Monday Poster Session
Category: Biliary/Pancreas
P2356 - Unmasking Mirizzi Syndrome: A Case Study of Malignancy Mimicry and Infectious Complications Post-ERCP and Subtotal Fenestrating Cholecystectomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Wilfredo J. Javier-Rojas, MD
HCA Florida Blake Hospital
Bradenton, FL
Presenting Author(s)
Wilfredo J.. Javier-Rojas, MD1, Vamsee Mupparaju, MD2, Douglas M.. Rivera-Agosto, MD1, Yizhi Lin, DO1
1HCA Florida Blake Hospital, Bradenton, FL; 2HCA Florida Citrus Hospital, Inverness, FL
Introduction: Mirizzi Syndrome is a rare complication of cholelithiasis, characterized by impaction of a gallstone in the cystic duct or Hartmann’s pouch, causing external compression of the common hepatic duct (CHD) or common bile duct (CBD). Its clinical and radiologic overlap with biliary malignancies, especially in the setting of elevated tumor markers like CA 19-9, makes diagnosis challenging. Definitive treatment is often surgical, with potential for rare complications such as biloma—an encapsulated bile collection outside the biliary system, often iatrogenic following interventions like cholecystectomy or ERCP.
Case Description/
Methods: A 53-year-old female with non-insulin dependent type II diabetes mellitus presented with four days of nausea, vomiting, fever, and epigastric pain, alongside two months of unintentional weight loss. Labs showed elevated liver enzymes (AST 1792, ALT 1098, ALP 767), a GGT of 922, and CA 19-9 of 114 U/mL. Initial CT A/P (Figure 1A) raised concern for a biliary system tumor. MRCP (Figure 1B) revealed intra and extrahepatic biliary dilation and a distended cystic duct with a 9mm stone compressing the CBD, suggestive of Mirizzi Syndrome. ERCP with CBD stenting and subsequent robotic-assisted cholecystectomy were performed. Intraoperative findings necessitated subtotal fenestrating cholecystectomy with indocyanine green (ICG) cholangiography due to inflammation and anatomic distortion.
Seven weeks post-stent removal, the patient was readmitted with sepsis, RUQ pain, and LFTs derangements. CT A/P and RUQ US (Figure 2A-C) revealed a biloma in the gallbladder fossa. Percutaneous drainage (Figure 2D) yielded 200 mL of bile, positive for Klebsiella pneumoniae. Due to rising LFTs and CBD dilation on the CT A/P, repeat ERCP confirmed and removed a retained stone. The biloma resolved, and the patient was discharged on oral antibiotics with planned surgical follow-up.
Discussion: Mirizzi Syndrome poses diagnostic difficulty due to its mimicry of malignancy on imaging and CA 19-9 elevation, which may also occur in benign biliary obstruction. MRCP and ERCP are essential in diagnosis, with ERCP being the gold standard. Surgical management depends on disease severity; in this case, distorted anatomy required a tailored approach. Bilomas are rare post-intervention complications that can become infected, compounding morbidity. Prompt recognition and multidisciplinary management with percutaneous drainage, antibiotics, and repeat ERCP (if persistent) are key to favorable outcomes.
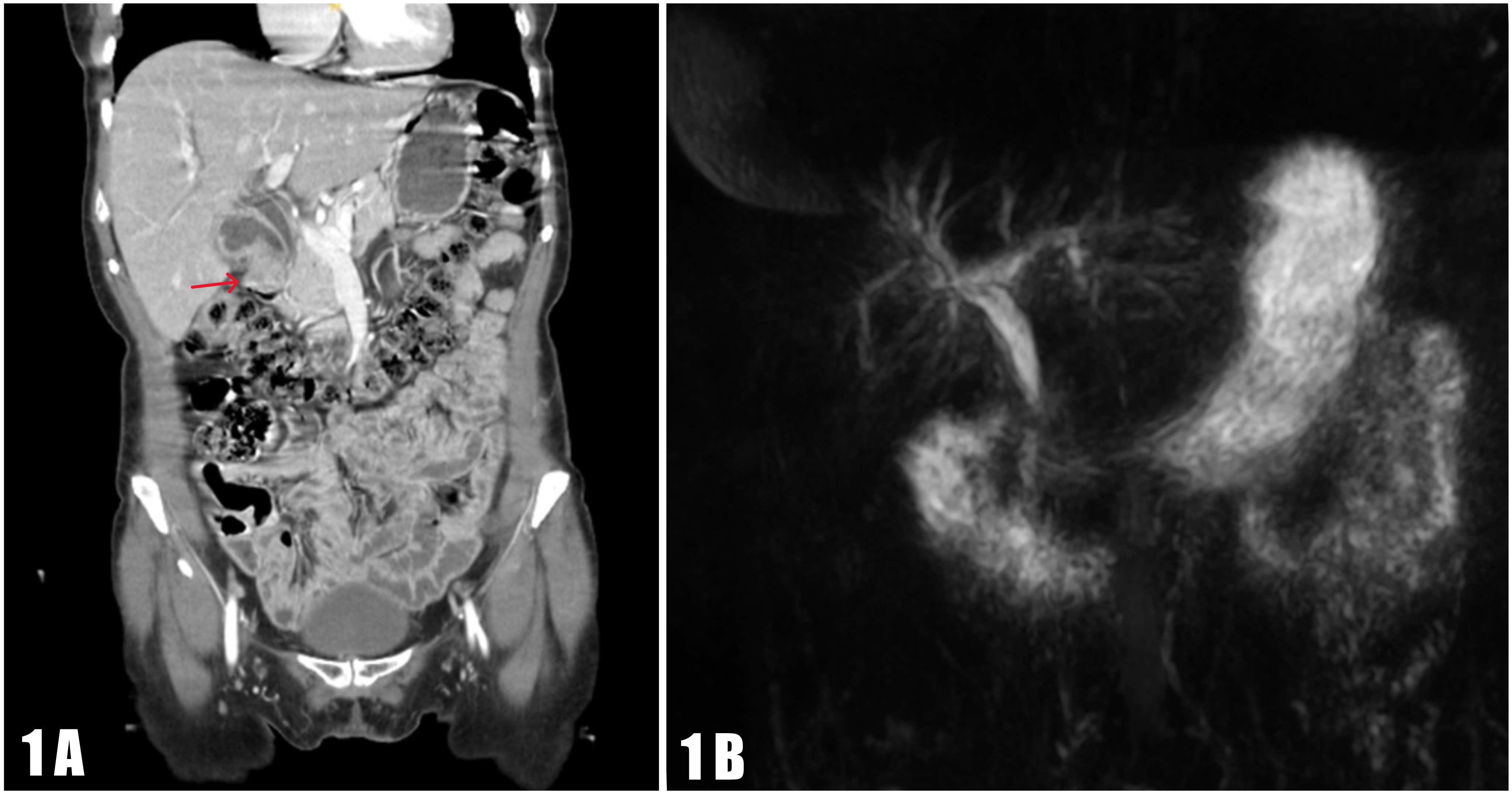
Figure: Figure 1A. Contrast-enhanced CT A/P showing mild intrahepatic biliary dilation and an abnormal gallbladder with irregular wall thickening and enhancement concerning for tumor (red arrow). The cystic duct (7.6 mm), hepatic duct (10 mm), and common bile duct are dilated; the distal common bile duct appeared normal in caliber (not clearly visualized on this image). The cystic duct arises from a relatively low origin.
Figure 1B. MRCP showing intra- and extrahepatic biliary dilation with a dilated common bile duct (8 mm) compressed distally by a distended, low-origin cystic duct. A 9 mm filling defect within the cystic duct suggests a distal stone. Findings are consistent with Mirizzi Syndrome.
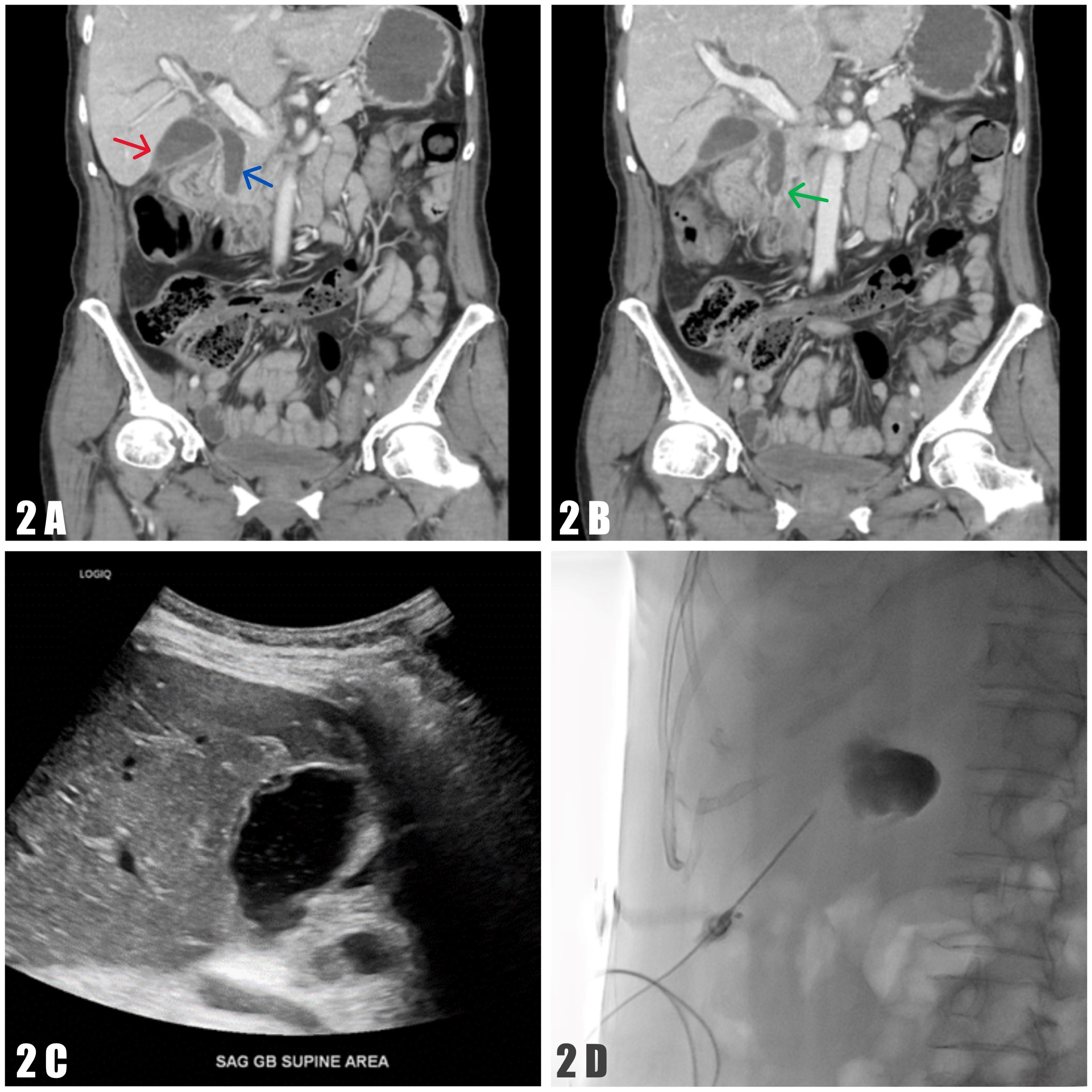
Figure: Figure 2A. Contrast-enhanced CT A/P showing a fluid collection in the gallbladder fossa suggestive of a biloma (red arrow), with biliary obstruction and dilated intra- and extrahepatic ducts. The common bile duct measures 12 mm (blue arrow).
Figure 2B. Contrast-enhanced CT A/P showing a 2 mm filling defect and wall thickening in the distal common bile duct (green arrow).
Figure 2C. RUQ ultrasound showing a complex fluid collection in the gallbladder fossa measuring 5.1 × 3.2 × 3.2 cm, consistent with a biloma.
Figure 2D. Ultrasound-guided, fluoroscopy-assisted percutaneous biloma drainage.
Disclosures:
Wilfredo Javier-Rojas indicated no relevant financial relationships.
Vamsee Mupparaju indicated no relevant financial relationships.
Douglas Rivera-Agosto indicated no relevant financial relationships.
Yizhi Lin indicated no relevant financial relationships.
Wilfredo J.. Javier-Rojas, MD1, Vamsee Mupparaju, MD2, Douglas M.. Rivera-Agosto, MD1, Yizhi Lin, DO1. P2356 - Unmasking Mirizzi Syndrome: A Case Study of Malignancy Mimicry and Infectious Complications Post-ERCP and Subtotal Fenestrating Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Florida Blake Hospital, Bradenton, FL; 2HCA Florida Citrus Hospital, Inverness, FL
Introduction: Mirizzi Syndrome is a rare complication of cholelithiasis, characterized by impaction of a gallstone in the cystic duct or Hartmann’s pouch, causing external compression of the common hepatic duct (CHD) or common bile duct (CBD). Its clinical and radiologic overlap with biliary malignancies, especially in the setting of elevated tumor markers like CA 19-9, makes diagnosis challenging. Definitive treatment is often surgical, with potential for rare complications such as biloma—an encapsulated bile collection outside the biliary system, often iatrogenic following interventions like cholecystectomy or ERCP.
Case Description/
Methods: A 53-year-old female with non-insulin dependent type II diabetes mellitus presented with four days of nausea, vomiting, fever, and epigastric pain, alongside two months of unintentional weight loss. Labs showed elevated liver enzymes (AST 1792, ALT 1098, ALP 767), a GGT of 922, and CA 19-9 of 114 U/mL. Initial CT A/P (Figure 1A) raised concern for a biliary system tumor. MRCP (Figure 1B) revealed intra and extrahepatic biliary dilation and a distended cystic duct with a 9mm stone compressing the CBD, suggestive of Mirizzi Syndrome. ERCP with CBD stenting and subsequent robotic-assisted cholecystectomy were performed. Intraoperative findings necessitated subtotal fenestrating cholecystectomy with indocyanine green (ICG) cholangiography due to inflammation and anatomic distortion.
Seven weeks post-stent removal, the patient was readmitted with sepsis, RUQ pain, and LFTs derangements. CT A/P and RUQ US (Figure 2A-C) revealed a biloma in the gallbladder fossa. Percutaneous drainage (Figure 2D) yielded 200 mL of bile, positive for Klebsiella pneumoniae. Due to rising LFTs and CBD dilation on the CT A/P, repeat ERCP confirmed and removed a retained stone. The biloma resolved, and the patient was discharged on oral antibiotics with planned surgical follow-up.
Discussion: Mirizzi Syndrome poses diagnostic difficulty due to its mimicry of malignancy on imaging and CA 19-9 elevation, which may also occur in benign biliary obstruction. MRCP and ERCP are essential in diagnosis, with ERCP being the gold standard. Surgical management depends on disease severity; in this case, distorted anatomy required a tailored approach. Bilomas are rare post-intervention complications that can become infected, compounding morbidity. Prompt recognition and multidisciplinary management with percutaneous drainage, antibiotics, and repeat ERCP (if persistent) are key to favorable outcomes.
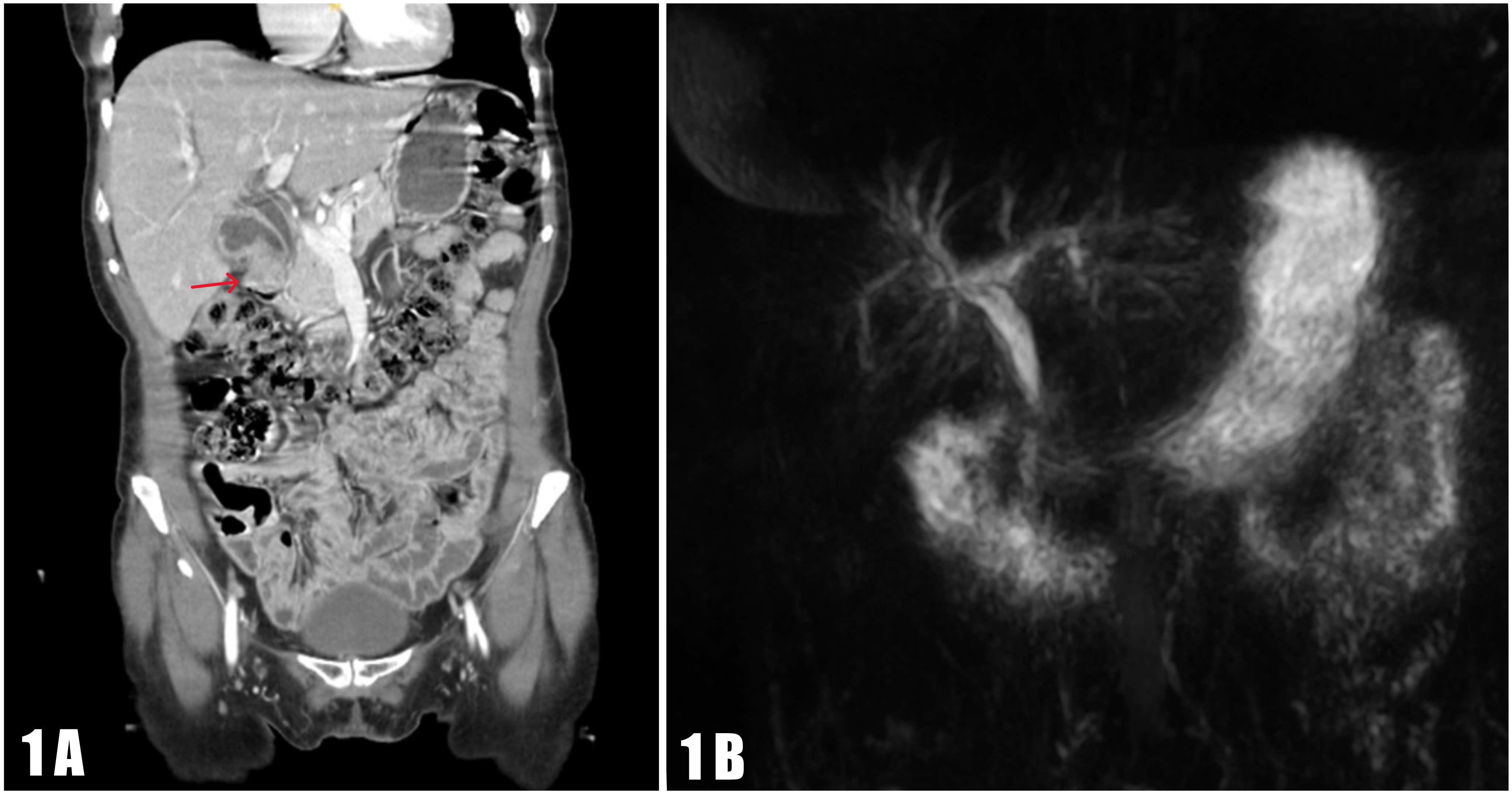
Figure: Figure 1A. Contrast-enhanced CT A/P showing mild intrahepatic biliary dilation and an abnormal gallbladder with irregular wall thickening and enhancement concerning for tumor (red arrow). The cystic duct (7.6 mm), hepatic duct (10 mm), and common bile duct are dilated; the distal common bile duct appeared normal in caliber (not clearly visualized on this image). The cystic duct arises from a relatively low origin.
Figure 1B. MRCP showing intra- and extrahepatic biliary dilation with a dilated common bile duct (8 mm) compressed distally by a distended, low-origin cystic duct. A 9 mm filling defect within the cystic duct suggests a distal stone. Findings are consistent with Mirizzi Syndrome.
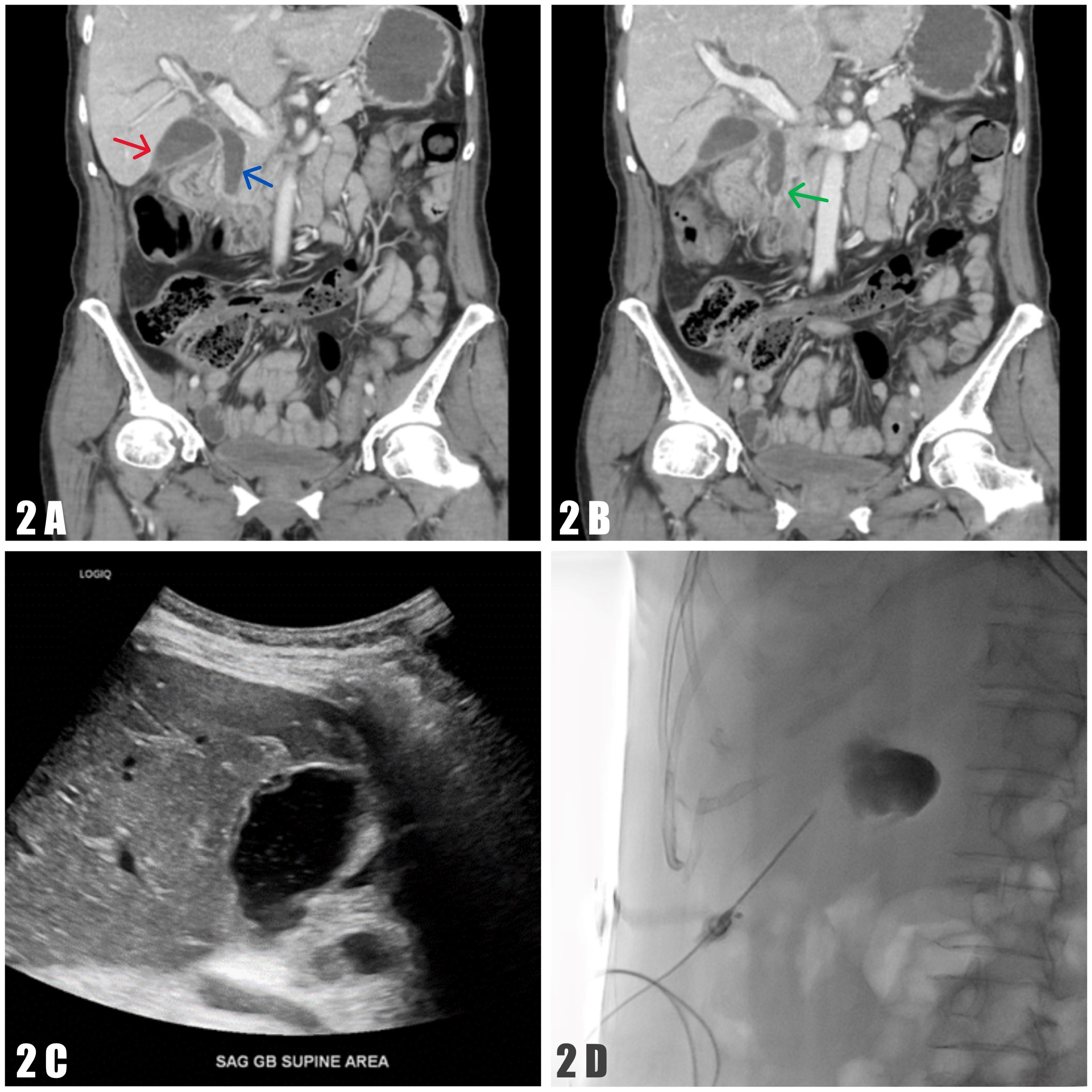
Figure: Figure 2A. Contrast-enhanced CT A/P showing a fluid collection in the gallbladder fossa suggestive of a biloma (red arrow), with biliary obstruction and dilated intra- and extrahepatic ducts. The common bile duct measures 12 mm (blue arrow).
Figure 2B. Contrast-enhanced CT A/P showing a 2 mm filling defect and wall thickening in the distal common bile duct (green arrow).
Figure 2C. RUQ ultrasound showing a complex fluid collection in the gallbladder fossa measuring 5.1 × 3.2 × 3.2 cm, consistent with a biloma.
Figure 2D. Ultrasound-guided, fluoroscopy-assisted percutaneous biloma drainage.
Disclosures:
Wilfredo Javier-Rojas indicated no relevant financial relationships.
Vamsee Mupparaju indicated no relevant financial relationships.
Douglas Rivera-Agosto indicated no relevant financial relationships.
Yizhi Lin indicated no relevant financial relationships.
Wilfredo J.. Javier-Rojas, MD1, Vamsee Mupparaju, MD2, Douglas M.. Rivera-Agosto, MD1, Yizhi Lin, DO1. P2356 - Unmasking Mirizzi Syndrome: A Case Study of Malignancy Mimicry and Infectious Complications Post-ERCP and Subtotal Fenestrating Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
