Monday Poster Session
Category: Biliary/Pancreas
P2178 - Drug-Induced Acute Pancreatitis Has a More Favorable Course Than Biliary Acute Pancreatitis: Findings From Analysis of the National Inpatient Sample
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamed Karam Douedari, MD
Mount Sinai Medical Center
Miami Beach, FL
Presenting Author(s)
Mohamed Karam Douedari, MD1, Jodie A. Barkin, MD, FACG2, Mahmoud Mahfouz, MD2, Rama Tarakji, MD, MPH1, Neil Chokshi, DO1
1Mount Sinai Medical Center, Miami Beach, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Acute pancreatitis (AP) is the third leading cause of gastrointestinal hospitalization in the U.S., with drug-induced AP (DIAP) representing a rare (0.1–2%) but clinically important subset, often diagnosed by exclusion. Delayed recognition may lead to recurrent injury and suboptimal care. Large-scale national studies on DIAP are limited. This study examines the characteristics, disparities, and outcomes of DIAP admissions compared to biliary AP.
Methods: We conducted a retrospective cohort study using the 2019–2022 National Inpatient Sample. Adult admissions with a primary diagnosis of AP were identified by ICD-10-CM codes, with DIAP and biliary AP defined accordingly. We excluded chronic pancreatitis and records with missing data. The primary outcome was to compare demographics, characteristics, and disparities between DIAP and biliary AP, with the latter serving as the reference standard for AP. Secondary outcomes included mortality, complications, length of stay, and hospital charges. Multivariable regression adjusted for demographics, comorbidities, hospital, and socioeconomic factors (Table 1).
Results: Among 1,030,954 adult AP admissions, 15,869 were DIAP cases. Compared to biliary AP, DIAP patients were less likely Hispanic, and had higher rates of diabetes, hyperlipidemia, and greater comorbidity burden (Table 1). In multivariable adjusted analyses, DIAP was associated with lower in-hospital mortality (aOR 0.58, p=0.049). DIAP had lower odds of necrotizing AP (aOR 0.69, p=0.001), respiratory failure (aOR 0.74, p=0.004), and shock (aOR 0.60, p=0.024), but higher odds of paralytic ileus (aOR 2.05, p=0.036). No difference was seen in AKI. DIAP was associated with shorter stays and lower charges (Figure 1a–c).
Discussion: In this large national inpatient cohort, DIAP accounted for 1.5% of AP admissions and was more common in non-Hispanic patients and those with greater comorbidities compared to biliary AP. Despite the higher comorbidity burden, DIAP admissions had lower mortality and significantly fewer complications, with shorter hospital stays and significantly reduced charges, suggesting a more favorable overall course than biliary AP. These findings may help clinicians identify distinct features of DIAP, monitor for specific complications, and influence clinical course and management. Ultimately, early identification of DIAP as the etiology is crucial to prevent repeated pancreatic injury and further morbidity and mortality.
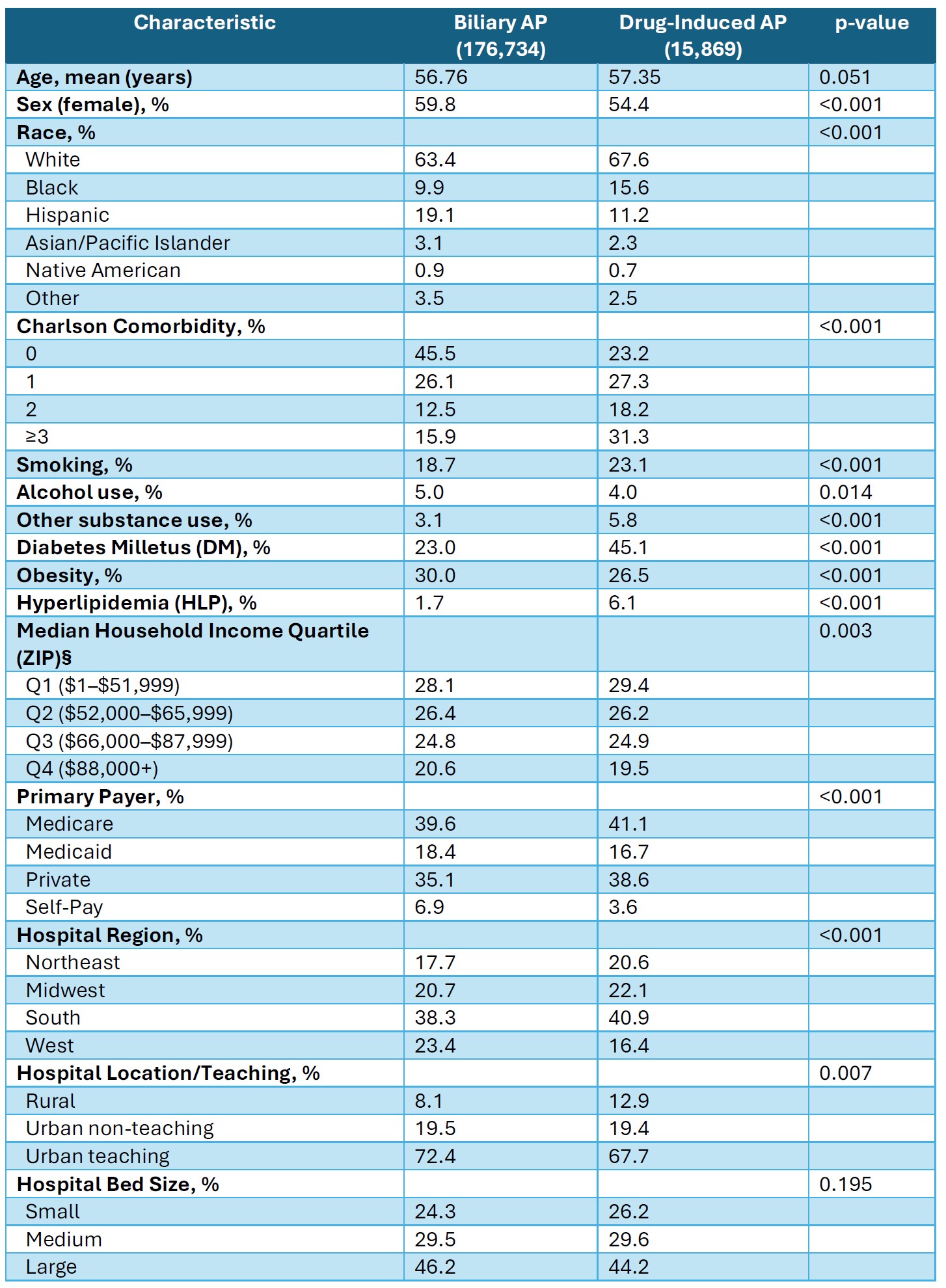
Figure: Table 1: Baseline Characteristics of Adult Pancreatitis Admissions by etiology: Drug-Induced vs. Biliary

Figure: Figure 1: Adjusted Odds Ratios for Mortality and Complications (a), Mean Length of Stay (b), and Mean Total Hospital Charges (c) in DIAP vs. Biliary AP.
Disclosures:
Mohamed Karam Douedari indicated no relevant financial relationships.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Mahmoud Mahfouz indicated no relevant financial relationships.
Rama Tarakji indicated no relevant financial relationships.
Neil Chokshi indicated no relevant financial relationships.
Mohamed Karam Douedari, MD1, Jodie A. Barkin, MD, FACG2, Mahmoud Mahfouz, MD2, Rama Tarakji, MD, MPH1, Neil Chokshi, DO1. P2178 - Drug-Induced Acute Pancreatitis Has a More Favorable Course Than Biliary Acute Pancreatitis: Findings From Analysis of the National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai Medical Center, Miami Beach, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Acute pancreatitis (AP) is the third leading cause of gastrointestinal hospitalization in the U.S., with drug-induced AP (DIAP) representing a rare (0.1–2%) but clinically important subset, often diagnosed by exclusion. Delayed recognition may lead to recurrent injury and suboptimal care. Large-scale national studies on DIAP are limited. This study examines the characteristics, disparities, and outcomes of DIAP admissions compared to biliary AP.
Methods: We conducted a retrospective cohort study using the 2019–2022 National Inpatient Sample. Adult admissions with a primary diagnosis of AP were identified by ICD-10-CM codes, with DIAP and biliary AP defined accordingly. We excluded chronic pancreatitis and records with missing data. The primary outcome was to compare demographics, characteristics, and disparities between DIAP and biliary AP, with the latter serving as the reference standard for AP. Secondary outcomes included mortality, complications, length of stay, and hospital charges. Multivariable regression adjusted for demographics, comorbidities, hospital, and socioeconomic factors (Table 1).
Results: Among 1,030,954 adult AP admissions, 15,869 were DIAP cases. Compared to biliary AP, DIAP patients were less likely Hispanic, and had higher rates of diabetes, hyperlipidemia, and greater comorbidity burden (Table 1). In multivariable adjusted analyses, DIAP was associated with lower in-hospital mortality (aOR 0.58, p=0.049). DIAP had lower odds of necrotizing AP (aOR 0.69, p=0.001), respiratory failure (aOR 0.74, p=0.004), and shock (aOR 0.60, p=0.024), but higher odds of paralytic ileus (aOR 2.05, p=0.036). No difference was seen in AKI. DIAP was associated with shorter stays and lower charges (Figure 1a–c).
Discussion: In this large national inpatient cohort, DIAP accounted for 1.5% of AP admissions and was more common in non-Hispanic patients and those with greater comorbidities compared to biliary AP. Despite the higher comorbidity burden, DIAP admissions had lower mortality and significantly fewer complications, with shorter hospital stays and significantly reduced charges, suggesting a more favorable overall course than biliary AP. These findings may help clinicians identify distinct features of DIAP, monitor for specific complications, and influence clinical course and management. Ultimately, early identification of DIAP as the etiology is crucial to prevent repeated pancreatic injury and further morbidity and mortality.
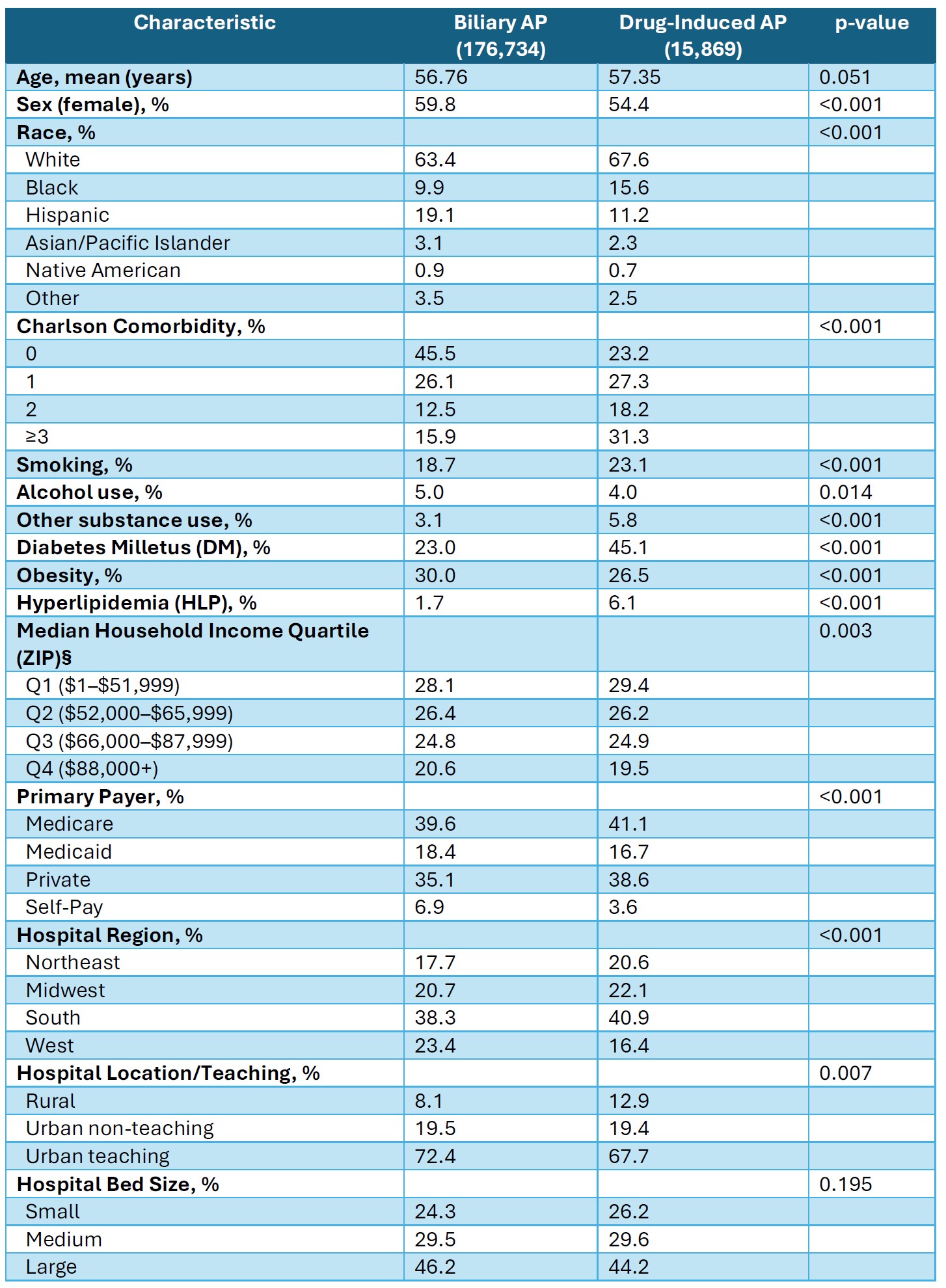
Figure: Table 1: Baseline Characteristics of Adult Pancreatitis Admissions by etiology: Drug-Induced vs. Biliary

Figure: Figure 1: Adjusted Odds Ratios for Mortality and Complications (a), Mean Length of Stay (b), and Mean Total Hospital Charges (c) in DIAP vs. Biliary AP.
Disclosures:
Mohamed Karam Douedari indicated no relevant financial relationships.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Mahmoud Mahfouz indicated no relevant financial relationships.
Rama Tarakji indicated no relevant financial relationships.
Neil Chokshi indicated no relevant financial relationships.
Mohamed Karam Douedari, MD1, Jodie A. Barkin, MD, FACG2, Mahmoud Mahfouz, MD2, Rama Tarakji, MD, MPH1, Neil Chokshi, DO1. P2178 - Drug-Induced Acute Pancreatitis Has a More Favorable Course Than Biliary Acute Pancreatitis: Findings From Analysis of the National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

