Monday Poster Session
Category: Biliary/Pancreas
P2370 - Needle Knife Facilitated Biliary Restenting for Management of Malignant Duodenobiliary Obstruction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Rachael Wong, BS (she/her/hers)
Carle Foundation hospital
Arcadia, CA
Presenting Author(s)
Rachael Wong, BS1, Ahmad Al-Taee, MD2
1Carle Foundation hospital, Arcadia, CA; 2Mercy Hospital, Oklahoma City, OK
Introduction: Biliary and duodenal obstruction are known complications of pancreatic head cancer. This case describes a novel technique for management of biliary stent obstruction after placement of duodenal self-expanding metal stent (SEMS).
Case Description/
Methods: A 54-year-old man with advanced pancreatic head cancer presented with nausea, vomiting, and abdominal distention. He previously underwent ERCP with placement of a fully covered SEMS with anti-migration flaps for biliary obstruction. Laboratory evaluation showed mildly elevated liver enzymes (ALP 187 U/L, AST 67 U/L, ALT 222 U/L) with a normal bilirubin. Abdominal CT scan revealed a fluid-filled, distended stomach likely resulting from duodenal invasion by pancreatic cancer. Endoscopy revealed a malignant-appearing duodenal stenosis that was treated by placement of a 22 mm x 9 cm uncovered SEMS (Fig 1).
Two days later, he developed fevers and worsening liver enzymes (ALP 537 U/L, AST 176 U/L, ALT 339 U/L, total bilirubin 3 mg/dL), suggesting biliary stent occlusion by the duodenal SEMS. Endoscopy showed tissue ingrowth of the duodenal stent, and the distal end of the biliary stent was inaccessible. A needle knife was then used to incise the sidewalls of the duodenal and biliary stents, permitting biliary access. Cholangiogram showed a filling defect consistent with sludge, which was cleared with balloon sweep. A second fully covered SEMS with anti-migration flaps was deployed through the sidewall of the existing biliary and duodenal stents into main bile duct, with its distal end protruding into the duodenum, forming an inverted Y configuration (Fig 2). After the procedure, his fever resolved, liver enzymes normalized, and he was discharged home in a stable condition.
Discussion: Biliary stent obstruction after duodenal stent placement has been previously reported. This has typically been managed by using argon plasma coagulation to trim the interstices of the duodenal stent to gain access to the distal end of the biliary stent and deploy a new stent. Here we report a unique scenario where the distal end of the biliary stent is inaccessible. We demonstrate the novel use of a needle knife to dissect the sidewalls of the duodenal and biliary stents to obtain biliary access and deploy a new biliary stent. This technique offers a novel and valuable option for managing biliary stent obstruction after duodenal stent placement.

Figure: FIgure 1: Malignant-appearing duodenal stenosis that was treated by placement of a 22 mmx 9 cm uncovered SEMS.
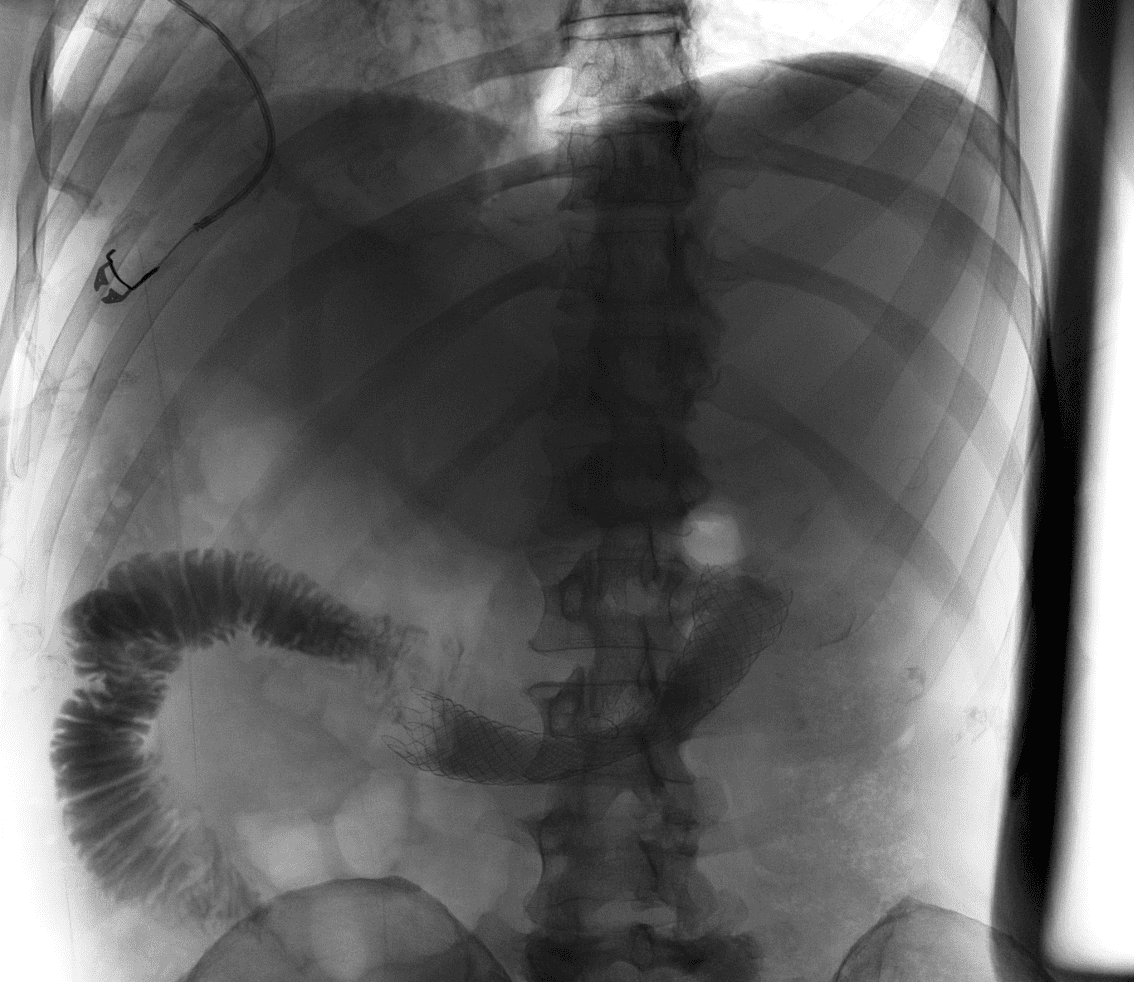
Figure: Figure 2: Inverted Y configuration created by a second fully covered SEMS with anti-migration flaps.
Disclosures:
Rachael Wong indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Rachael Wong, BS1, Ahmad Al-Taee, MD2. P2370 - Needle Knife Facilitated Biliary Restenting for Management of Malignant Duodenobiliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Carle Foundation hospital, Arcadia, CA; 2Mercy Hospital, Oklahoma City, OK
Introduction: Biliary and duodenal obstruction are known complications of pancreatic head cancer. This case describes a novel technique for management of biliary stent obstruction after placement of duodenal self-expanding metal stent (SEMS).
Case Description/
Methods: A 54-year-old man with advanced pancreatic head cancer presented with nausea, vomiting, and abdominal distention. He previously underwent ERCP with placement of a fully covered SEMS with anti-migration flaps for biliary obstruction. Laboratory evaluation showed mildly elevated liver enzymes (ALP 187 U/L, AST 67 U/L, ALT 222 U/L) with a normal bilirubin. Abdominal CT scan revealed a fluid-filled, distended stomach likely resulting from duodenal invasion by pancreatic cancer. Endoscopy revealed a malignant-appearing duodenal stenosis that was treated by placement of a 22 mm x 9 cm uncovered SEMS (Fig 1).
Two days later, he developed fevers and worsening liver enzymes (ALP 537 U/L, AST 176 U/L, ALT 339 U/L, total bilirubin 3 mg/dL), suggesting biliary stent occlusion by the duodenal SEMS. Endoscopy showed tissue ingrowth of the duodenal stent, and the distal end of the biliary stent was inaccessible. A needle knife was then used to incise the sidewalls of the duodenal and biliary stents, permitting biliary access. Cholangiogram showed a filling defect consistent with sludge, which was cleared with balloon sweep. A second fully covered SEMS with anti-migration flaps was deployed through the sidewall of the existing biliary and duodenal stents into main bile duct, with its distal end protruding into the duodenum, forming an inverted Y configuration (Fig 2). After the procedure, his fever resolved, liver enzymes normalized, and he was discharged home in a stable condition.
Discussion: Biliary stent obstruction after duodenal stent placement has been previously reported. This has typically been managed by using argon plasma coagulation to trim the interstices of the duodenal stent to gain access to the distal end of the biliary stent and deploy a new stent. Here we report a unique scenario where the distal end of the biliary stent is inaccessible. We demonstrate the novel use of a needle knife to dissect the sidewalls of the duodenal and biliary stents to obtain biliary access and deploy a new biliary stent. This technique offers a novel and valuable option for managing biliary stent obstruction after duodenal stent placement.

Figure: FIgure 1: Malignant-appearing duodenal stenosis that was treated by placement of a 22 mmx 9 cm uncovered SEMS.
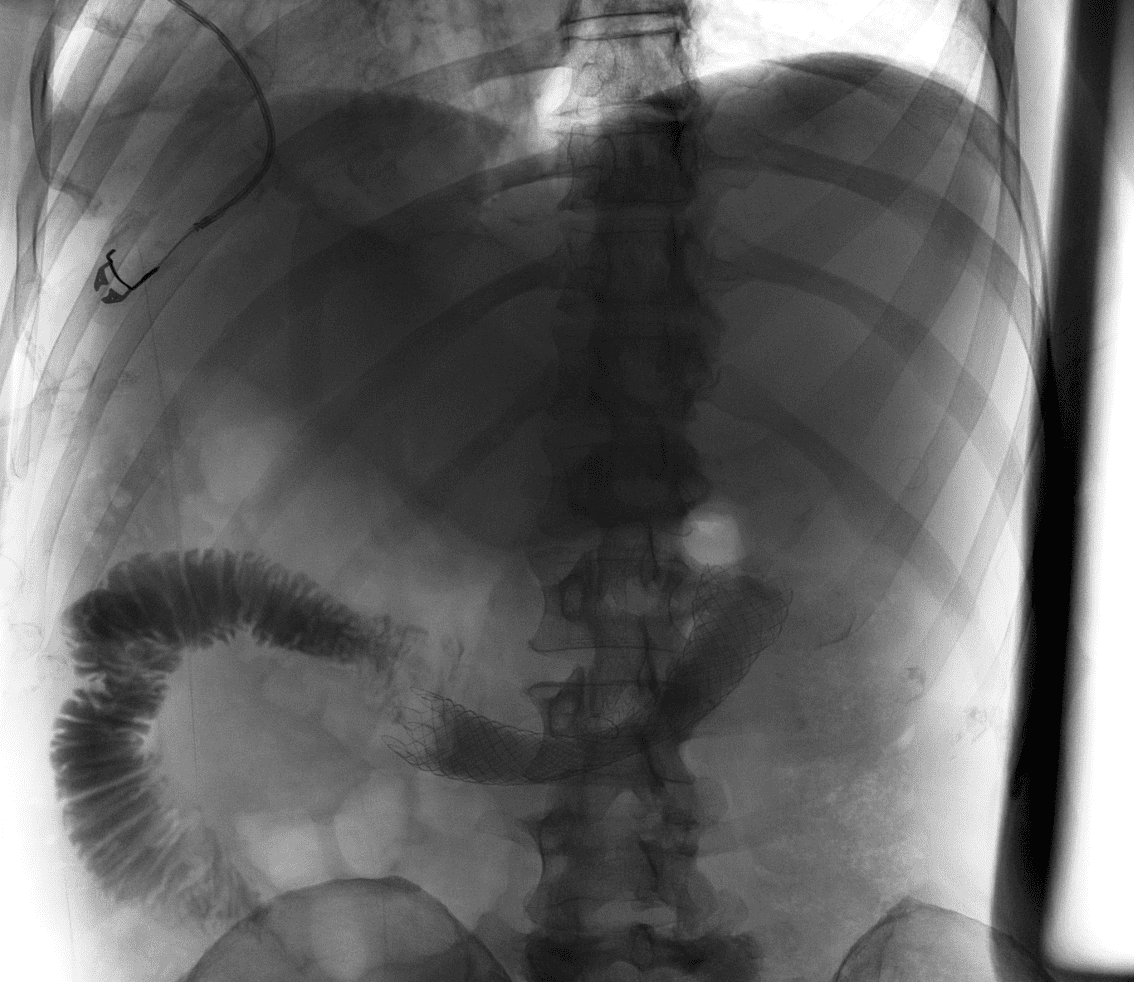
Figure: Figure 2: Inverted Y configuration created by a second fully covered SEMS with anti-migration flaps.
Disclosures:
Rachael Wong indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Rachael Wong, BS1, Ahmad Al-Taee, MD2. P2370 - Needle Knife Facilitated Biliary Restenting for Management of Malignant Duodenobiliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
