Monday Poster Session
Category: Colorectal Cancer Prevention
P2615 - Colorectal Cancer Screening Outcomes in Renal Transplant Recipients: A Single Center Retrospective Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tara Alleyasin, MD
Scripps Green Hospital
San Diego, California
Presenting Author(s)
Tara Alleyasin, MD1, Sang Hee Choi, MD1, Jeffrey Nguyen, MD2, Nabil El Hage Chehade, MD1, Merveille Kouka, BS3, Jennifer Au, MD1
1Scripps Green Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3san diego mesa college, San Diego, CA
Introduction: Renal transplant (RT) recipients are at increased risk for various malignancies given chronic immunosuppression. Cancer screening guidelines are mostly based on the general population, including the recommendations for colon cancer screening. This raises the question of whether there is increased incidence of adenomas in the RT population and if increased frequency for colonoscopy (COL) for colorectal cancer (CRC) screening is warranted. This study aims to examine the adenoma detection rate (ADR) and CRC in RT recipients compared with the average-risk adult.
Methods: We conducted a single-center retrospective cohort study of adult patients who underwent CRC screening COL post-RT from 1/2013 to 12/2023. Patients with < 1 year survival post-RT, first-degree family history of CRC, or no COL reports were excluded. Primary outcomes were the incidence of precancerous polyps and CRC.
Results: Among 748 RT recipients, 187 underwent post-transplant CRC screening COL and met the inclusion criteria (mean age 57.1±10.2, 50% male, 38.5% white). The most common indication for RT was diabetes mellitus (21.9) (Table1). Tacrolimus (85%) and mycophenolate mofetil (MMF) (68.5%) were the most commonly used immunosuppressants. 45% of RT recipients were on 3 immunosuppressant. Pre-RT COL were performed in 59.9% of patients and 51.8% of the COL had no polyps found; 84.5% of these remained negative on the first post-RT COL (Table 2). The mean time from the transplant to the first COL was 45.7±32.4 months. Post-RT COL findings included no polyps in 71.1%, at least 1 adenoma in 27.8%, and high-risk adenoma (HRA) in 8%. HRA included 6.4% with ≥3 polyps, 1.6% with polyps ≥ 10mm, and 2.1% with villous/tubulovillous histology. Follow-up COL were performed in 8%, with 90.6% showing negative results and 1.9% identifying HRA. CRC was diagnosed in 1.1% of patients’ post-RT COL.
Discussion: Our retrospective study of RT recipients found an ADR of 27.8% and a high-risk ADR of 8%. These rates are comparable to the ADR (20%-30%) and high-risk ADR (5%-10%) reported in the literature for average-risk adults. Since there was no significant difference in ADR and high-risk ADR between average-risk adults and RT recipients, there is no indication to increase the frequency of colonoscopy intervals in RT recipients. However, larger studies with a longer period of follow up as well as a matched dataset of average-risk patients are needed to further investigate variables associated with HRA and CRC in this population.
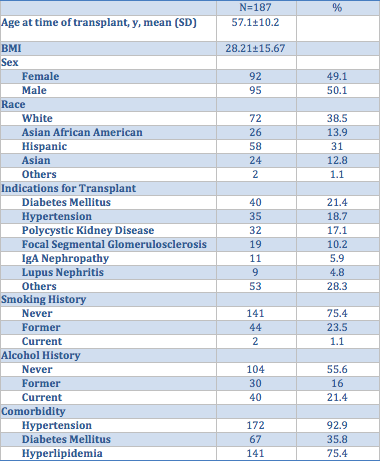
Figure: Table 1: Demographic Characteristics
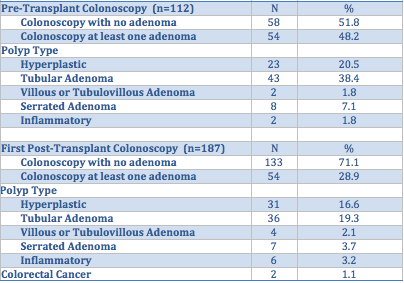
Figure: Table 2: Pre and Post-Transplant Colonoscopy Findings. Adenoma consisted of tubular, villous or tubulovillous, serrated adenomas, or polyps ≥ 10mm.
Disclosures:
Tara Alleyasin indicated no relevant financial relationships.
Sang Hee Choi indicated no relevant financial relationships.
Jeffrey Nguyen indicated no relevant financial relationships.
Nabil El Hage Chehade indicated no relevant financial relationships.
Merveille Kouka indicated no relevant financial relationships.
Jennifer Au indicated no relevant financial relationships.
Tara Alleyasin, MD1, Sang Hee Choi, MD1, Jeffrey Nguyen, MD2, Nabil El Hage Chehade, MD1, Merveille Kouka, BS3, Jennifer Au, MD1. P2615 - Colorectal Cancer Screening Outcomes in Renal Transplant Recipients: A Single Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Scripps Green Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3san diego mesa college, San Diego, CA
Introduction: Renal transplant (RT) recipients are at increased risk for various malignancies given chronic immunosuppression. Cancer screening guidelines are mostly based on the general population, including the recommendations for colon cancer screening. This raises the question of whether there is increased incidence of adenomas in the RT population and if increased frequency for colonoscopy (COL) for colorectal cancer (CRC) screening is warranted. This study aims to examine the adenoma detection rate (ADR) and CRC in RT recipients compared with the average-risk adult.
Methods: We conducted a single-center retrospective cohort study of adult patients who underwent CRC screening COL post-RT from 1/2013 to 12/2023. Patients with < 1 year survival post-RT, first-degree family history of CRC, or no COL reports were excluded. Primary outcomes were the incidence of precancerous polyps and CRC.
Results: Among 748 RT recipients, 187 underwent post-transplant CRC screening COL and met the inclusion criteria (mean age 57.1±10.2, 50% male, 38.5% white). The most common indication for RT was diabetes mellitus (21.9) (Table1). Tacrolimus (85%) and mycophenolate mofetil (MMF) (68.5%) were the most commonly used immunosuppressants. 45% of RT recipients were on 3 immunosuppressant. Pre-RT COL were performed in 59.9% of patients and 51.8% of the COL had no polyps found; 84.5% of these remained negative on the first post-RT COL (Table 2). The mean time from the transplant to the first COL was 45.7±32.4 months. Post-RT COL findings included no polyps in 71.1%, at least 1 adenoma in 27.8%, and high-risk adenoma (HRA) in 8%. HRA included 6.4% with ≥3 polyps, 1.6% with polyps ≥ 10mm, and 2.1% with villous/tubulovillous histology. Follow-up COL were performed in 8%, with 90.6% showing negative results and 1.9% identifying HRA. CRC was diagnosed in 1.1% of patients’ post-RT COL.
Discussion: Our retrospective study of RT recipients found an ADR of 27.8% and a high-risk ADR of 8%. These rates are comparable to the ADR (20%-30%) and high-risk ADR (5%-10%) reported in the literature for average-risk adults. Since there was no significant difference in ADR and high-risk ADR between average-risk adults and RT recipients, there is no indication to increase the frequency of colonoscopy intervals in RT recipients. However, larger studies with a longer period of follow up as well as a matched dataset of average-risk patients are needed to further investigate variables associated with HRA and CRC in this population.
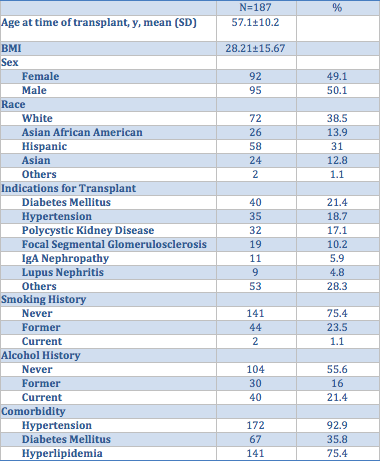
Figure: Table 1: Demographic Characteristics
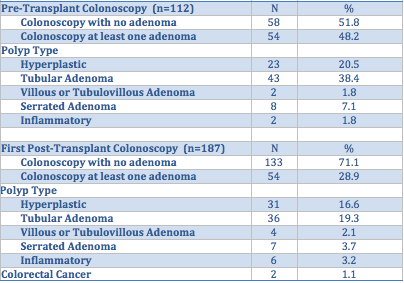
Figure: Table 2: Pre and Post-Transplant Colonoscopy Findings. Adenoma consisted of tubular, villous or tubulovillous, serrated adenomas, or polyps ≥ 10mm.
Disclosures:
Tara Alleyasin indicated no relevant financial relationships.
Sang Hee Choi indicated no relevant financial relationships.
Jeffrey Nguyen indicated no relevant financial relationships.
Nabil El Hage Chehade indicated no relevant financial relationships.
Merveille Kouka indicated no relevant financial relationships.
Jennifer Au indicated no relevant financial relationships.
Tara Alleyasin, MD1, Sang Hee Choi, MD1, Jeffrey Nguyen, MD2, Nabil El Hage Chehade, MD1, Merveille Kouka, BS3, Jennifer Au, MD1. P2615 - Colorectal Cancer Screening Outcomes in Renal Transplant Recipients: A Single Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
