Monday Poster Session
Category: Colon
P2596 - A Rare Case of Idiopathic Myointimal Hyperplasia of Mesenteric Veins Veiled as Inflammatory Bowel Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
David L. Hobby, MD (he/him/his)
Atrium Health Navicent
Atlanta, GA
Presenting Author(s)
David L. Hobby, MD1, Fadi Chanaa, MD2, Carl Jacobs, MD2, Mitchell Arbogast, MD2, Lynn Schiffern, MD2, Jennifer Wellington, DO2
1Atrium Health Navicent, Macon, GA; 2Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Idiopathic myointimal hyperplasia of mesenteric veins (IMHMV), often misdiagnosed as inflammatory bowel disease (IBD), requires meticulous histopathologic analysis of the mesenteric vessel sampling, as early findings may be nonspecific.
Case Description/
Methods: A 68-year-old man with a remote history of Crohn’s disease presented with intractable abdominal pain and intermittent diarrhea. Initial work-up revealed a Norovirus positive stool sample, elevated CRP of 3.4 mg/dL, low calprotectin; CT abdomen/pelvis with contrast noted descending and rectosigmoid colonic wall thickening with stranding concerning for undifferentiated colitis (Fig. 1A). These findings mirrored a similar episode six months prior that temporarily improved with supportive care. However, Norovirus did not explain the chronicity of his symptoms. Thus, inpatient colonoscopy was pursued which noted erythematous, friable, ulcerative mucosa in the left colon suspicious for severe acute on chronic IBD (Fig. 1B). Empiric Solumedrol 60 mg IV was initiated for suspected IBD; however, biopsies described active ischemic changes. CT Angiography abdomen/pelvis noted completely patent mesenteric vasculature. Despite 5 days of treatment, symptoms were unchanged, and CRP and calprotectin cyclically rose. Because of suspicion for ischemia, steroids were ultimately discontinued. A repeat flexible sigmoidoscopy noted interval improvement with healing distal rectal mucosa and improved edematous mucosa of the descending and sigmoid colon more consistent with resolving ischemia (Fig. 1C). Unfortunately, his pain regimen, peaking at 80 MME/day, was disproportionate to the mild physical exam findings. For completion, a third colonoscopy with deeper bite biopsies was performed on Hospital Day 29 highlighting dusky, necrotic, sloughing tissue from 18 to 55 cm with preserved right colonic mucosa (Fig. 2A, 2B). These pathology results were consistent with IMHMV based on the pattern of circumferential fibrin deposition and thrombus formation in the lamina propria vessels (Fig. 2C, 2D). Colorectal surgery ultimately performed a left hemicolectomy on Hospital Day 31 with concern for necrotic bowel. Post-operative course was uncomplicated, and the patient was discharged on Hospital Day 40.
Discussion: Non-specific biopsies in suspected insidious courses of IBD with persistent painful proctosigmoiditis should raise suspicion for IMHMV. Increased awareness and early recognition may reduce hospital stays, symptom duration, and ineffective steroid use.
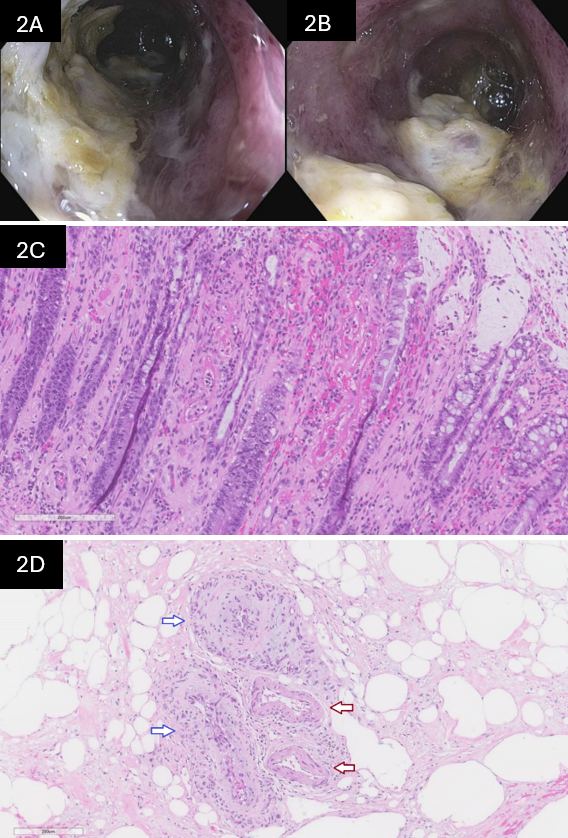
Figure: Figure 1A: Initial computed tomography abdomen pelvis with contrast coronal view noting marked wall thickening and mural edema of the rectum, sigmoid, and descending colon compatible with ongoing proctocolitis. 1B: Initial flexible sigmoidoscopy displays the gross examination of the severe, continuous inflammation up to at least 25 cm. 1C: Follow-up flexible sigmoidoscopy with slight interval improvement yet persistent edematous, friable mucosa; suggestive of resolving colitis.
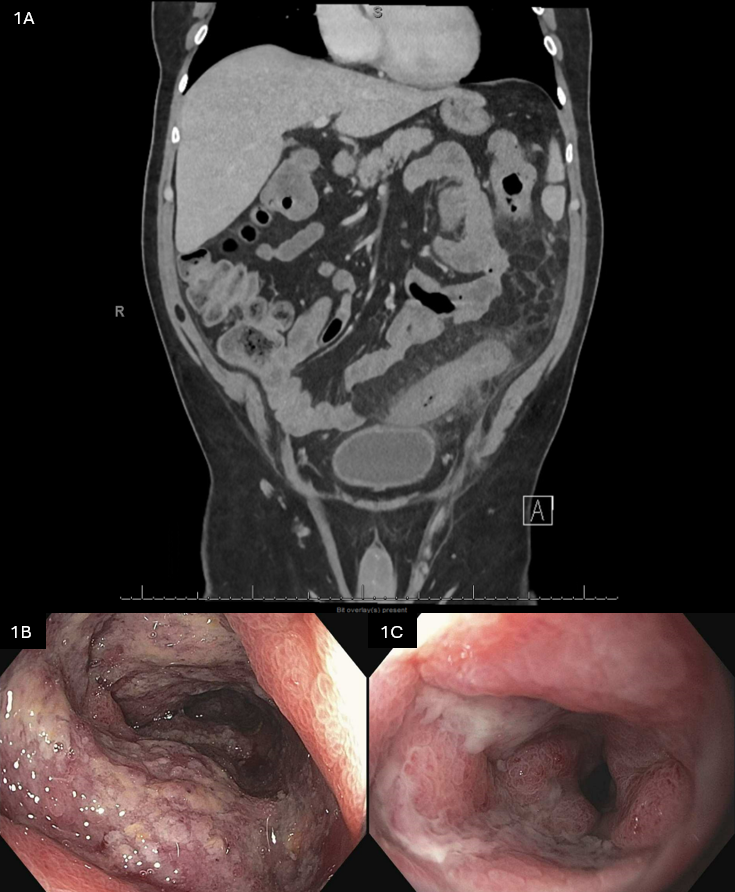
Figure: Figure 2A, 2B: Colonoscopy gross visualization noting the most severe example of edematous, erythematous, friable, hemorrhagic, ulcerated mucosa with loss of folds and pallor in the splenic flexure. 2C: High power image of mucosal ischemic-type injury demonstrating thick-walled abnormal capillaries in the lamina propria, classic presentation of IMHMV. 2D: Mesentery from resection specimen - two vein profiles with defined intimal hyperplasia (blue arrows) as well as two arterial profiles (red arrows).
Disclosures:
David Hobby indicated no relevant financial relationships.
Fadi Chanaa indicated no relevant financial relationships.
Carl Jacobs indicated no relevant financial relationships.
Mitchell Arbogast indicated no relevant financial relationships.
Lynn Schiffern indicated no relevant financial relationships.
Jennifer Wellington indicated no relevant financial relationships.
David L. Hobby, MD1, Fadi Chanaa, MD2, Carl Jacobs, MD2, Mitchell Arbogast, MD2, Lynn Schiffern, MD2, Jennifer Wellington, DO2. P2596 - A Rare Case of Idiopathic Myointimal Hyperplasia of Mesenteric Veins Veiled as Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Atrium Health Navicent, Macon, GA; 2Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Idiopathic myointimal hyperplasia of mesenteric veins (IMHMV), often misdiagnosed as inflammatory bowel disease (IBD), requires meticulous histopathologic analysis of the mesenteric vessel sampling, as early findings may be nonspecific.
Case Description/
Methods: A 68-year-old man with a remote history of Crohn’s disease presented with intractable abdominal pain and intermittent diarrhea. Initial work-up revealed a Norovirus positive stool sample, elevated CRP of 3.4 mg/dL, low calprotectin; CT abdomen/pelvis with contrast noted descending and rectosigmoid colonic wall thickening with stranding concerning for undifferentiated colitis (Fig. 1A). These findings mirrored a similar episode six months prior that temporarily improved with supportive care. However, Norovirus did not explain the chronicity of his symptoms. Thus, inpatient colonoscopy was pursued which noted erythematous, friable, ulcerative mucosa in the left colon suspicious for severe acute on chronic IBD (Fig. 1B). Empiric Solumedrol 60 mg IV was initiated for suspected IBD; however, biopsies described active ischemic changes. CT Angiography abdomen/pelvis noted completely patent mesenteric vasculature. Despite 5 days of treatment, symptoms were unchanged, and CRP and calprotectin cyclically rose. Because of suspicion for ischemia, steroids were ultimately discontinued. A repeat flexible sigmoidoscopy noted interval improvement with healing distal rectal mucosa and improved edematous mucosa of the descending and sigmoid colon more consistent with resolving ischemia (Fig. 1C). Unfortunately, his pain regimen, peaking at 80 MME/day, was disproportionate to the mild physical exam findings. For completion, a third colonoscopy with deeper bite biopsies was performed on Hospital Day 29 highlighting dusky, necrotic, sloughing tissue from 18 to 55 cm with preserved right colonic mucosa (Fig. 2A, 2B). These pathology results were consistent with IMHMV based on the pattern of circumferential fibrin deposition and thrombus formation in the lamina propria vessels (Fig. 2C, 2D). Colorectal surgery ultimately performed a left hemicolectomy on Hospital Day 31 with concern for necrotic bowel. Post-operative course was uncomplicated, and the patient was discharged on Hospital Day 40.
Discussion: Non-specific biopsies in suspected insidious courses of IBD with persistent painful proctosigmoiditis should raise suspicion for IMHMV. Increased awareness and early recognition may reduce hospital stays, symptom duration, and ineffective steroid use.
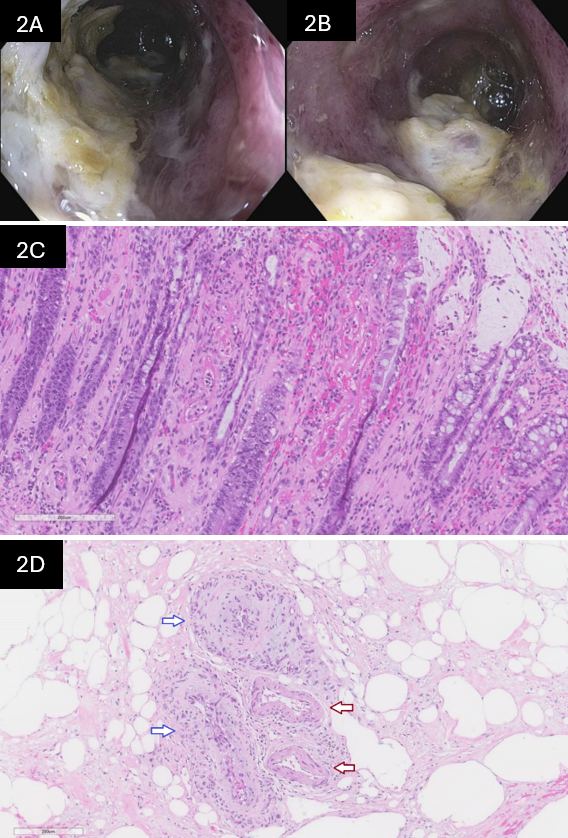
Figure: Figure 1A: Initial computed tomography abdomen pelvis with contrast coronal view noting marked wall thickening and mural edema of the rectum, sigmoid, and descending colon compatible with ongoing proctocolitis. 1B: Initial flexible sigmoidoscopy displays the gross examination of the severe, continuous inflammation up to at least 25 cm. 1C: Follow-up flexible sigmoidoscopy with slight interval improvement yet persistent edematous, friable mucosa; suggestive of resolving colitis.
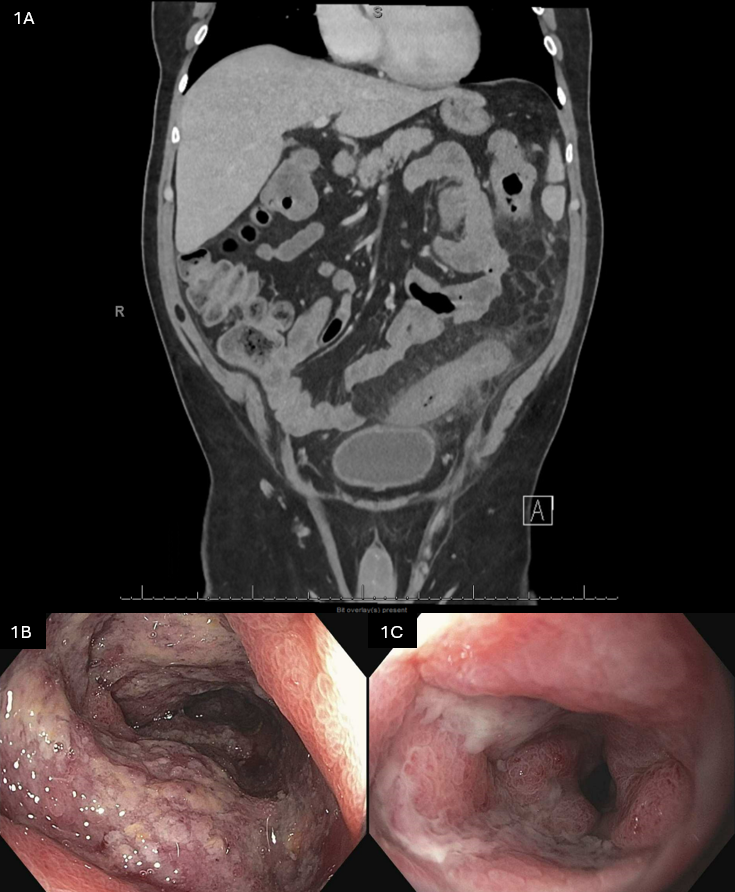
Figure: Figure 2A, 2B: Colonoscopy gross visualization noting the most severe example of edematous, erythematous, friable, hemorrhagic, ulcerated mucosa with loss of folds and pallor in the splenic flexure. 2C: High power image of mucosal ischemic-type injury demonstrating thick-walled abnormal capillaries in the lamina propria, classic presentation of IMHMV. 2D: Mesentery from resection specimen - two vein profiles with defined intimal hyperplasia (blue arrows) as well as two arterial profiles (red arrows).
Disclosures:
David Hobby indicated no relevant financial relationships.
Fadi Chanaa indicated no relevant financial relationships.
Carl Jacobs indicated no relevant financial relationships.
Mitchell Arbogast indicated no relevant financial relationships.
Lynn Schiffern indicated no relevant financial relationships.
Jennifer Wellington indicated no relevant financial relationships.
David L. Hobby, MD1, Fadi Chanaa, MD2, Carl Jacobs, MD2, Mitchell Arbogast, MD2, Lynn Schiffern, MD2, Jennifer Wellington, DO2. P2596 - A Rare Case of Idiopathic Myointimal Hyperplasia of Mesenteric Veins Veiled as Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
