Monday Poster Session
Category: Colon
P2394 - Exploring Racial and Ethnic Disparities in Survival Among Patients With MSI-High Rectal Cancer: A Population-Based Study Using SEER Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Geraldine Nabeta, MD, MS (she/her/hers)
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Janani Arunachalam, MBBS1, Geraldine Nabeta, MD2, Mridula Sree Naagendran, MBBS1, Brian Byrne, MD3
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3University of Connecticut, Plainville, CT
Introduction: Microsatellite instability (MSI), a molecular indicator of defective DNA mismatch repair, is seen in ~7% of rectal cancers. Tumors with MSI, either from sporadic epigenetic silencing of MLH1 gene or germline mutations in MMR genes, are highly susceptible to immune checkpoint inhibitors. Racial disparities in rectal cancer survival are well-documented, showing that non-Hispanic Black race is associated with poor survival outcomes. It remains unknown whether such disparities persist among patients with MSI-high (MSI-H) disease. Hence, we aimed to explore these disparities in MSI-H rectal cancer during the immuno-oncology era, as understanding them is crucial for addressing gaps in care.
Methods: We retrospectively collected data from the Surveillance, Epidemiology, and End Results (SEER) cancer database for patients diagnosed with rectal cancer (ICD code C20.9) from 2018 to 2021 and have MSI high (MSI-H) disease. We investigated disparities in survival outcomes of MSI-high rectal cancer based on age, sex, race, stage, annual income and rural vs. urban residency. Statistical analysis was conducted using R software, with the log-rank (Mantel-Cox) test used for group comparisons.
Results: 637 patients with MSI-H rectal cancer were identified, with 95% having rectal adenocarcinoma. 65% were Caucasians, 10% Blacks and 15% Hispanics. 1-year overall survival (OS) was 88%, and 3-year OS was 71%. 1-year cancer-specific survival (CSS) was 91%, and 3-year CSS was 78%. There was no statistically significant difference in survival outcomes (OS and CSS) when stratified based on race, sex, household income or rural vs. urban residency. Median overall survival (mOS) was poorer in patients with metastatic disease (34 months), compared to those with localised or regional disease (p < 0.0001).Younger patients (age < 65 years) had better overall survival among compared to older patients aged 65+ years (p < 0.0001).
Discussion: We did not observe significant racial or ethnic disparities in survival outcomes in MSI-high rectal cancer. Favorable molecular framework of MSI-high tumors and widespread accessibility of immunotherapy may have mitigated some of the disparities seen in the broader rectal cancer population. Larger data or pooled analyses may be needed to further clarify these findings. Additional research is warranted to explore whether such disparities persist in patients with other rectal cancer subtypes and to better understand the underlying contributors to the disparities observed in prior studies.
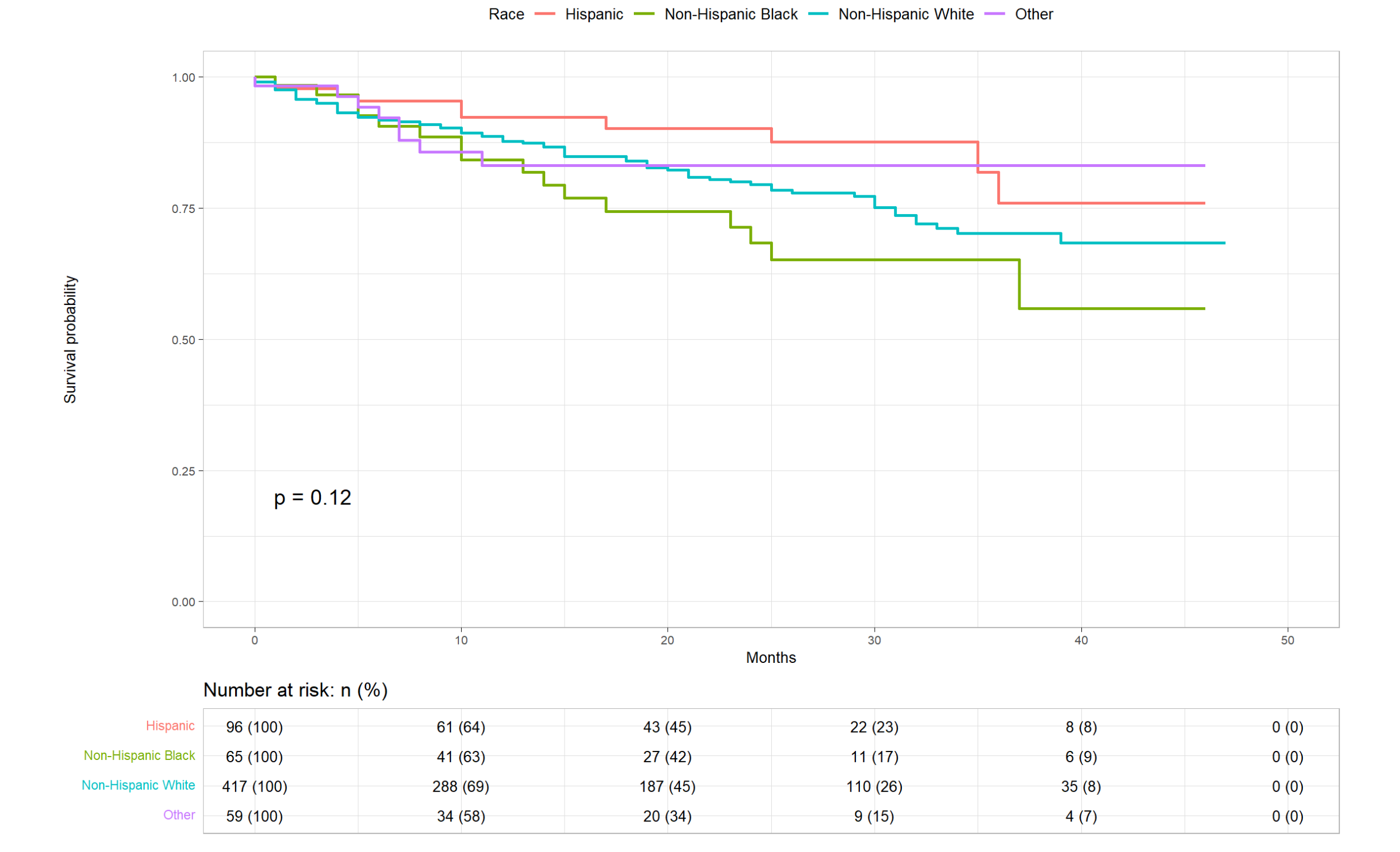
Figure: Kaplan-Meier curves showing overall survival among different racial/ethnic groups for patients with MSI-high rectal cancer
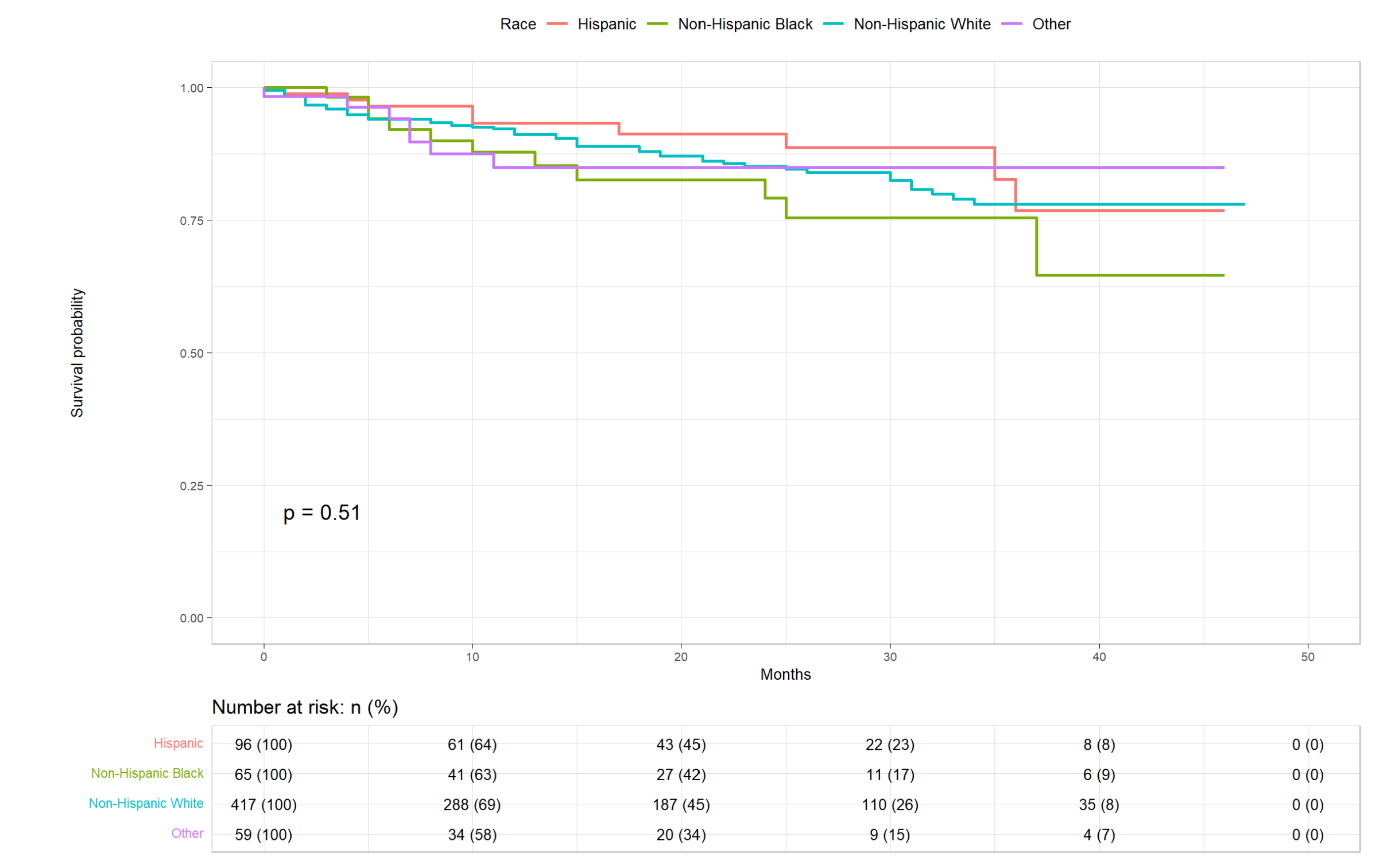
Figure: Kaplan-Meier curves illustrating cancer specific survival among different racial/ethnic groups for patients with MSI-high rectal cancer
Disclosures:
Janani Arunachalam indicated no relevant financial relationships.
Geraldine Nabeta indicated no relevant financial relationships.
Mridula Sree Naagendran indicated no relevant financial relationships.
Brian Byrne indicated no relevant financial relationships.
Janani Arunachalam, MBBS1, Geraldine Nabeta, MD2, Mridula Sree Naagendran, MBBS1, Brian Byrne, MD3. P2394 - Exploring Racial and Ethnic Disparities in Survival Among Patients With MSI-High Rectal Cancer: A Population-Based Study Using SEER Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3University of Connecticut, Plainville, CT
Introduction: Microsatellite instability (MSI), a molecular indicator of defective DNA mismatch repair, is seen in ~7% of rectal cancers. Tumors with MSI, either from sporadic epigenetic silencing of MLH1 gene or germline mutations in MMR genes, are highly susceptible to immune checkpoint inhibitors. Racial disparities in rectal cancer survival are well-documented, showing that non-Hispanic Black race is associated with poor survival outcomes. It remains unknown whether such disparities persist among patients with MSI-high (MSI-H) disease. Hence, we aimed to explore these disparities in MSI-H rectal cancer during the immuno-oncology era, as understanding them is crucial for addressing gaps in care.
Methods: We retrospectively collected data from the Surveillance, Epidemiology, and End Results (SEER) cancer database for patients diagnosed with rectal cancer (ICD code C20.9) from 2018 to 2021 and have MSI high (MSI-H) disease. We investigated disparities in survival outcomes of MSI-high rectal cancer based on age, sex, race, stage, annual income and rural vs. urban residency. Statistical analysis was conducted using R software, with the log-rank (Mantel-Cox) test used for group comparisons.
Results: 637 patients with MSI-H rectal cancer were identified, with 95% having rectal adenocarcinoma. 65% were Caucasians, 10% Blacks and 15% Hispanics. 1-year overall survival (OS) was 88%, and 3-year OS was 71%. 1-year cancer-specific survival (CSS) was 91%, and 3-year CSS was 78%. There was no statistically significant difference in survival outcomes (OS and CSS) when stratified based on race, sex, household income or rural vs. urban residency. Median overall survival (mOS) was poorer in patients with metastatic disease (34 months), compared to those with localised or regional disease (p < 0.0001).Younger patients (age < 65 years) had better overall survival among compared to older patients aged 65+ years (p < 0.0001).
Discussion: We did not observe significant racial or ethnic disparities in survival outcomes in MSI-high rectal cancer. Favorable molecular framework of MSI-high tumors and widespread accessibility of immunotherapy may have mitigated some of the disparities seen in the broader rectal cancer population. Larger data or pooled analyses may be needed to further clarify these findings. Additional research is warranted to explore whether such disparities persist in patients with other rectal cancer subtypes and to better understand the underlying contributors to the disparities observed in prior studies.
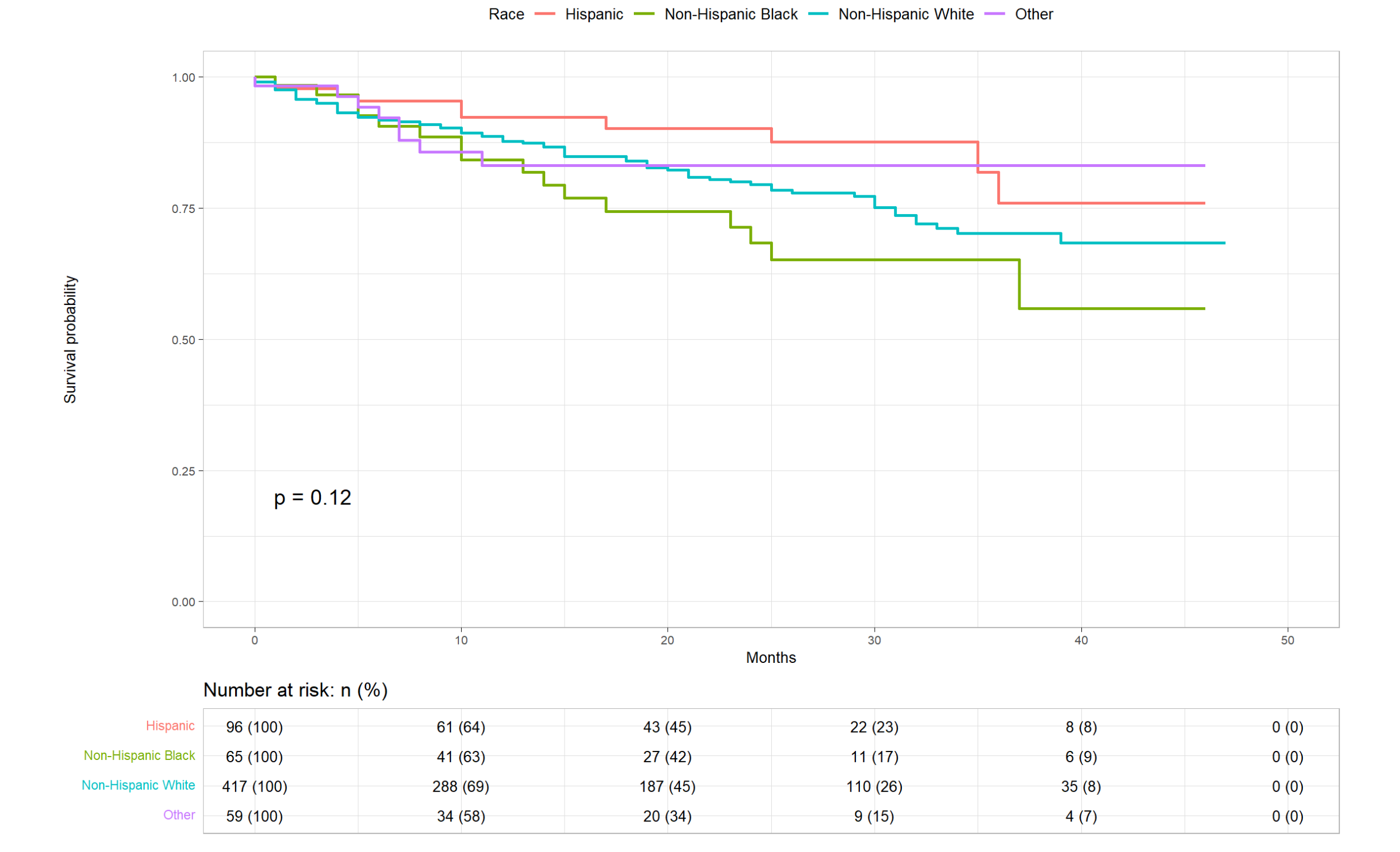
Figure: Kaplan-Meier curves showing overall survival among different racial/ethnic groups for patients with MSI-high rectal cancer
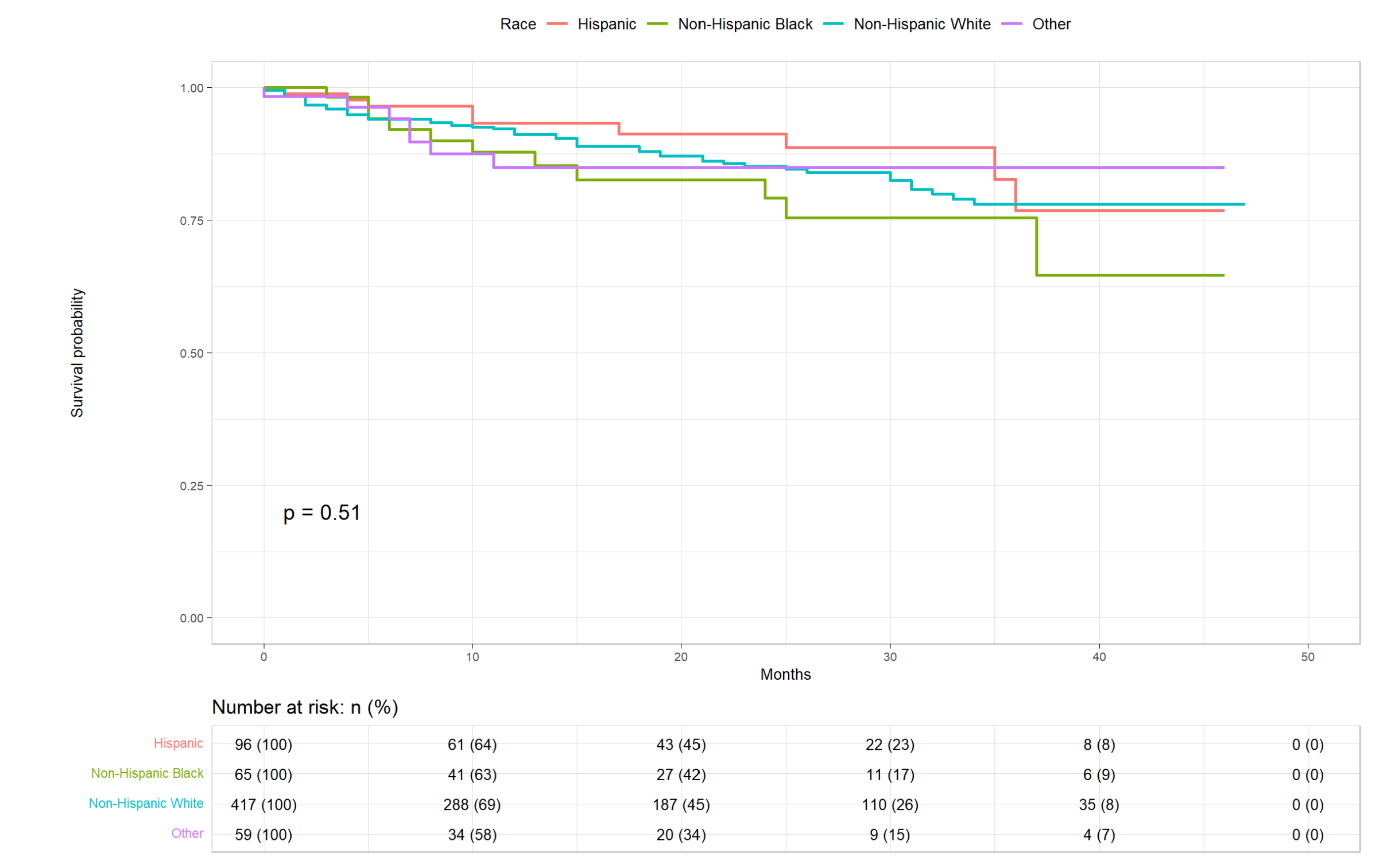
Figure: Kaplan-Meier curves illustrating cancer specific survival among different racial/ethnic groups for patients with MSI-high rectal cancer
Disclosures:
Janani Arunachalam indicated no relevant financial relationships.
Geraldine Nabeta indicated no relevant financial relationships.
Mridula Sree Naagendran indicated no relevant financial relationships.
Brian Byrne indicated no relevant financial relationships.
Janani Arunachalam, MBBS1, Geraldine Nabeta, MD2, Mridula Sree Naagendran, MBBS1, Brian Byrne, MD3. P2394 - Exploring Racial and Ethnic Disparities in Survival Among Patients With MSI-High Rectal Cancer: A Population-Based Study Using SEER Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
