad Kulkarni, MD, FACG2, Jeffrey Gill, MD2, Jennifer Reed, MD2, Alexander Somwaru, MD2, Martin Zloty, MD2, Robert Lucaj, MD2, Wojciech Blonski, MD, PhD, FACG2. P2096 - Gastric Mucosal Hyperplasia in the Setting of Long-Term Proton Pump Inhibitor Use Mimicking Submucosal Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
