Monday Poster Session
Category: Colon
P2420 - Lactulose vs Polyethylene Glycol for Colonoscopy Bowel Preparation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Emre Bardak, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Ali Emre Bardak, MD1, Gizem Teker, MD2, Mehmed Taha Dinc, MD3, Narisara Tribuddharat, MD1, Okan Cetin, MD2, Bilger Cavus, MD2
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2Istanbul University, Istanbul, Istanbul, Turkey; 3Boston Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Effective colonoscopy depends on successful bowel preparation. Polyethylene glycol (PEG) solutions are the standard regimens, but they are often poorly tolerated due to their taste and large volume. Lactulose, an osmotic laxative primarily used to treat constipation, has emerged as a more palatable, lower-volume alternative for bowel preparation. Studies to date comparing these two regimens have yielded variable and sometimes conflicting results. In this systematic review and meta-analysis, we aimed to compare lactulose- and PEG-based regimens in terms of bowel cleansing efficacy and adverse events.
Methods: We conducted a systematic literature search in PubMed, Embase, and Cochrane databases through May 2025 to identify randomized controlled trials (RCTs) comparing lactulose- and PEG-based bowel preparation regimens for colonoscopy in adults that reported at least one outcome of interest. The primary outcome was the bowel cleansing efficacy; secondary outcomes were polyp detection rate and adverse events. The mean difference (MD) and risk ratio (RR) were used as effect measures for continuous and dichotomous outcomes, respectively. Pooled analyses were performed using random-effects models.
Results: Six RCTs encompassing 1,447 patients (54.2% female; mean age 51.7 years) were included. Baseline characteristics were similar between the two regimens across all studies. Adequate bowel preparation rates were similar between the lactulose and PEG groups (RR 1.01, 95% CI 0.97–1.06). Lactulose was associated with modestly higher total Boston Bowel Preparation Scale (BBPS) scores (MD 0.48, 95% CI 0.03–0.92, Figure 1) and transverse colon BBPS scores (MD 0.11, 95% CI 0.04–0.24), whereas differences in right colon (MD 0.25, 95% CI -0.01–0.52) and left colon BBPS scores (MD 0.02, 95% CI -0.30–0.34) did not reach statistical significance. Polyp detection rates did not differ significantly (RR 1.11, 95% CI 0.81–1.51). Adverse event rates, including nausea or vomiting (RR 0.79, 95% CI 0.33–1.89), abdominal bloating (RR 0.33, 95% CI 0.05–2.22), and abdominal pain (RR 0.90, 95% CI 0.11–7.46), were also comparable. Details of the pooled outcomes are presented in Figure 2.
Discussion: Lactulose demonstrated comparable efficacy to PEG in achieving adequate bowel preparation, with slightly higher overall and segmental BBPS scores in some regions. Polyp detection and adverse event rates were similar between the two regimens. These findings suggest that lactulose may serve as an alternative to PEG.
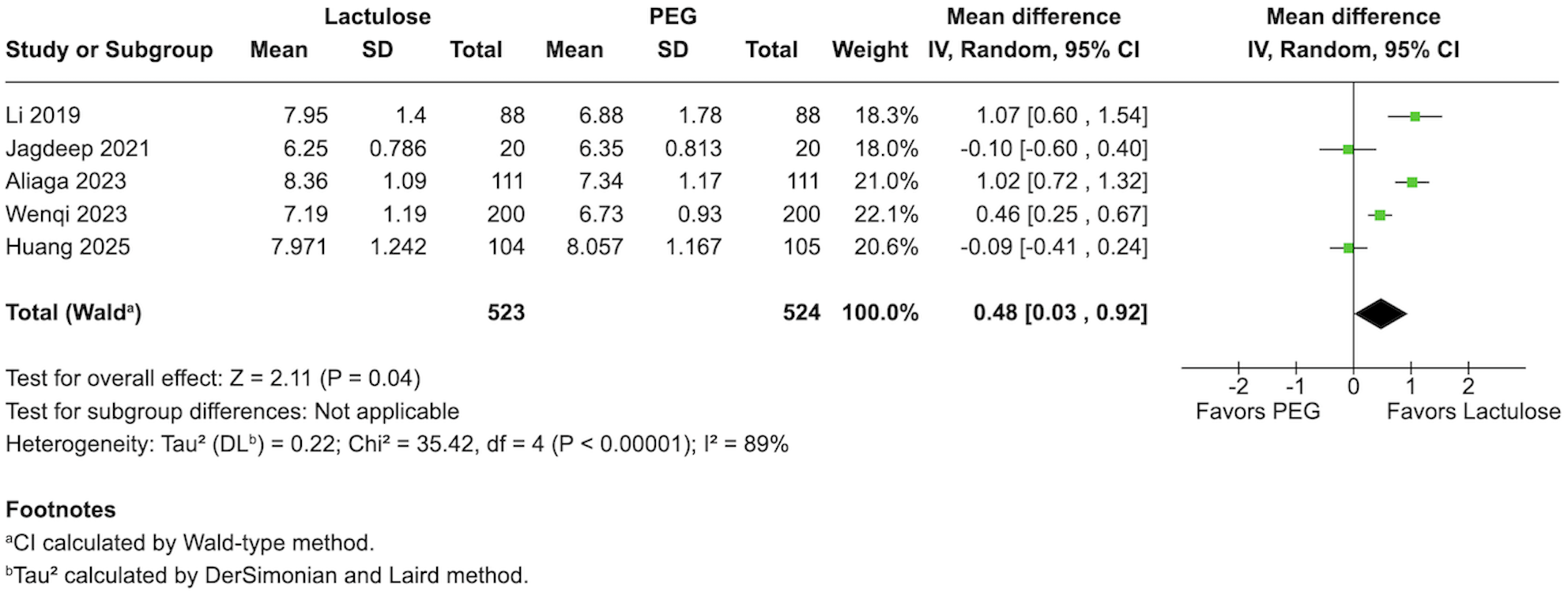
Figure: Figure 1: Forest plot of total Boston Bowel Preparation Scale (BBPS) scores comparing lactulose versus polyethylene glycol (PEG).
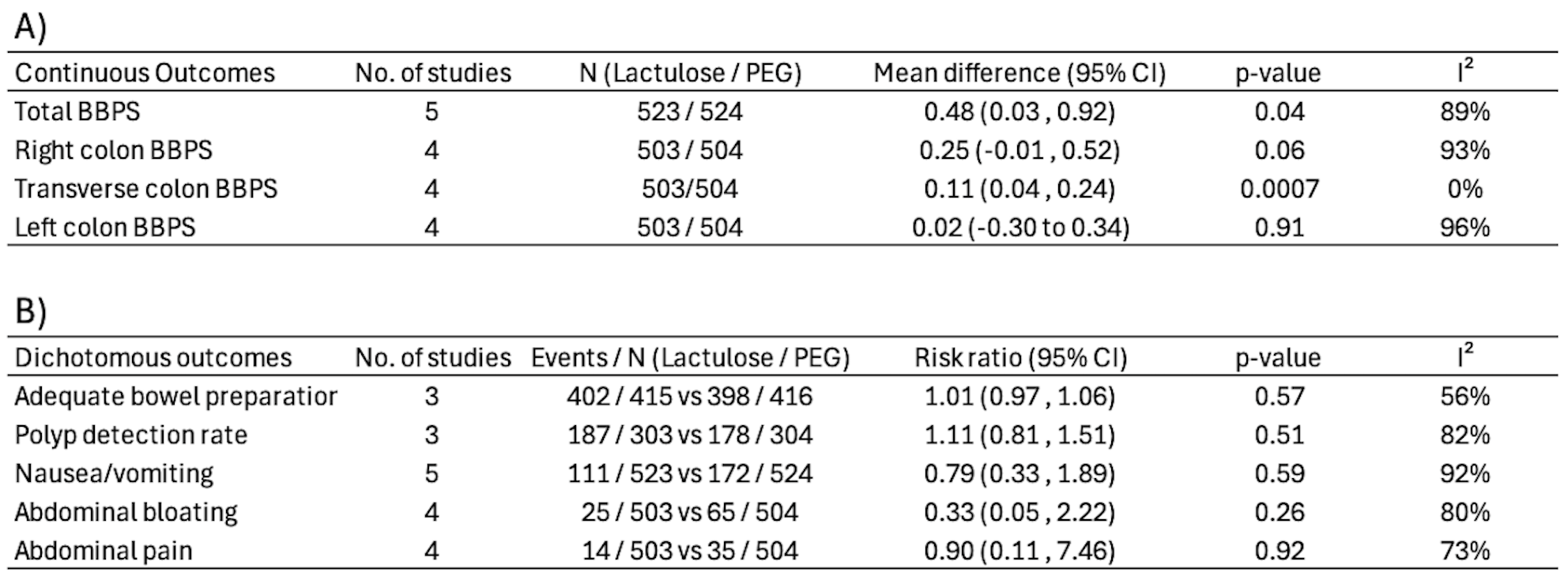
Figure: Figure 2: Summary of pooled effect measures for all outcomes. A) Continuous outcomes with mean differences, B) Dichotomous outcomes with risk ratios.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Gizem Teker indicated no relevant financial relationships.
Mehmed Taha Dinc indicated no relevant financial relationships.
Narisara Tribuddharat indicated no relevant financial relationships.
Okan Cetin indicated no relevant financial relationships.
Bilger Cavus indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Gizem Teker, MD2, Mehmed Taha Dinc, MD3, Narisara Tribuddharat, MD1, Okan Cetin, MD2, Bilger Cavus, MD2. P2420 - Lactulose vs Polyethylene Glycol for Colonoscopy Bowel Preparation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2Istanbul University, Istanbul, Istanbul, Turkey; 3Boston Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Effective colonoscopy depends on successful bowel preparation. Polyethylene glycol (PEG) solutions are the standard regimens, but they are often poorly tolerated due to their taste and large volume. Lactulose, an osmotic laxative primarily used to treat constipation, has emerged as a more palatable, lower-volume alternative for bowel preparation. Studies to date comparing these two regimens have yielded variable and sometimes conflicting results. In this systematic review and meta-analysis, we aimed to compare lactulose- and PEG-based regimens in terms of bowel cleansing efficacy and adverse events.
Methods: We conducted a systematic literature search in PubMed, Embase, and Cochrane databases through May 2025 to identify randomized controlled trials (RCTs) comparing lactulose- and PEG-based bowel preparation regimens for colonoscopy in adults that reported at least one outcome of interest. The primary outcome was the bowel cleansing efficacy; secondary outcomes were polyp detection rate and adverse events. The mean difference (MD) and risk ratio (RR) were used as effect measures for continuous and dichotomous outcomes, respectively. Pooled analyses were performed using random-effects models.
Results: Six RCTs encompassing 1,447 patients (54.2% female; mean age 51.7 years) were included. Baseline characteristics were similar between the two regimens across all studies. Adequate bowel preparation rates were similar between the lactulose and PEG groups (RR 1.01, 95% CI 0.97–1.06). Lactulose was associated with modestly higher total Boston Bowel Preparation Scale (BBPS) scores (MD 0.48, 95% CI 0.03–0.92, Figure 1) and transverse colon BBPS scores (MD 0.11, 95% CI 0.04–0.24), whereas differences in right colon (MD 0.25, 95% CI -0.01–0.52) and left colon BBPS scores (MD 0.02, 95% CI -0.30–0.34) did not reach statistical significance. Polyp detection rates did not differ significantly (RR 1.11, 95% CI 0.81–1.51). Adverse event rates, including nausea or vomiting (RR 0.79, 95% CI 0.33–1.89), abdominal bloating (RR 0.33, 95% CI 0.05–2.22), and abdominal pain (RR 0.90, 95% CI 0.11–7.46), were also comparable. Details of the pooled outcomes are presented in Figure 2.
Discussion: Lactulose demonstrated comparable efficacy to PEG in achieving adequate bowel preparation, with slightly higher overall and segmental BBPS scores in some regions. Polyp detection and adverse event rates were similar between the two regimens. These findings suggest that lactulose may serve as an alternative to PEG.
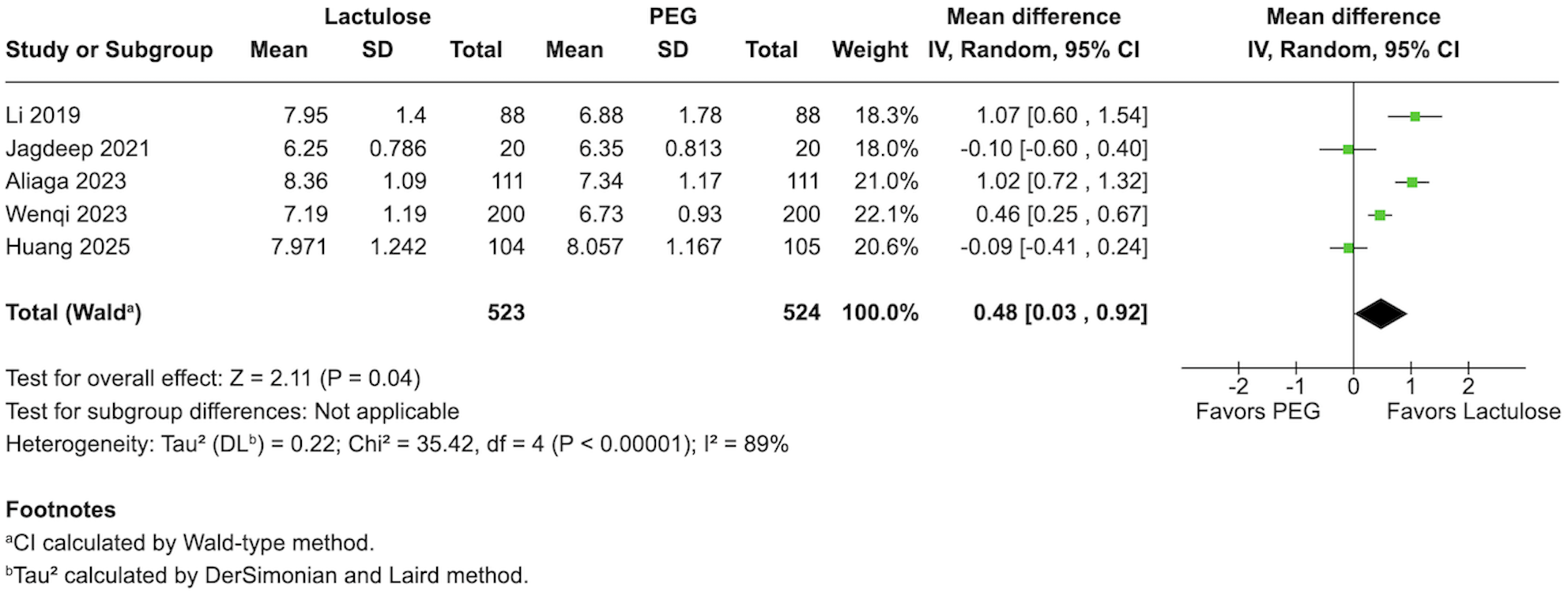
Figure: Figure 1: Forest plot of total Boston Bowel Preparation Scale (BBPS) scores comparing lactulose versus polyethylene glycol (PEG).
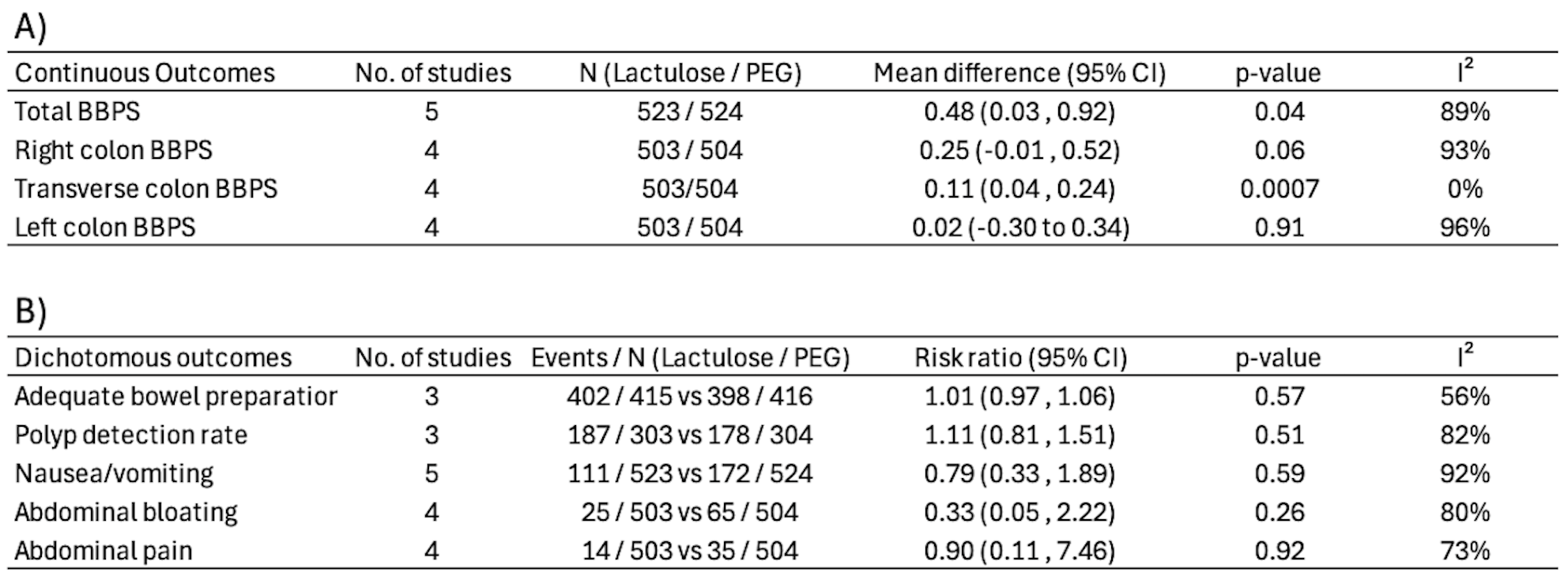
Figure: Figure 2: Summary of pooled effect measures for all outcomes. A) Continuous outcomes with mean differences, B) Dichotomous outcomes with risk ratios.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Gizem Teker indicated no relevant financial relationships.
Mehmed Taha Dinc indicated no relevant financial relationships.
Narisara Tribuddharat indicated no relevant financial relationships.
Okan Cetin indicated no relevant financial relationships.
Bilger Cavus indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Gizem Teker, MD2, Mehmed Taha Dinc, MD3, Narisara Tribuddharat, MD1, Okan Cetin, MD2, Bilger Cavus, MD2. P2420 - Lactulose vs Polyethylene Glycol for Colonoscopy Bowel Preparation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
