Monday Poster Session
Category: Colon
P2598 - An Unusual Case of Right-Sided Abdominal Pain: Rare Appendiceal Schwann Cell Hamartoma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ES
Emma Schnittka, DO
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Emma Schnittka, DO1, Mark Russell, MD2, Promila Banerjee, MD, FACG2
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL
Introduction: Mucosal Schwann cell hamartomas (MSCHs) are rare, benign lesions of the gastrointestinal (GI) tract. Since first described in 2009, they have been documented in only a few case reports. Most commonly, MSCHs are found incidentally during colonoscopy in the distal colon, typically in asymptomatic, older adults. This case report details a unique clinical presentation and location of MSCH, aiming to contribute to the growing understanding of these rare lesions.
Case Description/
Methods: A 39-year-old male with a history of hyperlipidemia and partial nephrectomy for a benign renal mass presented to GI clinic with a year-long history of dull RLQ pain. Previous workup included an abdominal ultrasound and X-ray, notable for hepatic steatosis and mild-to-moderate stool burden, respectively. Laxative therapy had been recommended. Despite improved bowel movements, pain persisted, prompting GI referral. On interview, the patient noted intermittent pain, not associated with eating, improved with bowel movements. He also endorsed bloating, variable bowel habits, and incomplete evacuation, but no constitutional symptoms or signs of bleeding. Physical exam was unremarkable. Labs were notable for elevated ALT (121) and AST (40). CT imaging was recommended, exhibiting hepatic steatosis and a 2.2 cm dilated tubular RLQ structure concerning for appendiceal mucocele (Figure 1). General surgery was consulted, and the patient underwent robotic-assisted appendectomy. Pathology revealed a mucosal-based proliferation of S-100-postive spindle cells, consistent with MSCH (Figure 2). Postoperatively, his pain resolved without recurrence.
Discussion: Due to limited available literature, MSCHs remain poorly understood. Though commonly identified in the distal colon, detection in the rectum, gallbladder, gastroesophageal junction, and duodenum has also been reported. This is the first report of MSCH presenting as a symptomatic appendiceal mucocele with resolution of symptoms following surgical resection. MSCHs must be distinguished from other GI tumors including GIST, leiomyomas, mucosal neuromas, and neurofibromas—some of which are associated with genetic syndromes or may require aggressive management. Surveillance guidelines for these lesions have not been defined. This case emphasizes the need for a higher index of suspicion to improve detection of MSCH. Further research is needed to clarify the optimal approach to diagnosis and management of MSCH to avoid unnecessary interventions and ensure appropriate patient care.

Figure: Figure 1: Appendiceal mucocele (blue arrow) noted on CT abdomen and pelvis.
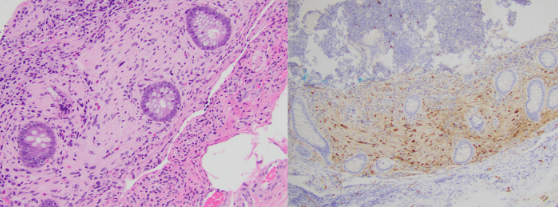
Figure: Figure 2: Histologic features of the excised appendix. (Left) H&E x100 exhibiting fibrofatty obliteration with mucosal proliferation and (right) immunohistochemistry x100 with S-100-postive spindle cells, diagnostic of mucosal Schwann Cell hamartoma (MSCH).
Disclosures:
Emma Schnittka indicated no relevant financial relationships.
Mark Russell indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Emma Schnittka, DO1, Mark Russell, MD2, Promila Banerjee, MD, FACG2. P2598 - An Unusual Case of Right-Sided Abdominal Pain: Rare Appendiceal Schwann Cell Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL
Introduction: Mucosal Schwann cell hamartomas (MSCHs) are rare, benign lesions of the gastrointestinal (GI) tract. Since first described in 2009, they have been documented in only a few case reports. Most commonly, MSCHs are found incidentally during colonoscopy in the distal colon, typically in asymptomatic, older adults. This case report details a unique clinical presentation and location of MSCH, aiming to contribute to the growing understanding of these rare lesions.
Case Description/
Methods: A 39-year-old male with a history of hyperlipidemia and partial nephrectomy for a benign renal mass presented to GI clinic with a year-long history of dull RLQ pain. Previous workup included an abdominal ultrasound and X-ray, notable for hepatic steatosis and mild-to-moderate stool burden, respectively. Laxative therapy had been recommended. Despite improved bowel movements, pain persisted, prompting GI referral. On interview, the patient noted intermittent pain, not associated with eating, improved with bowel movements. He also endorsed bloating, variable bowel habits, and incomplete evacuation, but no constitutional symptoms or signs of bleeding. Physical exam was unremarkable. Labs were notable for elevated ALT (121) and AST (40). CT imaging was recommended, exhibiting hepatic steatosis and a 2.2 cm dilated tubular RLQ structure concerning for appendiceal mucocele (Figure 1). General surgery was consulted, and the patient underwent robotic-assisted appendectomy. Pathology revealed a mucosal-based proliferation of S-100-postive spindle cells, consistent with MSCH (Figure 2). Postoperatively, his pain resolved without recurrence.
Discussion: Due to limited available literature, MSCHs remain poorly understood. Though commonly identified in the distal colon, detection in the rectum, gallbladder, gastroesophageal junction, and duodenum has also been reported. This is the first report of MSCH presenting as a symptomatic appendiceal mucocele with resolution of symptoms following surgical resection. MSCHs must be distinguished from other GI tumors including GIST, leiomyomas, mucosal neuromas, and neurofibromas—some of which are associated with genetic syndromes or may require aggressive management. Surveillance guidelines for these lesions have not been defined. This case emphasizes the need for a higher index of suspicion to improve detection of MSCH. Further research is needed to clarify the optimal approach to diagnosis and management of MSCH to avoid unnecessary interventions and ensure appropriate patient care.

Figure: Figure 1: Appendiceal mucocele (blue arrow) noted on CT abdomen and pelvis.
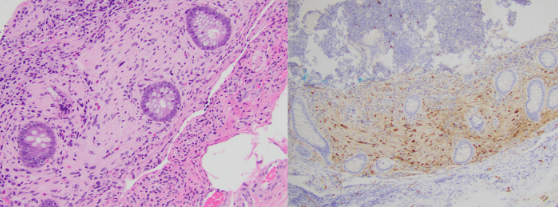
Figure: Figure 2: Histologic features of the excised appendix. (Left) H&E x100 exhibiting fibrofatty obliteration with mucosal proliferation and (right) immunohistochemistry x100 with S-100-postive spindle cells, diagnostic of mucosal Schwann Cell hamartoma (MSCH).
Disclosures:
Emma Schnittka indicated no relevant financial relationships.
Mark Russell indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Emma Schnittka, DO1, Mark Russell, MD2, Promila Banerjee, MD, FACG2. P2598 - An Unusual Case of Right-Sided Abdominal Pain: Rare Appendiceal Schwann Cell Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
