Monday Poster Session
Category: Biliary/Pancreas
P2276 - Gas and Fluid: Emphysematous Pancreatitis With Pancreatic Ascites as a Sequela of Necrotizing Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Kajol Patel, MD2, Abel Setlhoka, BS3, Praneeth Bandaru, MD1, Yana Cavanagh, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2Florida State University, Paterson, NJ; 3St. George's University, Paterson, NJ
Introduction: Emphysematous pancreatitis (EP) is a rare and fulminant variant of necrotizing pancreatitis characterized by gas-forming bacterial infection of pancreatic tissue. Pancreatic ascites, typically resulting from pancreatic duct disruption or pseudocyst rupture, is an uncommon complication of chronic or severe acute pancreatitis. The coexistence of EP and pancreatic ascites is exceedingly rare and portends a poor prognosis. Herein, we describe a rare case of EP with pancreatic ascites as a sequela of necrotizing pancreatitis.
Case Description/
Methods: A 68-year-old man presented to the ED for acute-onset pleuritic chest pain and dyspnea. The patient was admitted to our hospital a month prior for gallstone pancreatitis that progressed to necrotizing pancreatitis. He was treated with empiric antibiotics, IV fluids, nutrition, and analgesics. ERCP was aborted twice due to severe edema at the ampulla and later deferred due to persistent hypoxemia. Two weeks later, the patient underwent laparoscopic cholecystectomy and was found to have a walled-off pancreatic collection.
During this encounter, the patient was tachypneic and tachycardic, but afebrile. Contrast-enhanced CT of the abdomen and pelvis revealed a new pancreatico-colonic fistula, emphysematous pancreatitis, a walled-off necrosis measuring 10.5 cm x 3.2 cm, a large pleural effusion, and large complex ascites (Figure 1). The patient had a thoracentesis and Pigtail catheter was inserted in the ED for drainage and pleural fluid was exudative in nature. EUS demonstrated intrapancreatic air and calcific material, and diffuse echogenicity of the pancreatic parenchyma (Figure 2). Pancreatic duct could not be visualized due to intrapancreatic air. ERCP revealed pancreatic duct obstruction/stenosis in the genu of the pancreas, and wire, spyglass and contrast could not be extended beyond that point. One plastic stent was placed into the ventral pancreatic duct. Given his functional status and need for continued invasive procedures, the patient opted for hospice care.
Discussion: The coexistence of EP and pancreatic ascites is extremely rare and suggests severe pancreatic injury. This combination likely reflects extensive tissue necrosis with dual disruption, making management more complex. Although the patient declined further interventions, early recognition and prompt interventions remain critical to improving patient outcomes.

Figure: Figure 1. CT abdomen and pelvis with and without contrast showing near total replacement of the pancreas with an emphysematous gas collection with a fistulous tract from the tail into the descending colon.
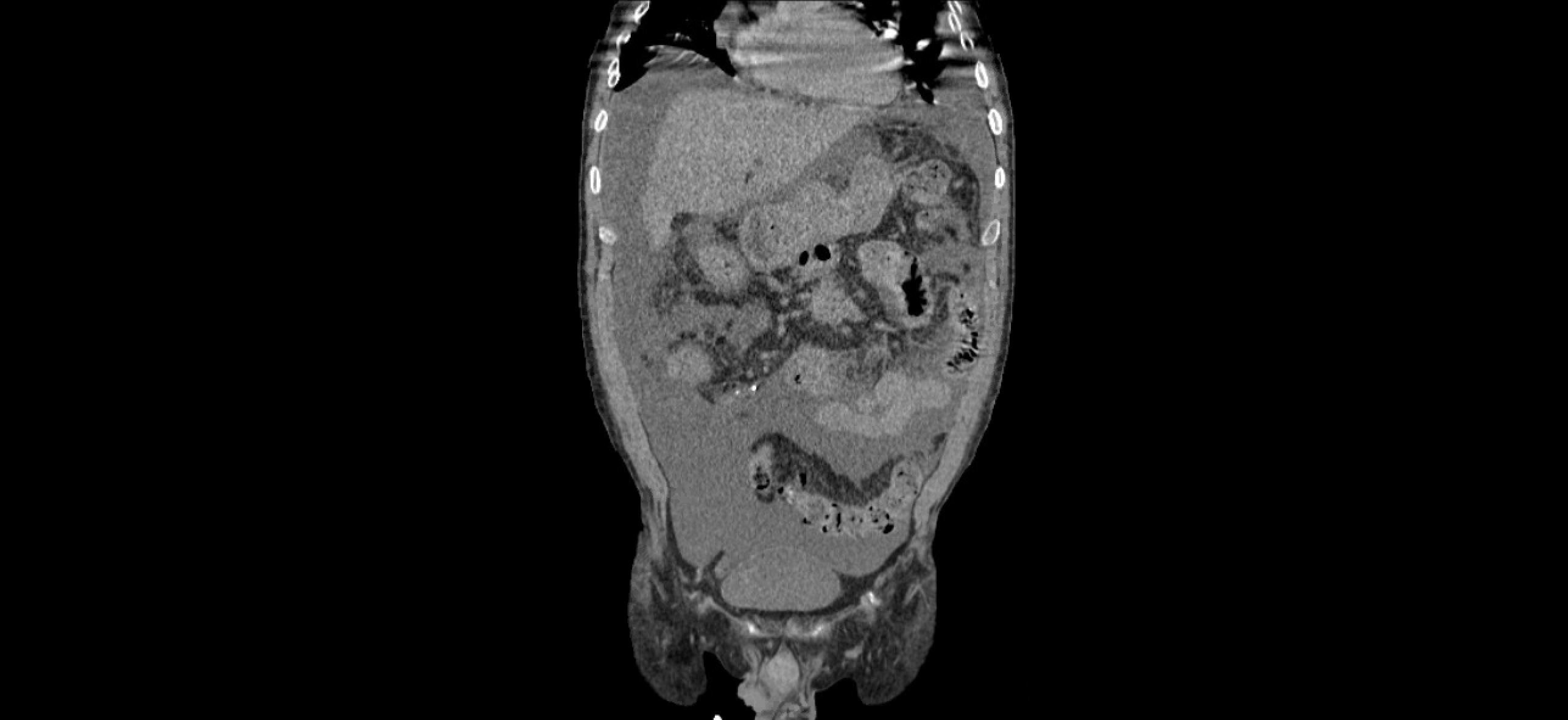
Figure: Figure 2. Contrast-enhanced computed tomography of the chest, abdomen, and pelvis showing complex pancreatic ascites (coronal view)
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Reshma John indicated no relevant financial relationships.
Kajol Patel indicated no relevant financial relationships.
Abel Setlhoka indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Kajol Patel, MD2, Abel Setlhoka, BS3, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2276 - Gas and Fluid: Emphysematous Pancreatitis With Pancreatic Ascites as a Sequela of Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Florida State University, Paterson, NJ; 3St. George's University, Paterson, NJ
Introduction: Emphysematous pancreatitis (EP) is a rare and fulminant variant of necrotizing pancreatitis characterized by gas-forming bacterial infection of pancreatic tissue. Pancreatic ascites, typically resulting from pancreatic duct disruption or pseudocyst rupture, is an uncommon complication of chronic or severe acute pancreatitis. The coexistence of EP and pancreatic ascites is exceedingly rare and portends a poor prognosis. Herein, we describe a rare case of EP with pancreatic ascites as a sequela of necrotizing pancreatitis.
Case Description/
Methods: A 68-year-old man presented to the ED for acute-onset pleuritic chest pain and dyspnea. The patient was admitted to our hospital a month prior for gallstone pancreatitis that progressed to necrotizing pancreatitis. He was treated with empiric antibiotics, IV fluids, nutrition, and analgesics. ERCP was aborted twice due to severe edema at the ampulla and later deferred due to persistent hypoxemia. Two weeks later, the patient underwent laparoscopic cholecystectomy and was found to have a walled-off pancreatic collection.
During this encounter, the patient was tachypneic and tachycardic, but afebrile. Contrast-enhanced CT of the abdomen and pelvis revealed a new pancreatico-colonic fistula, emphysematous pancreatitis, a walled-off necrosis measuring 10.5 cm x 3.2 cm, a large pleural effusion, and large complex ascites (Figure 1). The patient had a thoracentesis and Pigtail catheter was inserted in the ED for drainage and pleural fluid was exudative in nature. EUS demonstrated intrapancreatic air and calcific material, and diffuse echogenicity of the pancreatic parenchyma (Figure 2). Pancreatic duct could not be visualized due to intrapancreatic air. ERCP revealed pancreatic duct obstruction/stenosis in the genu of the pancreas, and wire, spyglass and contrast could not be extended beyond that point. One plastic stent was placed into the ventral pancreatic duct. Given his functional status and need for continued invasive procedures, the patient opted for hospice care.
Discussion: The coexistence of EP and pancreatic ascites is extremely rare and suggests severe pancreatic injury. This combination likely reflects extensive tissue necrosis with dual disruption, making management more complex. Although the patient declined further interventions, early recognition and prompt interventions remain critical to improving patient outcomes.

Figure: Figure 1. CT abdomen and pelvis with and without contrast showing near total replacement of the pancreas with an emphysematous gas collection with a fistulous tract from the tail into the descending colon.
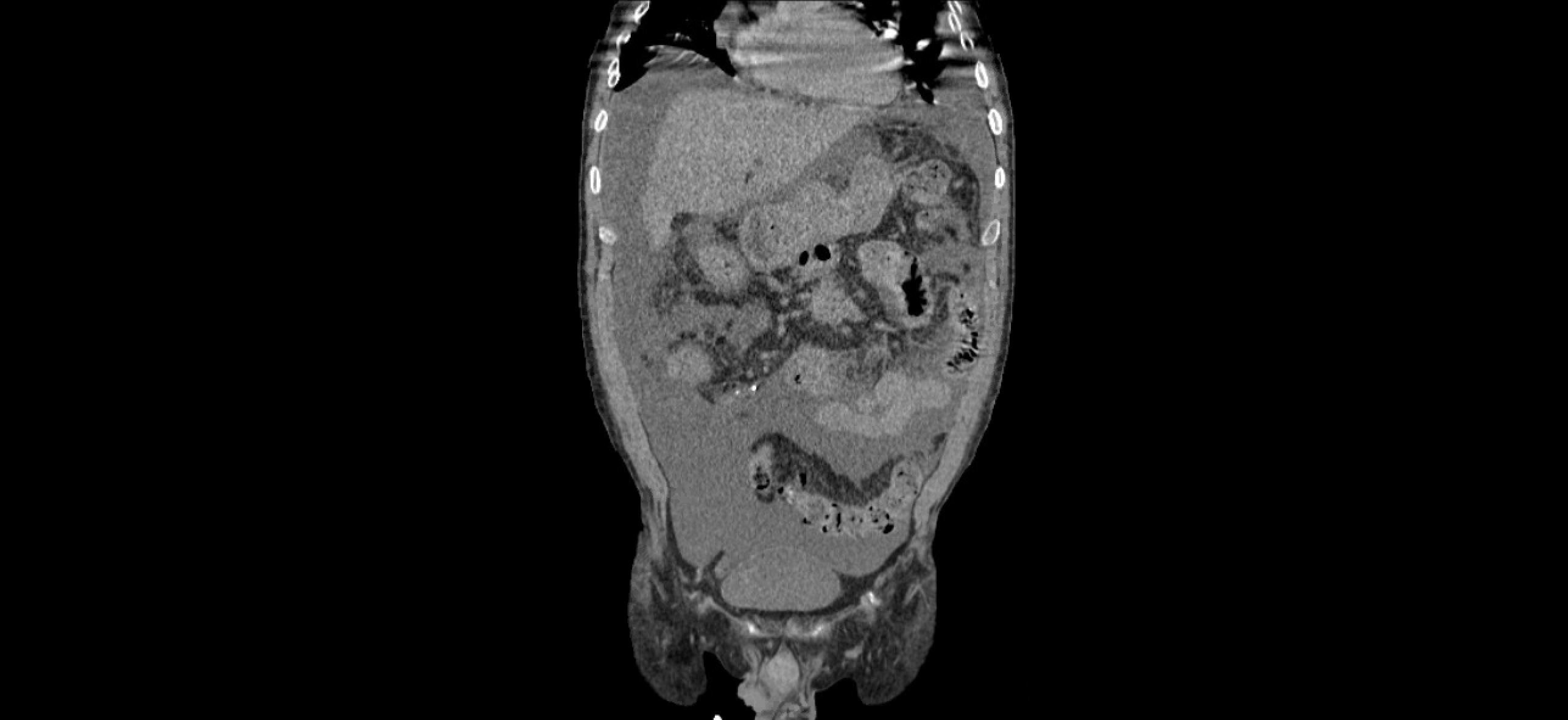
Figure: Figure 2. Contrast-enhanced computed tomography of the chest, abdomen, and pelvis showing complex pancreatic ascites (coronal view)
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Reshma John indicated no relevant financial relationships.
Kajol Patel indicated no relevant financial relationships.
Abel Setlhoka indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Reshma John, MD, MPH1, Kajol Patel, MD2, Abel Setlhoka, BS3, Praneeth Bandaru, MD1, Yana Cavanagh, MD1. P2276 - Gas and Fluid: Emphysematous Pancreatitis With Pancreatic Ascites as a Sequela of Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
