Monday Poster Session
Category: Colon
P2430 - Comparative Efficacy of Precut Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Colorectal Polyps: A Systematic Review and Meta-Analysis

Aamir Saeed, MD
Vanderbilt University Medical Center
Memphis, TN
Presenting Author(s)
Award: ACG Presidential Poster Award
Aamir Saeed, MD1, Saira Yousuf, MD1, Marjan Haider, MD2, Ghulam Ali Hasnan, MBBS3, Hina Akbar, MD4, Sachit Sharma, MD5, Umar Hayat, MD6, Umer Farooq, MD7, Manesh Gangwani, MD8, Muhammad Hashim Hayat, MD9, Zohaib Ahmed, MD10, Muhammad Aziz, MBBS11, Mark Radlinski, MD1, Faisal Kamal, MD12
1Vanderbilt University Medical Center, Nashville, TN; 2Trinity Health Ann Arbor Hospital, Ypsilanti, MI; 3Dr Grays Hospital NHS Grampian, Elgin, Scotland, United Kingdom; 4King Edward Medical University, Chattanooga, TN; 5Richmond Gastroenterology Associates, Richmond, VA; 6Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 7Saint Louis University, Saint Louis, MO; 8University of Arkansas for Medical Sciences, Little Rock, AR; 9Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 10University of Toledo College Medicine and Life Sciences, Toledo, OH; 11Bon Secours Mercy Health, Toledo, OH; 12Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction:
Endoscopic submucosal dissection (ESD) is effective in the management of large colorectal polyps. However, ESD is technically demanding and time consuming. Precut EMR (EMR-P) is a modified EMR method that overcomes some of the limitations of EMR. It involves creating a circumferential mucosal incision around the lesion before resection. We conducted a meta-analysis to compare the outcomes of EMR-P with ESD in the management of colorectal polyps.
Methods:
Several databases were reviewed to identify studies comparing outcomes of EMR-P and ESD for colorectal polyps from inception to November 08, 2024. The databases searched included PubMed, Web of Science Core Collection, Embase, and the Cochrane Database of Systematic Reviews. Our outcomes of interest were en bloc resection, complete resection, local recurrence, delayed perforation, delayed bleeding, and procedure time. Subgroup analysis were performed for ≥20mm polyps. We calculated risk ratios (RRs) with 95% confidence intervals (CIs) for all categorical variables and mean differences with 95% CI for continuous variables. Data was analyzed using random effect model. Heterogeneity was assessed using the I2 statistic. Publication bias was assessed by funnel plots and Egger’s test.
Results:
Four studies comprising 870 patients (289 patients in EMR-P and 581 in ESD groups) met the
inclusion criteria. We found no significant difference in rates of en bloc resection, RR (95% CI): 0.72 (0.46, 1.11), p=0.13 (Figure 1A), complete resection RR (95% CI): 0.85 (0.66, 1.11), p=0.23 (Figure 1B) and local recurrence, RR (95% CI): 1.21 (0.07, 21.85), p=0.90 (Figure 2A) between groups. There was no significant difference in rate of adverse events between groups such as, delayed bleeding, RR (95% CI): 0.82 (0.21, 3.10), p=0.76 and delayed perforation RR (95% CI): 0.78 (0.24, 2.54), p=0.69. EMR-P was associated with shorter procedure time compared to ESD, MD (95% CI): -27.47 (-31.61, -23.33), p< 0.00001 (Figure 2B). Subgroup analysis for ≥20mm polyps also showed no significant difference in rates of en bloc resection RR (95% CI): 0.73 (0.42, 1.27), p=0.27, delayed bleeding, RR (95% CI): 0.99 (0.13, 7.42), p=0.99, and delayed perforation RR (95% CI): 0.49(0.20, 1.21), p=0.12 between groups.
Discussion:
Our meta-analysis found that, the outcomes of EMR-P were comparable to ESD for colorectal polyps, except procedure time which was shorter with EMR-P. Future large, multicentre studies are required to further evaluate these findings. 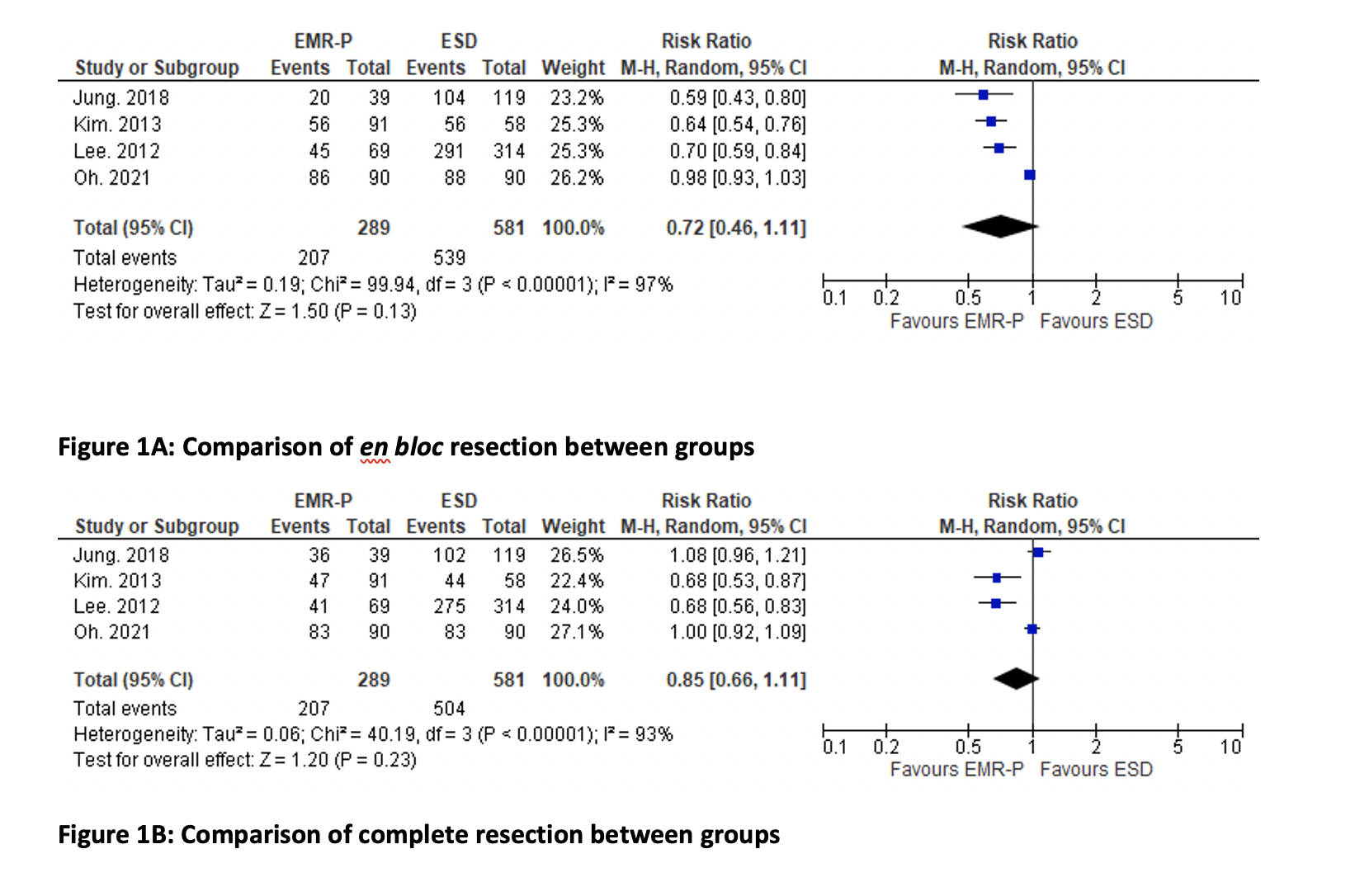
Figure: Comparison of en bloc resection and complete resection between groups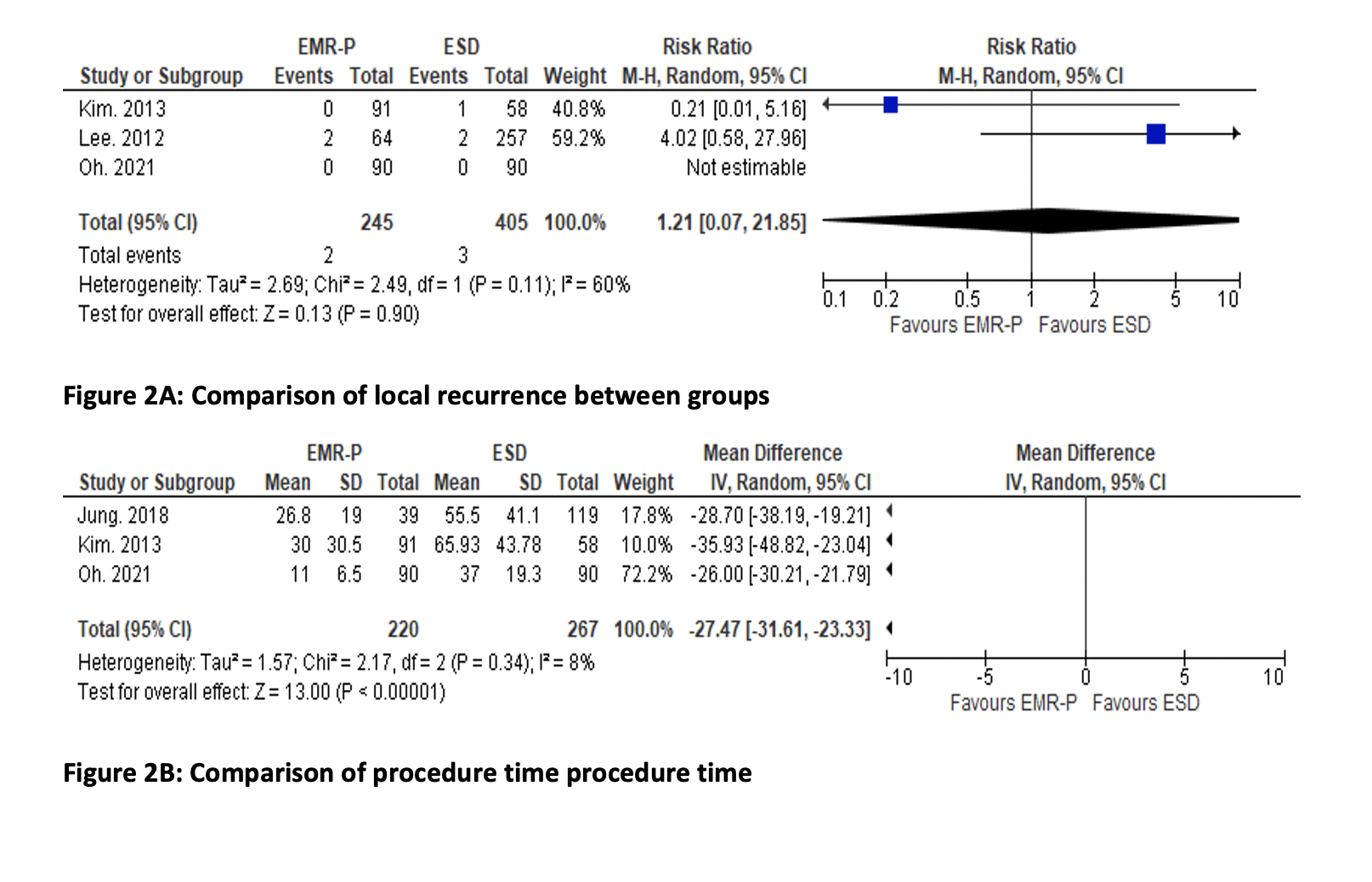
Figure: Comparison of local recurrence and procedure time between groups
Disclosures:
Aamir Saeed indicated no relevant financial relationships.
Saira Yousuf indicated no relevant financial relationships.
Marjan Haider indicated no relevant financial relationships.
Ghulam Ali Hasnan indicated no relevant financial relationships.
Hina Akbar indicated no relevant financial relationships.
Sachit Sharma indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Manesh Gangwani indicated no relevant financial relationships.
Muhammad Hashim Hayat indicated no relevant financial relationships.
Zohaib Ahmed indicated no relevant financial relationships.
Muhammad Aziz indicated no relevant financial relationships.
Mark Radlinski indicated no relevant financial relationships.
Faisal Kamal indicated no relevant financial relationships.
Aamir Saeed, MD1, Saira Yousuf, MD1, Marjan Haider, MD2, Ghulam Ali Hasnan, MBBS3, Hina Akbar, MD4, Sachit Sharma, MD5, Umar Hayat, MD6, Umer Farooq, MD7, Manesh Gangwani, MD8, Muhammad Hashim Hayat, MD9, Zohaib Ahmed, MD10, Muhammad Aziz, MBBS11, Mark Radlinski, MD1, Faisal Kamal, MD12. P2430 - Comparative Efficacy of Precut Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Colorectal Polyps: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

