Monday Poster Session
Category: Biliary/Pancreas
P2323 - Cholecystoenteric Fistula Presenting with Acute Cholecystitis and Acute Diverticulitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Faizan Ahmed, MD (he/him/his)
HCA Florida Healthcare
Clearwater, FL
Presenting Author(s)
Faizan Ahmed, MD1, Nimal Patel, DO1, Patrick Stocker, PhD2, Olugbenga Oyesanmi, MD2
1HCA Florida Healthcare, Clearwater, FL; 2HCA Florida Healthcare, Saint Petersburg, FL
Introduction: Cholecystoenteric fistulas complicate 0.4–1.9% of gallstone disease and usually involve the duodenum; colonic fistulas are rarer but more morbid¹. Chronic gallbladder inflammation, pressure necrosis from stones, and adjacent diverticulitis can converge to form a cholecystocolic fistula². Because presentations mimic routine cholecystitis or diverticulitis, cross-sectional imaging is essential for timely diagnosis.
Case Description/
Methods: A 59-year-old man with heavy alcohol and 30-pack-year smoking history had 3 days of right-upper-quadrant pain, nausea, and bilious emesis. Vitals: temperature 38.4°C, heart rate 110, blood pressure 146/86mmHg. Labs: White Blood Cells (WBC) 14.2×10⁹/L, Alanine Aminotransferase (ALT) 67U/L; bilirubin and lipase normal. Computed Tomagraphy (CT) showed a gas-filled, thick-walled gallbladder with pericholecystic fluid plus segmental colonic thickening and fat stranding at the hepatic flexure. Magnetic Resonance Cholangiopancreatography (MRCP) confirmed gas within the gallbladder fundus abutting colon; Hepatobiliary Iminodiacetic Acid Scan (HIDA) failed to visualize the gallbladder. Blood cultures were sterile. Given severe local inflammation and ASA III status, interventional radiology placed a 10-Fr cholecystostomy tube; purulent bile grew amoxicillin-clavulanate–sensitive E. coli. After 2 days of piperacillin-tazobactam he completed oral amoxicillin-clavulanate. Symptoms and leukocytosis resolved, and he was discharged on day 5 with plans for elective cholecystectomy and possible colonic resection.
Discussion: Colonic cholecystoenteric fistulas usually follow long-standing cholelithiasis but may also arise from contiguous diverticulitis³. Pneumobilia or gallbladder gas without instrumentation strongly suggests a fistula⁴. For unstable or high-risk patients, percutaneous cholecystostomy provides rapid source control, decompresses the biliary tree, and lets inflammation subside before definitive surgery, reducing operative risk⁵. This patient’s quick recovery with drainage and culture-directed antibiotics supports the staged approach; elective cholecystectomy with en-bloc fistula takedown or limited colonic resection remains definitive to prevent recurrent infection or gallstone ileus.
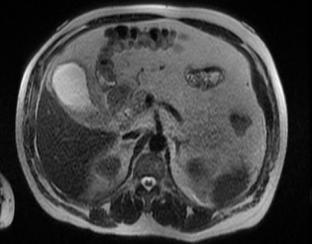
Figure: Figure 1. Gallbladder distention with pericholecystic fat stranding.

Figure: Figure 2. Fluoroscopic-guided placement of a cholecystectomy tube.
Disclosures:
Faizan Ahmed indicated no relevant financial relationships.
Nimal Patel indicated no relevant financial relationships.
Patrick Stocker indicated no relevant financial relationships.
Olugbenga Oyesanmi indicated no relevant financial relationships.
Faizan Ahmed, MD1, Nimal Patel, DO1, Patrick Stocker, PhD2, Olugbenga Oyesanmi, MD2. P2323 - Cholecystoenteric Fistula Presenting with Acute Cholecystitis and Acute Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Florida Healthcare, Clearwater, FL; 2HCA Florida Healthcare, Saint Petersburg, FL
Introduction: Cholecystoenteric fistulas complicate 0.4–1.9% of gallstone disease and usually involve the duodenum; colonic fistulas are rarer but more morbid¹. Chronic gallbladder inflammation, pressure necrosis from stones, and adjacent diverticulitis can converge to form a cholecystocolic fistula². Because presentations mimic routine cholecystitis or diverticulitis, cross-sectional imaging is essential for timely diagnosis.
Case Description/
Methods: A 59-year-old man with heavy alcohol and 30-pack-year smoking history had 3 days of right-upper-quadrant pain, nausea, and bilious emesis. Vitals: temperature 38.4°C, heart rate 110, blood pressure 146/86mmHg. Labs: White Blood Cells (WBC) 14.2×10⁹/L, Alanine Aminotransferase (ALT) 67U/L; bilirubin and lipase normal. Computed Tomagraphy (CT) showed a gas-filled, thick-walled gallbladder with pericholecystic fluid plus segmental colonic thickening and fat stranding at the hepatic flexure. Magnetic Resonance Cholangiopancreatography (MRCP) confirmed gas within the gallbladder fundus abutting colon; Hepatobiliary Iminodiacetic Acid Scan (HIDA) failed to visualize the gallbladder. Blood cultures were sterile. Given severe local inflammation and ASA III status, interventional radiology placed a 10-Fr cholecystostomy tube; purulent bile grew amoxicillin-clavulanate–sensitive E. coli. After 2 days of piperacillin-tazobactam he completed oral amoxicillin-clavulanate. Symptoms and leukocytosis resolved, and he was discharged on day 5 with plans for elective cholecystectomy and possible colonic resection.
Discussion: Colonic cholecystoenteric fistulas usually follow long-standing cholelithiasis but may also arise from contiguous diverticulitis³. Pneumobilia or gallbladder gas without instrumentation strongly suggests a fistula⁴. For unstable or high-risk patients, percutaneous cholecystostomy provides rapid source control, decompresses the biliary tree, and lets inflammation subside before definitive surgery, reducing operative risk⁵. This patient’s quick recovery with drainage and culture-directed antibiotics supports the staged approach; elective cholecystectomy with en-bloc fistula takedown or limited colonic resection remains definitive to prevent recurrent infection or gallstone ileus.
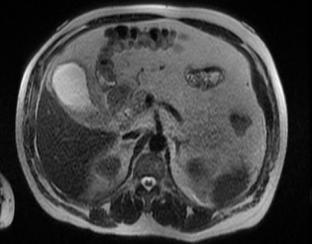
Figure: Figure 1. Gallbladder distention with pericholecystic fat stranding.

Figure: Figure 2. Fluoroscopic-guided placement of a cholecystectomy tube.
Disclosures:
Faizan Ahmed indicated no relevant financial relationships.
Nimal Patel indicated no relevant financial relationships.
Patrick Stocker indicated no relevant financial relationships.
Olugbenga Oyesanmi indicated no relevant financial relationships.
Faizan Ahmed, MD1, Nimal Patel, DO1, Patrick Stocker, PhD2, Olugbenga Oyesanmi, MD2. P2323 - Cholecystoenteric Fistula Presenting with Acute Cholecystitis and Acute Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
