Monday Poster Session
Category: Biliary/Pancreas
P2245 - A Complicated Case of Recurrent Pancreatitis in a Patient With 2 CFTR Gene Mutations
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SZ
Sarah Zimmer, MD (she/her/hers)
Naval Medical Center Portsmouth
Chesapeake, VA
Presenting Author(s)
Sarah Zimmer, MD1, Allison Bush, MD2, Ryan Dinnen, MD, MBA3, Tyler Church, DO4
1Naval Medical Center Portsmouth, Chesapeake, VA; 2Uniformed Services University of the Health Sciences, Portsmouth, VA; 3Naval Medical Center Portsmouth, Portsmouth, VA; 4Naval Medical Center Portsmouth, Virginia Beach, VA
Introduction: Recurrent pancreatitis is a multifactorial condition influenced by both environmental and genetic factors. Mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene are a known contributor, with certain variants associated with recurrent pancreatitis. We present a case of a young, otherwise healthy male with recurrent necrotizing pancreatitis requiring extensive surgical intervention, who ultimately found to have cystic fibrosis (CF).
Case Description/
Methods: A 27-year-old male with no past medical history presented with epigastric pain radiating to his back, described as more intense but similar to five previous self-managed episodes. Imaging revealed necrotizing pancreatitis without gallstones or ductal dilation (Figure 1A). He was admitted for conservative management and discharged. However, over the following year, he experienced 11 hospital admissions for acute-on-chronic pancreatitis or its complications, including two intensive care unit stays. One episode involved multiple pancreatic fluid collections with walled-off necrosis (WON) extending into the colon (Figure 1B), requiring three exploratory laparotomies with debridement, necrosectomy, and partial colectomy with colostomy. Additional complications included an infected pancreatic fluid collection managed with retroperitoneal drain placement and WON managed by cystogastrostomy stent (Figures 1C and 1D). He was on no medications and laboratory testing was negative for alcohol use with normal triglycerides and IgG4. With no clear etiology identified, genetic testing was pursued, revealing two CFTR mutations (1585-1G >A and 5T_TG12), both associated with an increased risk of chronic pancreatitis. He additionally underwent sweat chloride testing, which confirmed CF, and he was started on CFTR modulator therapy.
Discussion: While an uncommon etiology of recurrent pancreatitis, growing evidence supports a significant role for genetic mutations in its pathogenesis. Individuals with two CFTR mutations have been shown to carry an approximately 40-fold increased risk of developing pancreatitis. As targeted therapies for these mutations become available, it is crucial for clinicians to consider genetic testing in appropriate clinical contexts. This case underscores the clinical relevance of CFTR mutations in pancreatic disease and highlights the expanding role of genetic evaluation in complex or idiopathic cases.
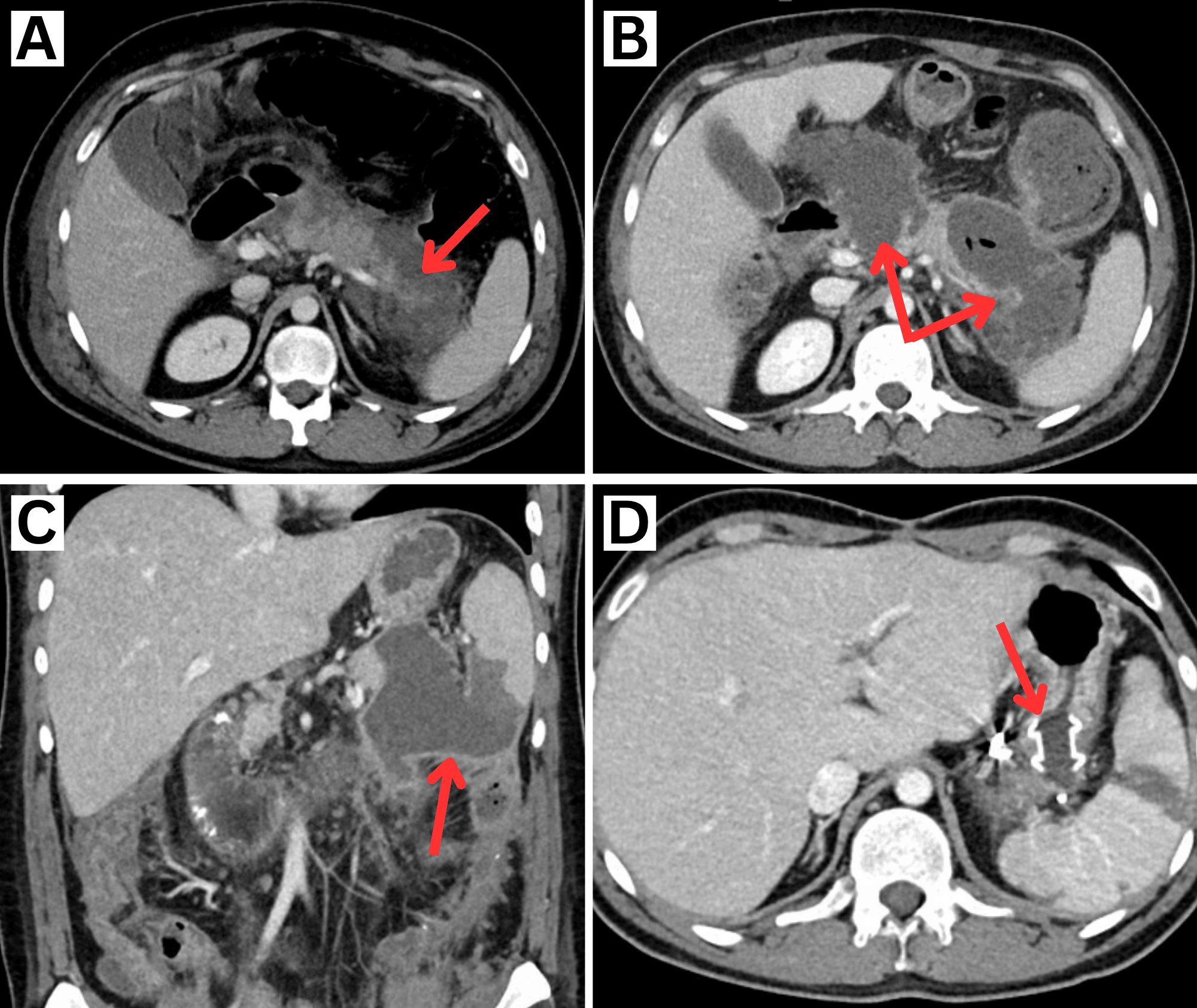
Figure: Figure 1. Image A: Axial contrast-enhanced CT A/P shows extensive pancreatic edema with non-enhancement of the head and tail consistent with necrotizing pancreatitis. Image B: One month later, axial contrast-enhanced CT A/P shows two well-defined areas of walled-off necrosis in the pancreatic head measuring 9.8 x 5.3cm and tail measuring 9.2 x 4.6cm with peripheral enhancement and free air concerning for infection or perforated viscus. Image C: Two months later, coronal contrast-enhanced CT A/P reveals progression of the pancreatic tail walled-off necrosis with possible extension into the spleen and developing enteric fistula. Image D: Axial contrast-enhanced CT after cystogastrostomy stent placement demonstrates a collapsed walled-off collection along the pancreatic tail.
Disclosures:
Sarah Zimmer indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Ryan Dinnen indicated no relevant financial relationships.
Tyler Church indicated no relevant financial relationships.
Sarah Zimmer, MD1, Allison Bush, MD2, Ryan Dinnen, MD, MBA3, Tyler Church, DO4. P2245 - A Complicated Case of Recurrent Pancreatitis in a Patient With 2 CFTR Gene Mutations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Naval Medical Center Portsmouth, Chesapeake, VA; 2Uniformed Services University of the Health Sciences, Portsmouth, VA; 3Naval Medical Center Portsmouth, Portsmouth, VA; 4Naval Medical Center Portsmouth, Virginia Beach, VA
Introduction: Recurrent pancreatitis is a multifactorial condition influenced by both environmental and genetic factors. Mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene are a known contributor, with certain variants associated with recurrent pancreatitis. We present a case of a young, otherwise healthy male with recurrent necrotizing pancreatitis requiring extensive surgical intervention, who ultimately found to have cystic fibrosis (CF).
Case Description/
Methods: A 27-year-old male with no past medical history presented with epigastric pain radiating to his back, described as more intense but similar to five previous self-managed episodes. Imaging revealed necrotizing pancreatitis without gallstones or ductal dilation (Figure 1A). He was admitted for conservative management and discharged. However, over the following year, he experienced 11 hospital admissions for acute-on-chronic pancreatitis or its complications, including two intensive care unit stays. One episode involved multiple pancreatic fluid collections with walled-off necrosis (WON) extending into the colon (Figure 1B), requiring three exploratory laparotomies with debridement, necrosectomy, and partial colectomy with colostomy. Additional complications included an infected pancreatic fluid collection managed with retroperitoneal drain placement and WON managed by cystogastrostomy stent (Figures 1C and 1D). He was on no medications and laboratory testing was negative for alcohol use with normal triglycerides and IgG4. With no clear etiology identified, genetic testing was pursued, revealing two CFTR mutations (1585-1G >A and 5T_TG12), both associated with an increased risk of chronic pancreatitis. He additionally underwent sweat chloride testing, which confirmed CF, and he was started on CFTR modulator therapy.
Discussion: While an uncommon etiology of recurrent pancreatitis, growing evidence supports a significant role for genetic mutations in its pathogenesis. Individuals with two CFTR mutations have been shown to carry an approximately 40-fold increased risk of developing pancreatitis. As targeted therapies for these mutations become available, it is crucial for clinicians to consider genetic testing in appropriate clinical contexts. This case underscores the clinical relevance of CFTR mutations in pancreatic disease and highlights the expanding role of genetic evaluation in complex or idiopathic cases.
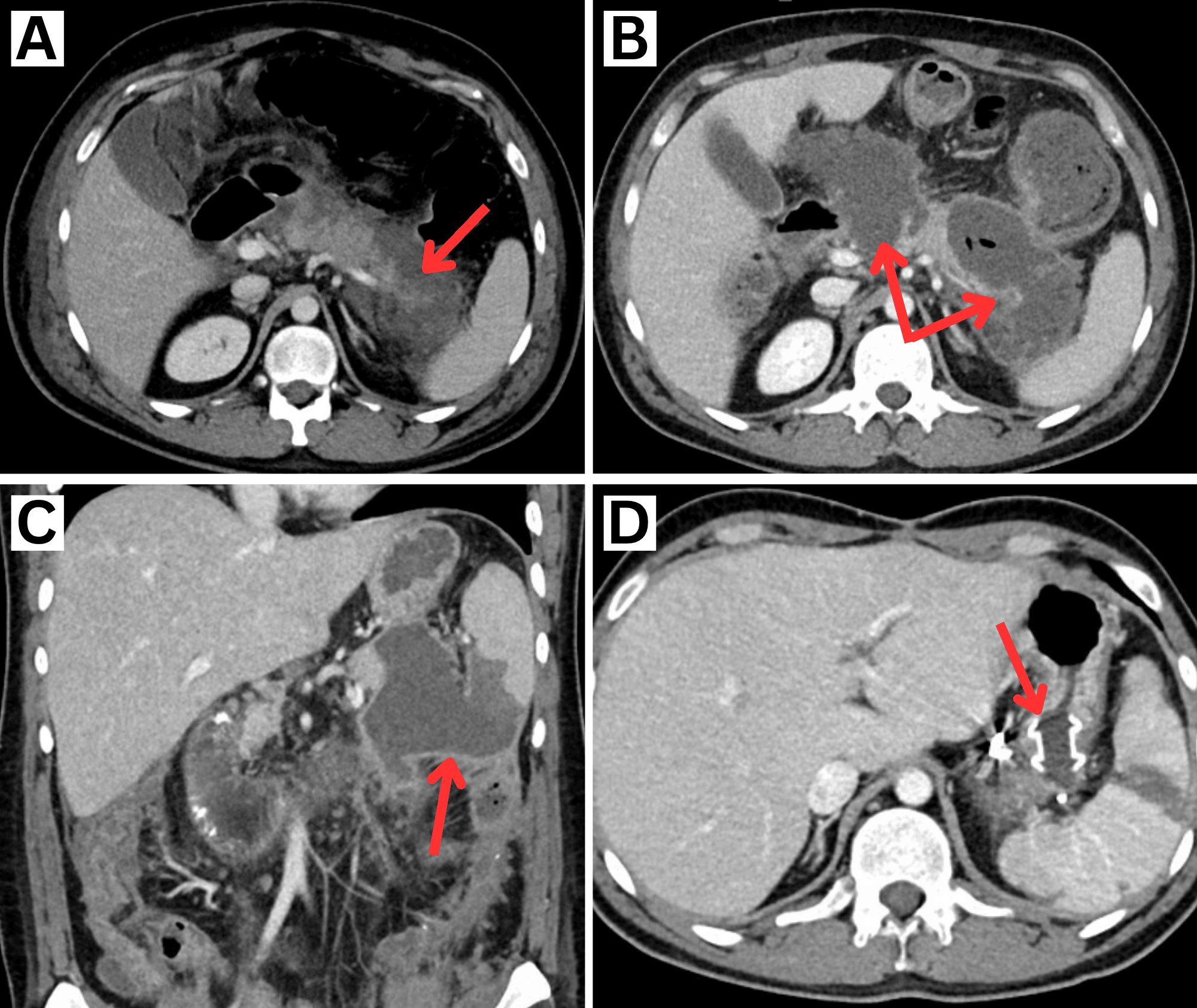
Figure: Figure 1. Image A: Axial contrast-enhanced CT A/P shows extensive pancreatic edema with non-enhancement of the head and tail consistent with necrotizing pancreatitis. Image B: One month later, axial contrast-enhanced CT A/P shows two well-defined areas of walled-off necrosis in the pancreatic head measuring 9.8 x 5.3cm and tail measuring 9.2 x 4.6cm with peripheral enhancement and free air concerning for infection or perforated viscus. Image C: Two months later, coronal contrast-enhanced CT A/P reveals progression of the pancreatic tail walled-off necrosis with possible extension into the spleen and developing enteric fistula. Image D: Axial contrast-enhanced CT after cystogastrostomy stent placement demonstrates a collapsed walled-off collection along the pancreatic tail.
Disclosures:
Sarah Zimmer indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Ryan Dinnen indicated no relevant financial relationships.
Tyler Church indicated no relevant financial relationships.
Sarah Zimmer, MD1, Allison Bush, MD2, Ryan Dinnen, MD, MBA3, Tyler Church, DO4. P2245 - A Complicated Case of Recurrent Pancreatitis in a Patient With 2 CFTR Gene Mutations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

