Monday Poster Session
Category: Biliary/Pancreas
P2366 - Atypical Autoimmune Pancreatitis in Young Adult: Diagnostic Dilemma Between Type 1 and Type 2 AIP
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sharan Poonja, MD (he/him/his)
Tulane University
New Orleans, LA
Presenting Author(s)
Sharan Poonja, MD1, Madeline Novack, MD2, Peng-Sheng Ting, MD3
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane School of Medicine, New Orleans, LA
Introduction: Autoimmune pancreatitis (AIP) is a rare, immune-mediated form of chronic pancreatitis, that exists in two subtypes. Type 1, associated with IgG4-related disease (IgG4-RD), typically presents in older men and is characterized by elevated serum IgG4, extra pancreatic organ involvement, and histologic infiltration of IgG4-positive plasma cells. Type 2 affects younger individuals, lacks systemic involvement, and is often associated with IBD. Differentiating the subtypes is crucial for determining treatment duration, relapse risk, and long-term follow-up.
Case Description/
Methods: A 19-year-old male with no prior autoimmune or GI history presented with 3 months of progressive postprandial upper abdominal pain worsened with fatty foods that radiates to his back as well as an eight-pound weight loss and intermittent hematochezia. His initial labs revealed a mild cholestatic liver injury pattern while CT and MRCP imaging showed a thickened sausage-shaped pancreas with focal mass-like thickening of pancreatic head and intrahepatic and extrahepatic biliary ductal dilation with narrowing. These findings were classic for AIP but also suggested IgG4-related sclerosing cholangitis. However, while IgG1, IgG2, and IgG3 subclasses were elevated, IgG4 was negative and endoscopic ultrasound with fine-needle biopsy of the pancreas showed acute inflammation and mild fibrosis without histologic evidence of IgG4-RD or lymphoma. Liver biopsy revealed moderate portal and periductal fibrosis and scattered portal mixed inflammation consistent with biliary obstructive process but without evidence of autoimmune hepatitis or IgG4 tissue infiltration. He was started on steroid therapy and had significant improvement in liver enzymes with resolution of symptoms.
Discussion: This case illustrates an atypical presentation of AIP in a young adult, with a diagnostic profile that straddles both subtypes. The patient’s age, normal IgG4, and symptoms suggestive of IBD align with Type 2, while biliary dilation and narrowing is representative of sclerosing cholangitis in Type 1. Although both serologic and histologic IgG4 criteria are lacking, the elevation of non-IgG4 IgG subclasses raises the possibility of an atypical or incomplete variant of IgG4-RD. This diagnostic ambiguity underscores the limitations of current classification systems and raises the question of whether such cases represent a broader disease spectrum or an intermediate phenotype between the established AIP subtypes. *Generative AI assisted in abstract writing.
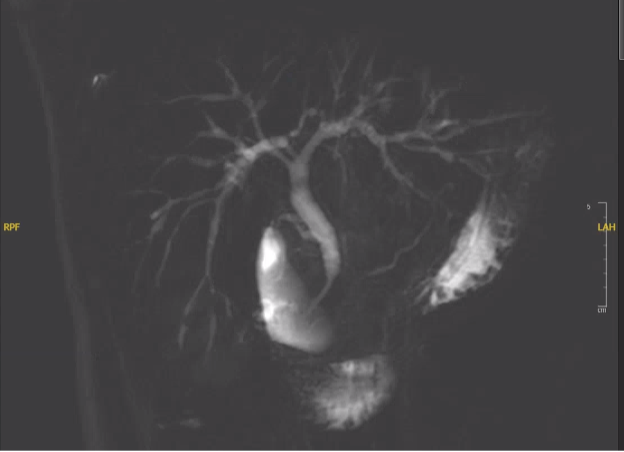
Figure: Intrapancreatic CBD segment stricturing with beading of intrahepatic bile ducts
Disclosures:
Sharan Poonja indicated no relevant financial relationships.
Madeline Novack indicated no relevant financial relationships.
Peng-Sheng Ting indicated no relevant financial relationships.
Sharan Poonja, MD1, Madeline Novack, MD2, Peng-Sheng Ting, MD3. P2366 - Atypical Autoimmune Pancreatitis in Young Adult: Diagnostic Dilemma Between Type 1 and Type 2 AIP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane School of Medicine, New Orleans, LA
Introduction: Autoimmune pancreatitis (AIP) is a rare, immune-mediated form of chronic pancreatitis, that exists in two subtypes. Type 1, associated with IgG4-related disease (IgG4-RD), typically presents in older men and is characterized by elevated serum IgG4, extra pancreatic organ involvement, and histologic infiltration of IgG4-positive plasma cells. Type 2 affects younger individuals, lacks systemic involvement, and is often associated with IBD. Differentiating the subtypes is crucial for determining treatment duration, relapse risk, and long-term follow-up.
Case Description/
Methods: A 19-year-old male with no prior autoimmune or GI history presented with 3 months of progressive postprandial upper abdominal pain worsened with fatty foods that radiates to his back as well as an eight-pound weight loss and intermittent hematochezia. His initial labs revealed a mild cholestatic liver injury pattern while CT and MRCP imaging showed a thickened sausage-shaped pancreas with focal mass-like thickening of pancreatic head and intrahepatic and extrahepatic biliary ductal dilation with narrowing. These findings were classic for AIP but also suggested IgG4-related sclerosing cholangitis. However, while IgG1, IgG2, and IgG3 subclasses were elevated, IgG4 was negative and endoscopic ultrasound with fine-needle biopsy of the pancreas showed acute inflammation and mild fibrosis without histologic evidence of IgG4-RD or lymphoma. Liver biopsy revealed moderate portal and periductal fibrosis and scattered portal mixed inflammation consistent with biliary obstructive process but without evidence of autoimmune hepatitis or IgG4 tissue infiltration. He was started on steroid therapy and had significant improvement in liver enzymes with resolution of symptoms.
Discussion: This case illustrates an atypical presentation of AIP in a young adult, with a diagnostic profile that straddles both subtypes. The patient’s age, normal IgG4, and symptoms suggestive of IBD align with Type 2, while biliary dilation and narrowing is representative of sclerosing cholangitis in Type 1. Although both serologic and histologic IgG4 criteria are lacking, the elevation of non-IgG4 IgG subclasses raises the possibility of an atypical or incomplete variant of IgG4-RD. This diagnostic ambiguity underscores the limitations of current classification systems and raises the question of whether such cases represent a broader disease spectrum or an intermediate phenotype between the established AIP subtypes. *Generative AI assisted in abstract writing.
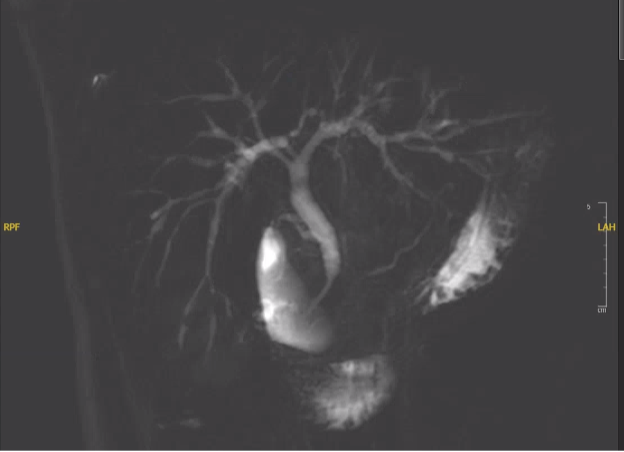
Figure: Intrapancreatic CBD segment stricturing with beading of intrahepatic bile ducts
Disclosures:
Sharan Poonja indicated no relevant financial relationships.
Madeline Novack indicated no relevant financial relationships.
Peng-Sheng Ting indicated no relevant financial relationships.
Sharan Poonja, MD1, Madeline Novack, MD2, Peng-Sheng Ting, MD3. P2366 - Atypical Autoimmune Pancreatitis in Young Adult: Diagnostic Dilemma Between Type 1 and Type 2 AIP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
