Monday Poster Session
Category: Biliary/Pancreas
P2325 - The Novel Complication of Portal Vein Thrombosis After Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Parekh, DO
University of Florida College of Medicine
Jacksonville, FL
Presenting Author(s)
Sneh Parekh, DO, Ty Merry, DO, Vanshika Tripathi, DO, Pramod Reddy, MD
University of Florida College of Medicine, Jacksonville, FL
Introduction: Acute pancreatitis (AP) is a well-known cause of hospitalization and can lead to numerous complications. One such complication is portal vein thrombosis (PVT), which is the obstruction of the portal vein due to a thrombus in the vessel. PVT is a rare complication, occurring in approximately 0.8% of cases. Additionally, the development of PVT in patients without any predisposing risk factors may pose a significant diagnostic challenge and can lead to delays in diagnosis and treatment. Here, we present the case of a patient with no past medical history and no significant risk factors, who insidiously developed PVT after initially being admitted with acute pancreatitis.
Case Description/
Methods: A 40-year-old male with no past medical history presented with the typical epigastric pain seen in pancreatitis. Initial vitals were significant for tachycardia. Blood work revealed transaminitis, with AST and ALT elevation to 478 and 609 IU/L respectively, and an elevated lipase to 384 U/L. A CT abdomen and pelvis (CT AP) revealed acute edematous interstitial pancreatitis with surrounding nonlocalized fluid and fat stranding, after which the patient was admitted. His pain soon resolved with supportive care and bowel rest, and he was tolerating a regular diet until day 4 when he became persistently tachycardic with reemergence of the epigastric pain. Persistent low-grade fevers and leukocytosis prompted an infectious workup with blood cultures that ultimately returned negative. A repeat CT AP then revealed evidence of PVT, for which he was started on apixaban. His tachycardia and epigastric pain soon resolved, and he was discharged on a 3-month course of apixaban with close outpatient follow-up.
Discussion: This case highlights the rare presentation of PVT following AP, a unique phenomenon occurring in about 0.8% of cases. Risk factors for developing PVT after AP include the presence of pancreatic pseudocysts, bacteremia, and cirrhosis, none of which were present in our patient. Additionally, PVT can present insidiously, which can result in worse patient outcomes if not identified and treated appropriately. The presence of fevers, leukocytosis, and tachycardia in our patient, in the absence of obvious infection, prompted repeat imaging, thereby correctly identifying the PVT. For patients without obvious clinical signs or risk factors, and in atypical presentations, repeat imaging may help identify PVT’s, allowing for rapid initiation of anticoagulation, and thereby improving long-term outcomes.

Figure: Figure 1: CT of the abdomen and pelvis obtained on admission, showing acute interstitial edematous pancreatitis, as indicated by the orange arrow.
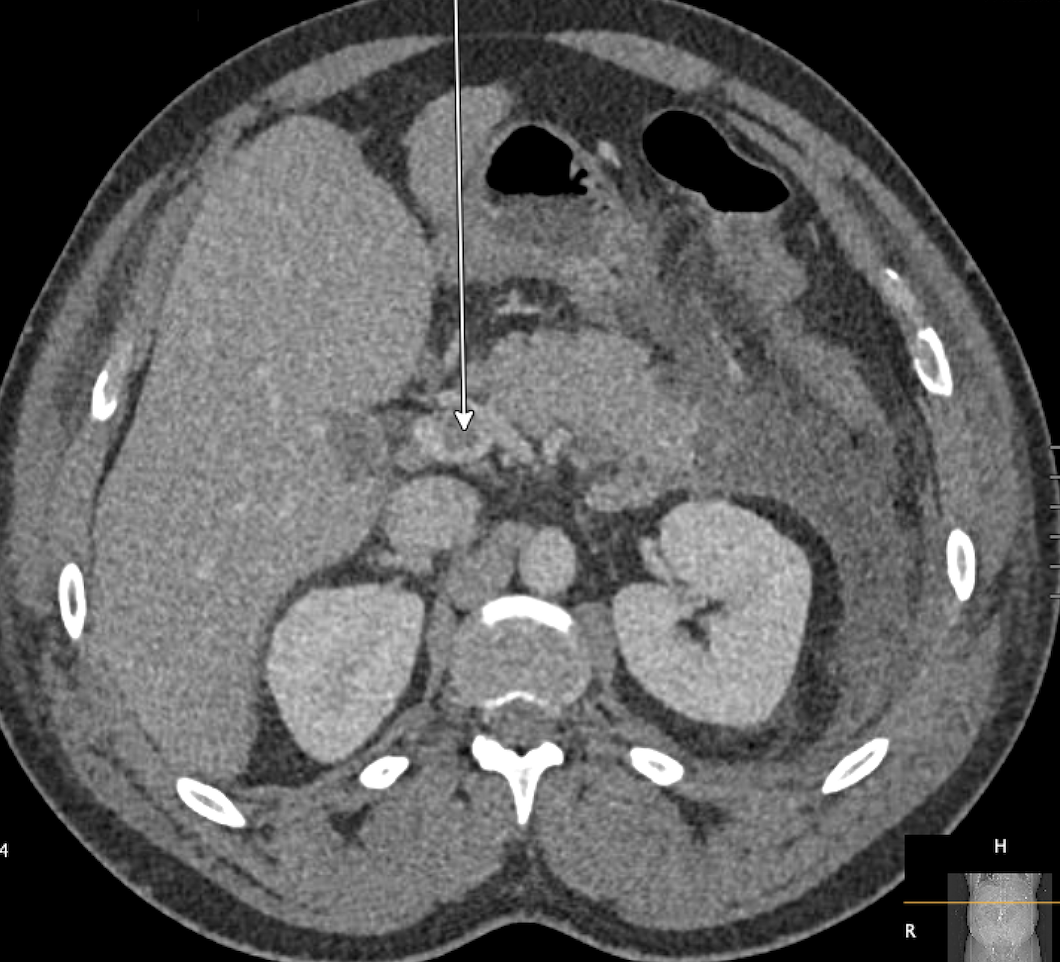
Figure: Figure 2: CT of the abdomen and pelvis with the white arrow indicating the nonocclusive filling defect in the proximal portal vein, consistent with the patient's portal vein thrombosis.
Disclosures:
Sneh Parekh indicated no relevant financial relationships.
Ty Merry indicated no relevant financial relationships.
Vanshika Tripathi indicated no relevant financial relationships.
Pramod Reddy indicated no relevant financial relationships.
Sneh Parekh, DO, Ty Merry, DO, Vanshika Tripathi, DO, Pramod Reddy, MD. P2325 - The Novel Complication of Portal Vein Thrombosis After Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Florida College of Medicine, Jacksonville, FL
Introduction: Acute pancreatitis (AP) is a well-known cause of hospitalization and can lead to numerous complications. One such complication is portal vein thrombosis (PVT), which is the obstruction of the portal vein due to a thrombus in the vessel. PVT is a rare complication, occurring in approximately 0.8% of cases. Additionally, the development of PVT in patients without any predisposing risk factors may pose a significant diagnostic challenge and can lead to delays in diagnosis and treatment. Here, we present the case of a patient with no past medical history and no significant risk factors, who insidiously developed PVT after initially being admitted with acute pancreatitis.
Case Description/
Methods: A 40-year-old male with no past medical history presented with the typical epigastric pain seen in pancreatitis. Initial vitals were significant for tachycardia. Blood work revealed transaminitis, with AST and ALT elevation to 478 and 609 IU/L respectively, and an elevated lipase to 384 U/L. A CT abdomen and pelvis (CT AP) revealed acute edematous interstitial pancreatitis with surrounding nonlocalized fluid and fat stranding, after which the patient was admitted. His pain soon resolved with supportive care and bowel rest, and he was tolerating a regular diet until day 4 when he became persistently tachycardic with reemergence of the epigastric pain. Persistent low-grade fevers and leukocytosis prompted an infectious workup with blood cultures that ultimately returned negative. A repeat CT AP then revealed evidence of PVT, for which he was started on apixaban. His tachycardia and epigastric pain soon resolved, and he was discharged on a 3-month course of apixaban with close outpatient follow-up.
Discussion: This case highlights the rare presentation of PVT following AP, a unique phenomenon occurring in about 0.8% of cases. Risk factors for developing PVT after AP include the presence of pancreatic pseudocysts, bacteremia, and cirrhosis, none of which were present in our patient. Additionally, PVT can present insidiously, which can result in worse patient outcomes if not identified and treated appropriately. The presence of fevers, leukocytosis, and tachycardia in our patient, in the absence of obvious infection, prompted repeat imaging, thereby correctly identifying the PVT. For patients without obvious clinical signs or risk factors, and in atypical presentations, repeat imaging may help identify PVT’s, allowing for rapid initiation of anticoagulation, and thereby improving long-term outcomes.

Figure: Figure 1: CT of the abdomen and pelvis obtained on admission, showing acute interstitial edematous pancreatitis, as indicated by the orange arrow.
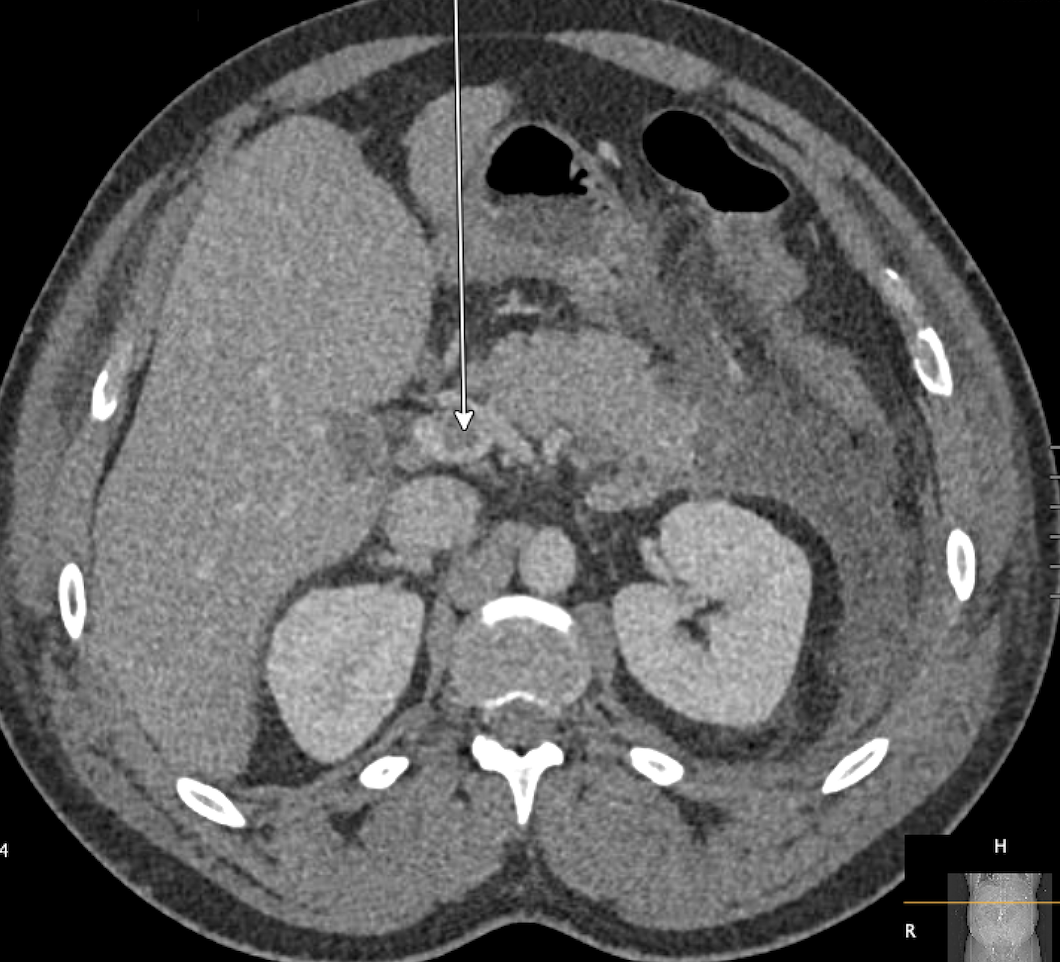
Figure: Figure 2: CT of the abdomen and pelvis with the white arrow indicating the nonocclusive filling defect in the proximal portal vein, consistent with the patient's portal vein thrombosis.
Disclosures:
Sneh Parekh indicated no relevant financial relationships.
Ty Merry indicated no relevant financial relationships.
Vanshika Tripathi indicated no relevant financial relationships.
Pramod Reddy indicated no relevant financial relationships.
Sneh Parekh, DO, Ty Merry, DO, Vanshika Tripathi, DO, Pramod Reddy, MD. P2325 - The Novel Complication of Portal Vein Thrombosis After Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
