Monday Poster Session
Category: Esophagus
P2822 - Complete Endoscopic and Histopathologic Resolution of Lymphocytic Esophagitis with Budesonide Slurry Therapy After Failure of PPI Therapy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hussam Almasri, MD, MRCP(UK)
University of North Dakota, School of Medicine and Health Sciences
Fargo, ND
Presenting Author(s)
Hussam Almasri, MD, MRCP(UK)1, Tory Durkin, MD2, Jeffrey Murray, MD3
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 3Sanford Health, Sioux Falls, SD
Introduction: Lymphocytic esophagitis (LE), first described by Rubio et al. in 2006, is a rare form of chronic esophagitis characterized by a dense intra-epithelial parapapillary lymphocytic infiltration. LE has been increasingly recognized due to increased awareness and use of esophageal biopsies. It is notably more common in older women. We present a case of LE with failure to respond to PPI therapy and subsequent clinical, endoscopic, and complete histopathologic response to topical budesonide.
Case Description/
Methods: A 69-year-old female with a known medical history of Charcot-Marie-Tooth (CMT) disease, hypertension, and gastroesophageal reflux disease (GERD), who presented with progressive solid food dysphagia for a few years, first noticed difficulty swallowing pills. She also had symptoms of a choking sensation in the chest without significant weight loss. The association with CMT was felt to be a rare epiphenomenon; therefore, prognosticating esophagogastroduodenoscopy (EGD) was done, which showed rings with EREFS classification of grade 1, and a benign-appearing intrinsic moderate esophageal stenosis at 18 cm from the incisors, with dilation performed by passing the scope only. Esophageal biopsies were consistent with lymphocytic esophagitis. Laboratory studies showed a normal blood count, including lymphocyte count. After a trial of twice daily PPI course for 12 weeks, a repeat EGD was performed with similar rings and a stenosis with biopsies showing persistence of LE findings; therefore, the patient was started on a budesonide slurry 2 mg twice daily with improvement of dysphagia. Subsequent EGD, 12 weeks later, showed improvement of the rings and no stricture. Esophageal biopsies also showed complete resolution of the lymphocytic infiltration (Figure 1+2). The patient remained dysphagia-free at 6-month follow-up.
Discussion: Due to a lack of clear guidance on managing LE, most clinicians use similar medical treatment to eosinophilic esophagitis. In terms of histopathologic remission, more than half of patients with LE will fail high-dose PPI therapy, and it is hypothesized that PPI exerts its effect via managing associated GERD only, instead of a direct effect on the inflammatory process of LE. Therefore, it is not clear if topical steroids such as budesonide slurry should be considered as first line in patients with LE and strictures to prevent further need for invasive procedures. Larger studies will be needed to form a clear consensus guide on the management of patients with LE.
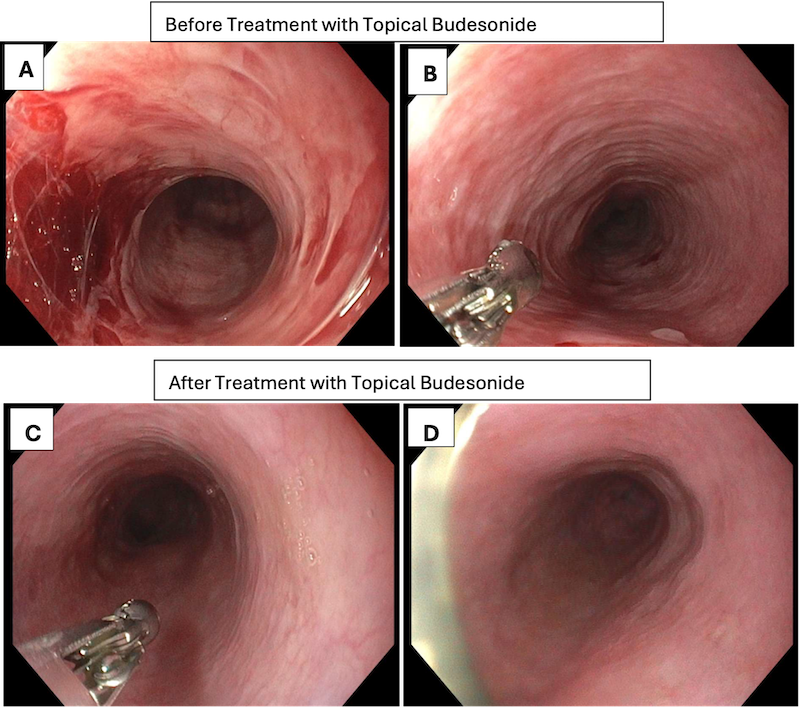
Figure: Figure 1: Endoscopic findings of the upper and mid-esophagus. A+B before treatment showing stenosis with rings. C+D Improvement of stenosis and rings after treatment.
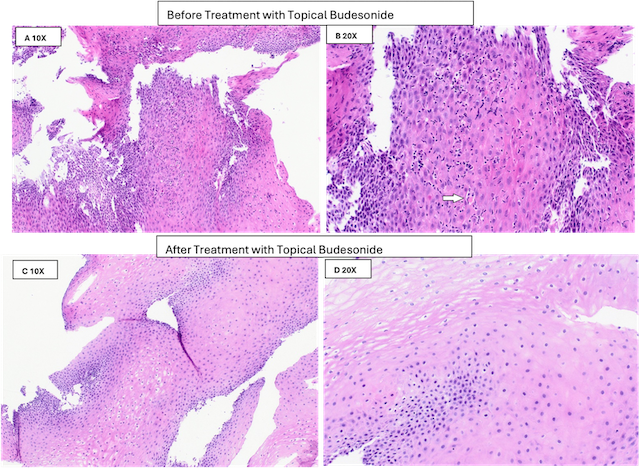
Figure: Figure 2 A+B Esophageal squamous mucosa with numerous intraepithelial lymphocytes, edema, and necrotic keratinocytes (white arrow) H&E; C+D: Esophageal squamous mucosa with no residual inflammatory cells H&E.
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Tory Durkin indicated no relevant financial relationships.
Jeffrey Murray indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP(UK)1, Tory Durkin, MD2, Jeffrey Murray, MD3. P2822 - Complete Endoscopic and Histopathologic Resolution of Lymphocytic Esophagitis with Budesonide Slurry Therapy After Failure of PPI Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 3Sanford Health, Sioux Falls, SD
Introduction: Lymphocytic esophagitis (LE), first described by Rubio et al. in 2006, is a rare form of chronic esophagitis characterized by a dense intra-epithelial parapapillary lymphocytic infiltration. LE has been increasingly recognized due to increased awareness and use of esophageal biopsies. It is notably more common in older women. We present a case of LE with failure to respond to PPI therapy and subsequent clinical, endoscopic, and complete histopathologic response to topical budesonide.
Case Description/
Methods: A 69-year-old female with a known medical history of Charcot-Marie-Tooth (CMT) disease, hypertension, and gastroesophageal reflux disease (GERD), who presented with progressive solid food dysphagia for a few years, first noticed difficulty swallowing pills. She also had symptoms of a choking sensation in the chest without significant weight loss. The association with CMT was felt to be a rare epiphenomenon; therefore, prognosticating esophagogastroduodenoscopy (EGD) was done, which showed rings with EREFS classification of grade 1, and a benign-appearing intrinsic moderate esophageal stenosis at 18 cm from the incisors, with dilation performed by passing the scope only. Esophageal biopsies were consistent with lymphocytic esophagitis. Laboratory studies showed a normal blood count, including lymphocyte count. After a trial of twice daily PPI course for 12 weeks, a repeat EGD was performed with similar rings and a stenosis with biopsies showing persistence of LE findings; therefore, the patient was started on a budesonide slurry 2 mg twice daily with improvement of dysphagia. Subsequent EGD, 12 weeks later, showed improvement of the rings and no stricture. Esophageal biopsies also showed complete resolution of the lymphocytic infiltration (Figure 1+2). The patient remained dysphagia-free at 6-month follow-up.
Discussion: Due to a lack of clear guidance on managing LE, most clinicians use similar medical treatment to eosinophilic esophagitis. In terms of histopathologic remission, more than half of patients with LE will fail high-dose PPI therapy, and it is hypothesized that PPI exerts its effect via managing associated GERD only, instead of a direct effect on the inflammatory process of LE. Therefore, it is not clear if topical steroids such as budesonide slurry should be considered as first line in patients with LE and strictures to prevent further need for invasive procedures. Larger studies will be needed to form a clear consensus guide on the management of patients with LE.
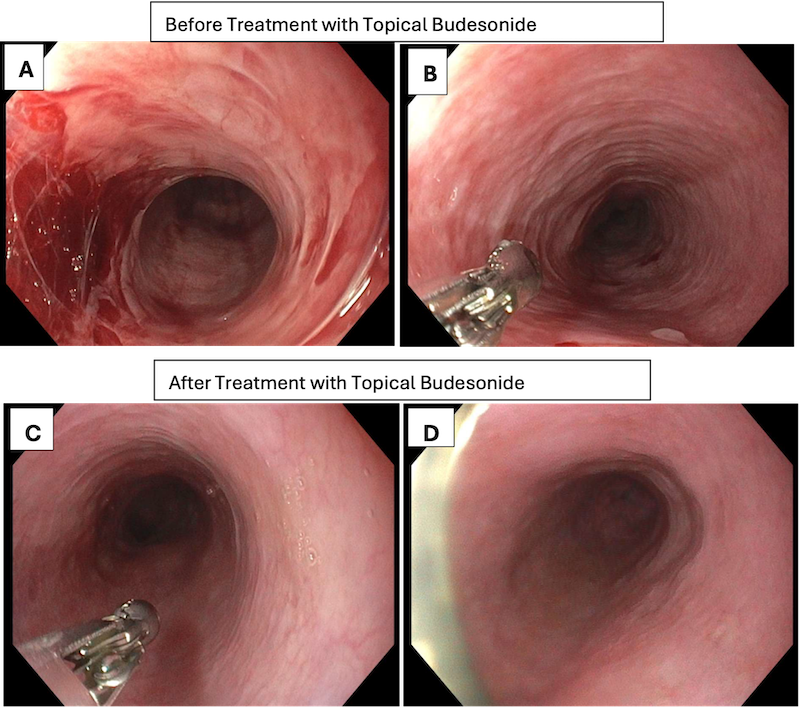
Figure: Figure 1: Endoscopic findings of the upper and mid-esophagus. A+B before treatment showing stenosis with rings. C+D Improvement of stenosis and rings after treatment.
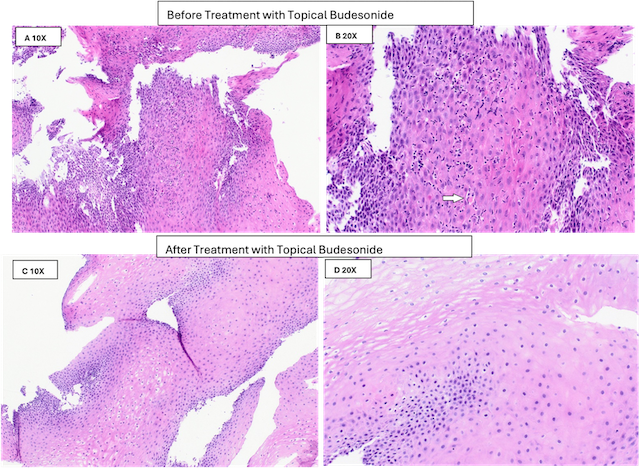
Figure: Figure 2 A+B Esophageal squamous mucosa with numerous intraepithelial lymphocytes, edema, and necrotic keratinocytes (white arrow) H&E; C+D: Esophageal squamous mucosa with no residual inflammatory cells H&E.
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Tory Durkin indicated no relevant financial relationships.
Jeffrey Murray indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP(UK)1, Tory Durkin, MD2, Jeffrey Murray, MD3. P2822 - Complete Endoscopic and Histopathologic Resolution of Lymphocytic Esophagitis with Budesonide Slurry Therapy After Failure of PPI Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

