Monday Poster Session
Category: Biliary/Pancreas
Uncommon Culprit in Acute Pancreatitis: Atypical <i>Mycoplasma pneumoniae</i> Presentation Without Respiratory Symptoms
P2284 - Uncommon Culprit in Acute Pancreatitis: Atypical Mycoplasma pneumoniae Presentation Without Respiratory Symptoms
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jennifer John, MS (she/her/hers)
A.T. Still University
Little Falls, NJ
Presenting Author(s)
Jennifer John, MS1, Marielina Garcia, MD2, Anas Al Mardini, MBBS3, Yazmin Rustomji, MD4, Saloni Brahmbhatt, MD2
1A.T. Still University, Little Falls, NJ; 2St. Mary's General Hospital, New York Medical College, Passaic, NJ; 3NYMC at St Mary's and St Clare's, Montclair, NJ; 4Rush University Medical Center, Chicago, IL
Introduction: Mycoplasma pneumoniae is a well-known cause of atypical pneumonia but can also lead to extrapulmonary complications in a notable proportion of cases. These may involve the neurologic, dermatologic, hematologic, and gastrointestinal systems. Among gastrointestinal presentations, pancreatitis is a particularly rare and often overlooked association. This case highlights an unusual presentation of suspected acute pancreatitis related to M. pneumoniae infection in the absence of respiratory symptoms, emphasizing diagnostic challenges and clinical implications.
Case Description/
Methods: A 63-year-old male with no significant medical history presented with two weeks of progressive abdominal pain, nausea, vomiting, chills, and decreased oral intake. He denied alcohol use, recent travel, or sick contacts. He was febrile (100.8°F) with mild epigastric tenderness. Labs revealed AST 177 U/L, ALT 185 U/L, ALP 183 U/L, lipase 246 U/L, and WBC 2.5 K/µL. CT abdomen and MRCP showed hepatic steatosis without pancreatitis or biliary obstruction. Broad infectious (HIV, CMV, SARS-CoV-2, Influenza A/B, malaria, Campylobacter, Shiga toxin, Legionella, fungi, ova/parasites) and autoimmune panels (ANA, dsDNA, SSA/SSB, anti-Scl-70, RNP, Smith, anti-Jo-1, anti-centromere B, AMA) were negative. Despite empiric antibiotics, he remained febrile. On hospital day seven, Mycoplasma pneumoniae IgM returned positive. He was started on azithromycin, then transitioned to doxycycline for suspected macrolide resistance. He defervesced within 48 hours and was discharged with outpatient follow-up.
Discussion: Pancreatitis is an uncommon extrapulmonary manifestation of Mycoplasma pneumoniae, particularly in the absence of respiratory symptoms. Gastrointestinal involvement occurs in approximately 5–8% of extrapulmonary cases, but pancreatitis remains underrecognized. This case underscores the diagnostic challenges and healthcare burden of atypical infections, including delayed diagnosis, prolonged hospitalization, inappropriate antibiotic use, and extensive testing. The absence of radiologic findings despite elevated enzymes and symptoms illustrates how imaging may lag behind biochemical markers in infectious etiologies. Earlier recognition of M. pneumoniae as a potential cause of pancreatitis—even without pulmonary signs—could expedite therapy and reduce morbidity.
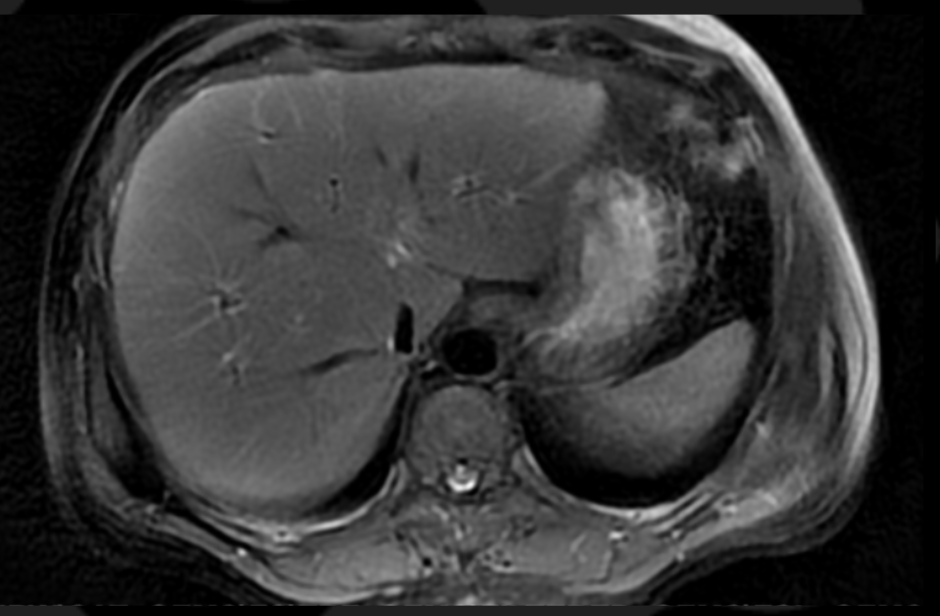
Figure: Magnetic Resonance Cholangiopancreatography
Impression: Liver, spleen, pancreas, adrenal glands, and kidneys show no signal abnormality or enhancement. No cholelithiasis noted

Figure: Non-Contrast CT Abdomen
Impression: No CT evidence of pancreatitis
Disclosures:
Jennifer John indicated no relevant financial relationships.
Marielina Garcia indicated no relevant financial relationships.
Anas Al Mardini indicated no relevant financial relationships.
Yazmin Rustomji indicated no relevant financial relationships.
Saloni Brahmbhatt indicated no relevant financial relationships.
Jennifer John, MS1, Marielina Garcia, MD2, Anas Al Mardini, MBBS3, Yazmin Rustomji, MD4, Saloni Brahmbhatt, MD2. P2284 - Uncommon Culprit in Acute Pancreatitis: Atypical <i>Mycoplasma pneumoniae</i> Presentation Without Respiratory Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1A.T. Still University, Little Falls, NJ; 2St. Mary's General Hospital, New York Medical College, Passaic, NJ; 3NYMC at St Mary's and St Clare's, Montclair, NJ; 4Rush University Medical Center, Chicago, IL
Introduction: Mycoplasma pneumoniae is a well-known cause of atypical pneumonia but can also lead to extrapulmonary complications in a notable proportion of cases. These may involve the neurologic, dermatologic, hematologic, and gastrointestinal systems. Among gastrointestinal presentations, pancreatitis is a particularly rare and often overlooked association. This case highlights an unusual presentation of suspected acute pancreatitis related to M. pneumoniae infection in the absence of respiratory symptoms, emphasizing diagnostic challenges and clinical implications.
Case Description/
Methods: A 63-year-old male with no significant medical history presented with two weeks of progressive abdominal pain, nausea, vomiting, chills, and decreased oral intake. He denied alcohol use, recent travel, or sick contacts. He was febrile (100.8°F) with mild epigastric tenderness. Labs revealed AST 177 U/L, ALT 185 U/L, ALP 183 U/L, lipase 246 U/L, and WBC 2.5 K/µL. CT abdomen and MRCP showed hepatic steatosis without pancreatitis or biliary obstruction. Broad infectious (HIV, CMV, SARS-CoV-2, Influenza A/B, malaria, Campylobacter, Shiga toxin, Legionella, fungi, ova/parasites) and autoimmune panels (ANA, dsDNA, SSA/SSB, anti-Scl-70, RNP, Smith, anti-Jo-1, anti-centromere B, AMA) were negative. Despite empiric antibiotics, he remained febrile. On hospital day seven, Mycoplasma pneumoniae IgM returned positive. He was started on azithromycin, then transitioned to doxycycline for suspected macrolide resistance. He defervesced within 48 hours and was discharged with outpatient follow-up.
Discussion: Pancreatitis is an uncommon extrapulmonary manifestation of Mycoplasma pneumoniae, particularly in the absence of respiratory symptoms. Gastrointestinal involvement occurs in approximately 5–8% of extrapulmonary cases, but pancreatitis remains underrecognized. This case underscores the diagnostic challenges and healthcare burden of atypical infections, including delayed diagnosis, prolonged hospitalization, inappropriate antibiotic use, and extensive testing. The absence of radiologic findings despite elevated enzymes and symptoms illustrates how imaging may lag behind biochemical markers in infectious etiologies. Earlier recognition of M. pneumoniae as a potential cause of pancreatitis—even without pulmonary signs—could expedite therapy and reduce morbidity.
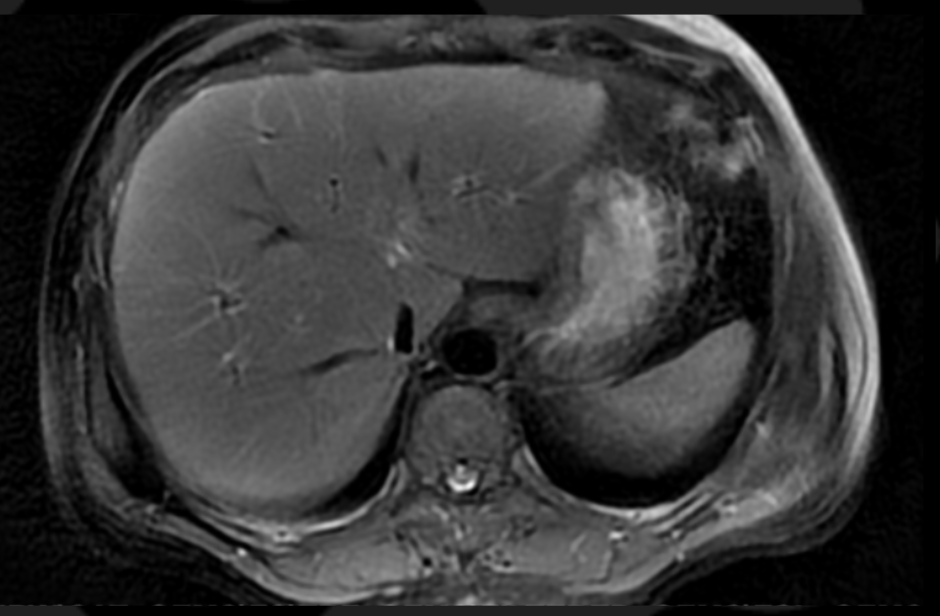
Figure: Magnetic Resonance Cholangiopancreatography
Impression: Liver, spleen, pancreas, adrenal glands, and kidneys show no signal abnormality or enhancement. No cholelithiasis noted

Figure: Non-Contrast CT Abdomen
Impression: No CT evidence of pancreatitis
Disclosures:
Jennifer John indicated no relevant financial relationships.
Marielina Garcia indicated no relevant financial relationships.
Anas Al Mardini indicated no relevant financial relationships.
Yazmin Rustomji indicated no relevant financial relationships.
Saloni Brahmbhatt indicated no relevant financial relationships.
Jennifer John, MS1, Marielina Garcia, MD2, Anas Al Mardini, MBBS3, Yazmin Rustomji, MD4, Saloni Brahmbhatt, MD2. P2284 - Uncommon Culprit in Acute Pancreatitis: Atypical <i>Mycoplasma pneumoniae</i> Presentation Without Respiratory Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
