Monday Poster Session
Category: Biliary/Pancreas
P2224 - Early or Late? Timing of Intervention in Acute Biliary Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Ramandeep Sandhu, MD1, Wael Youssef, MD1, Dalbir S. Sandhu, MD3
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3St. Joseph's Hospital and Medical Center, Phoenix, AZ
Introduction: Acute biliary pancreatitis (ABP) is a leading cause of acute pancreatitis, arising from gallstones. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) are two primary interventional strategies. This study aims to evaluate and compare the timings of ERCP and LCBDE in the management of ABP.
Methods: Data were obtained from the Nationwide Readmissions Database, from 2016 to 2021 with total cost adjusted to 2021 dollars. Patients were categorized by timing into urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP or LCBDE.
Results: The analysis included 67,738 admissions, patients undergoing LCBDE were younger (mean age 53.8 ± 0.08 vs. 63.7 ± 0.18 years; p< 0.001) and more frequently female (62.9% vs. 53.8%; p< 0.001). Clinical outcomes favored LCBDE over ERCP, with shorter length of stay (LOS) (4.65 ± 0.017 vs. 6.36 ± 0.081 days; p< 0.001), lower 30-day readmission rates (6.56% vs. 14.5%; odds ratio (OR): 0.54, 95% confidence interval (CI): 0.50–0.59; p< 0.001), and 38% reduced mortality during readmission (OR: 0.62, 95% CI: 0.41–0.95; p=0.026). LCBDE also resulted in fewer complications, including sepsis, septic shock, respiratory failure, and kidney failure (p< 0.001).
Timing of ERCP was critical, with late ERCP associated with higher complication rates, such as septic shock (2.11%) and severe sepsis (0.77%). Adjusted analyses showed late ERCP resulted in a 3.32-day longer LOS compared to no ERCP (p< 0.001) and a 67% higher likelihood of 30-day readmission (OR: 1.67, 95% CI: 1.40–1.99; p< 0.001).
Similarly, late LCBDE was associated with the longest LOS (6.33 ± 0.028 days) and the highest complication rates. Adjusted analyses indicated that late LCBDE significantly increased LOS and costs (p< 0.001). Early LCBDE was associated with 21% lower odds of readmission compared to urgent LCBDE (p=0.002), with both early and urgent procedures showing reduced odds of readmission compared to no LCBDE (p< 0.001).
Discussion: LCBDE was associated with more favorable outcomes, including shorter length of stay, lower rates of complications, reduced 30-day readmission rates, and decreased odds of death during readmission compared to ERCP. The timing of both ERCP and LCBDE played a critical role in patient outcomes, with earlier procedures consistently associated with reduced complications, lower healthcare costs, shorter hospital stays, and decreased readmission rates.
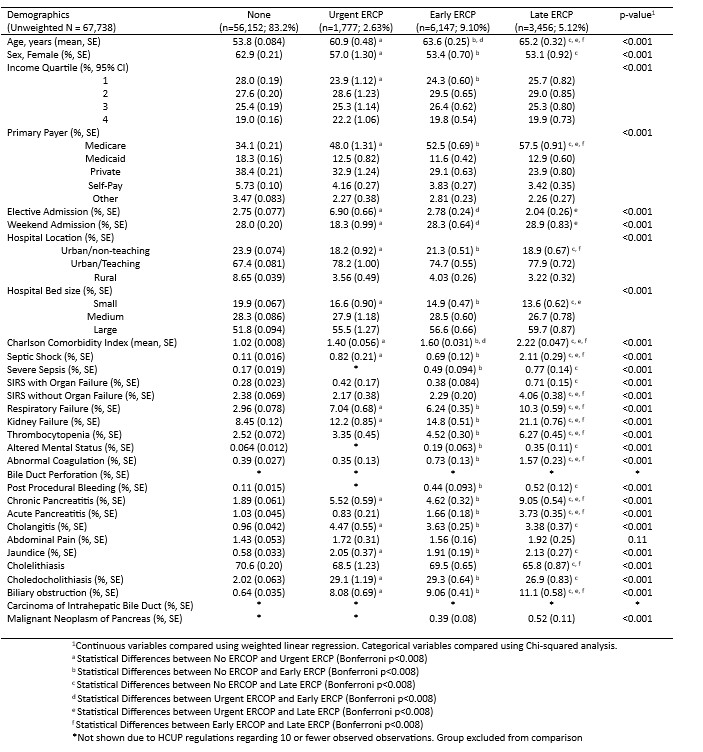
Figure: Table 1: Demographics and clinical characteristics by ERCP Timing
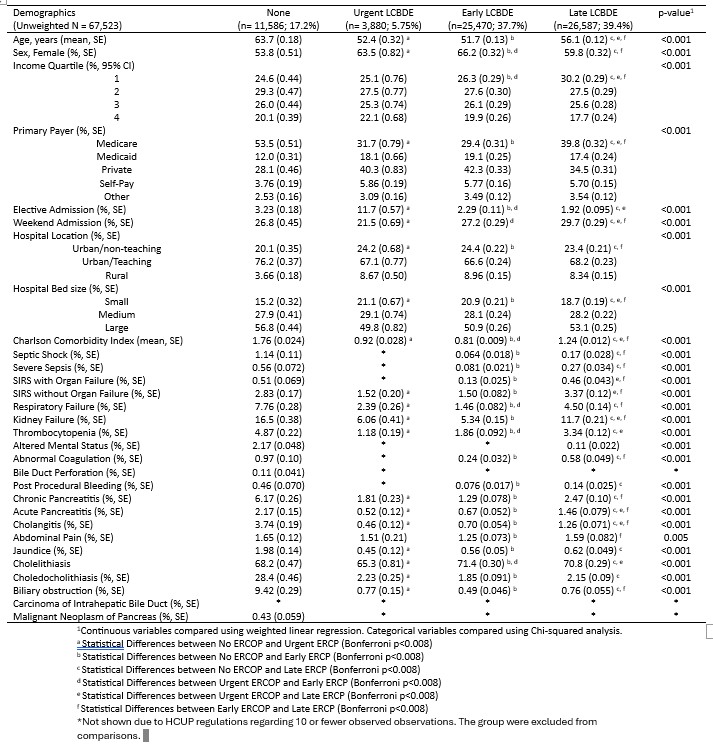
Figure: Table 2: Demographics and clinical characteristics by LCBDE Timing
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Sunanda Ellina indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Ramandeep Sandhu, MD1, Wael Youssef, MD1, Dalbir S. Sandhu, MD3. P2224 - Early or Late? Timing of Intervention in Acute Biliary Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3St. Joseph's Hospital and Medical Center, Phoenix, AZ
Introduction: Acute biliary pancreatitis (ABP) is a leading cause of acute pancreatitis, arising from gallstones. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) are two primary interventional strategies. This study aims to evaluate and compare the timings of ERCP and LCBDE in the management of ABP.
Methods: Data were obtained from the Nationwide Readmissions Database, from 2016 to 2021 with total cost adjusted to 2021 dollars. Patients were categorized by timing into urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP or LCBDE.
Results: The analysis included 67,738 admissions, patients undergoing LCBDE were younger (mean age 53.8 ± 0.08 vs. 63.7 ± 0.18 years; p< 0.001) and more frequently female (62.9% vs. 53.8%; p< 0.001). Clinical outcomes favored LCBDE over ERCP, with shorter length of stay (LOS) (4.65 ± 0.017 vs. 6.36 ± 0.081 days; p< 0.001), lower 30-day readmission rates (6.56% vs. 14.5%; odds ratio (OR): 0.54, 95% confidence interval (CI): 0.50–0.59; p< 0.001), and 38% reduced mortality during readmission (OR: 0.62, 95% CI: 0.41–0.95; p=0.026). LCBDE also resulted in fewer complications, including sepsis, septic shock, respiratory failure, and kidney failure (p< 0.001).
Timing of ERCP was critical, with late ERCP associated with higher complication rates, such as septic shock (2.11%) and severe sepsis (0.77%). Adjusted analyses showed late ERCP resulted in a 3.32-day longer LOS compared to no ERCP (p< 0.001) and a 67% higher likelihood of 30-day readmission (OR: 1.67, 95% CI: 1.40–1.99; p< 0.001).
Similarly, late LCBDE was associated with the longest LOS (6.33 ± 0.028 days) and the highest complication rates. Adjusted analyses indicated that late LCBDE significantly increased LOS and costs (p< 0.001). Early LCBDE was associated with 21% lower odds of readmission compared to urgent LCBDE (p=0.002), with both early and urgent procedures showing reduced odds of readmission compared to no LCBDE (p< 0.001).
Discussion: LCBDE was associated with more favorable outcomes, including shorter length of stay, lower rates of complications, reduced 30-day readmission rates, and decreased odds of death during readmission compared to ERCP. The timing of both ERCP and LCBDE played a critical role in patient outcomes, with earlier procedures consistently associated with reduced complications, lower healthcare costs, shorter hospital stays, and decreased readmission rates.
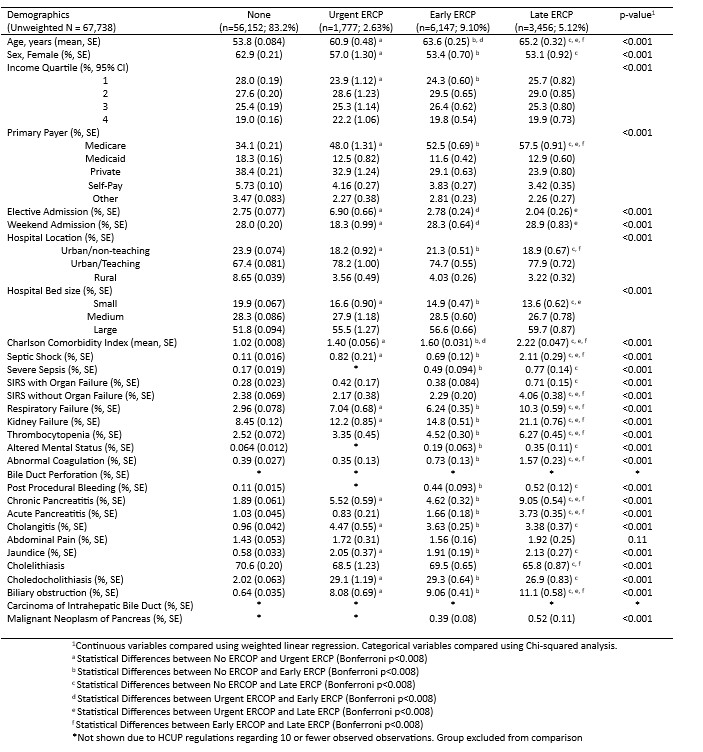
Figure: Table 1: Demographics and clinical characteristics by ERCP Timing
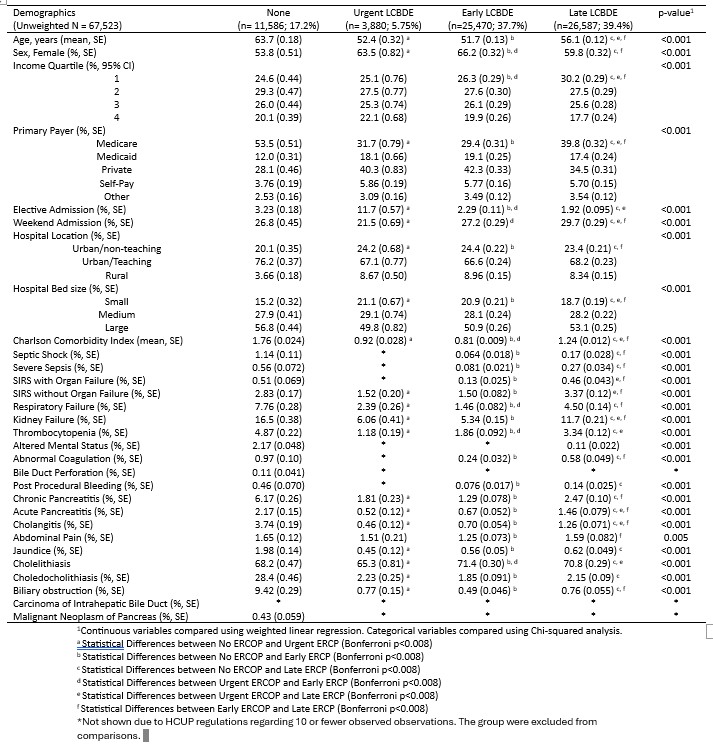
Figure: Table 2: Demographics and clinical characteristics by LCBDE Timing
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Sunanda Ellina indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Ramandeep Sandhu, MD1, Wael Youssef, MD1, Dalbir S. Sandhu, MD3. P2224 - Early or Late? Timing of Intervention in Acute Biliary Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
