Monday Poster Session
Category: Biliary/Pancreas
P2237 - EUS-Guided Choledochoduodenostomy vs ERCP Transpapillary Metal Stenting for Distal Malignant Biliary Obstruction: Outcomes From a Single Center Experience
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

David Jonason, MD (he/him/his)
University of Utah
Salt Lake City, UT
Presenting Author(s)
David Jonason, MD1, Daniel Holten, MD1, Adam Bria, MD1, Emily Fellows, MD2, Christopher Ko, MD1, John Morris, MD1
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Endoscopic retrograde cholangiopancreatography with metal stenting (ERCP-M) is standard care to treat distal malignant biliary obstruction (dMBO). Endoscopic ultrasound-guided choledochoduodenostomy (EUS-CDS) with a lumen apposing metal stent has emerged as rescue therapy when ERCP-M fails and as a potential alternative first line therapy. Studies show comparable results, but involved endoscopists experienced in EUS biliary drainage (EUS-BD). We review outcomes of EUS-CDS for dMBO at our institution, with minimal prior EUS-BD experience.
Methods: Adult patients with dMBO treated by two endoscopists (4 EUS-CDS total, prior to study) with ERCP-M or EUS-CDS from 1/1/22 to 7/30/24 were included for retrospective analysis. Demographics, comorbidities, cancer type/extent, clinical success (bilirubin decrease > 30% by 1 week or > 50% by 30 days), 30-day complication/readmission rates, and biliary reintervention rates were compared between cohorts. One year stent patency (time from index procedure to first reintervention, death, or surgery) was assessed by Kaplan-Meier method with log rank. Predictors of stent dysfunction were evaluated by univariable and multivariable Cox regression.
Results: A total of 174 patients were included; 36 EUS-CDS, 138 ERCP-M. EUS-CDS technical success was 97%; 75% (27/36 cases) were performed as first line. Cases were restricted to a bile duct diameter ≥ 14 mm. Cohort characteristics were similar (Table 1) except for greater bile duct diameter and bilirubin in the EUS-CDS group. Both groups achieved high clinical success; 98% ERCP-M, 100% EUS-CDS. One-year stent patency did not significantly differ between cohorts (Fig. 1). There was no difference in time to discharge, 30-day complication/readmission rates, stent occlusion or need for repeat biliary intervention. The most common 30-day complication was cholangitis (n=3, 75%) after EUS-CDS and pancreatitis (n=10, 45%) after ERCP-M. On univariable analysis, BMI (for every 10 kg/m2 increase), metastatic disease and prior chemotherapy (HR 1.52, 2.2, 2.15, respectively) were associated with higher reintervention. BMI and metastatic disease remained significant on multivariable analysis (HR 1.74 and 2.18). There was no difference in reintervention between groups after adjusting for these covariables.
Discussion: Our experience suggests that EUS-CDS, with proper training, is adoptable for therapeutic endoscopists without prior EUS-BD expertise with outcomes comparable to ERCP-M for salvage and first line treatment of dMBO.
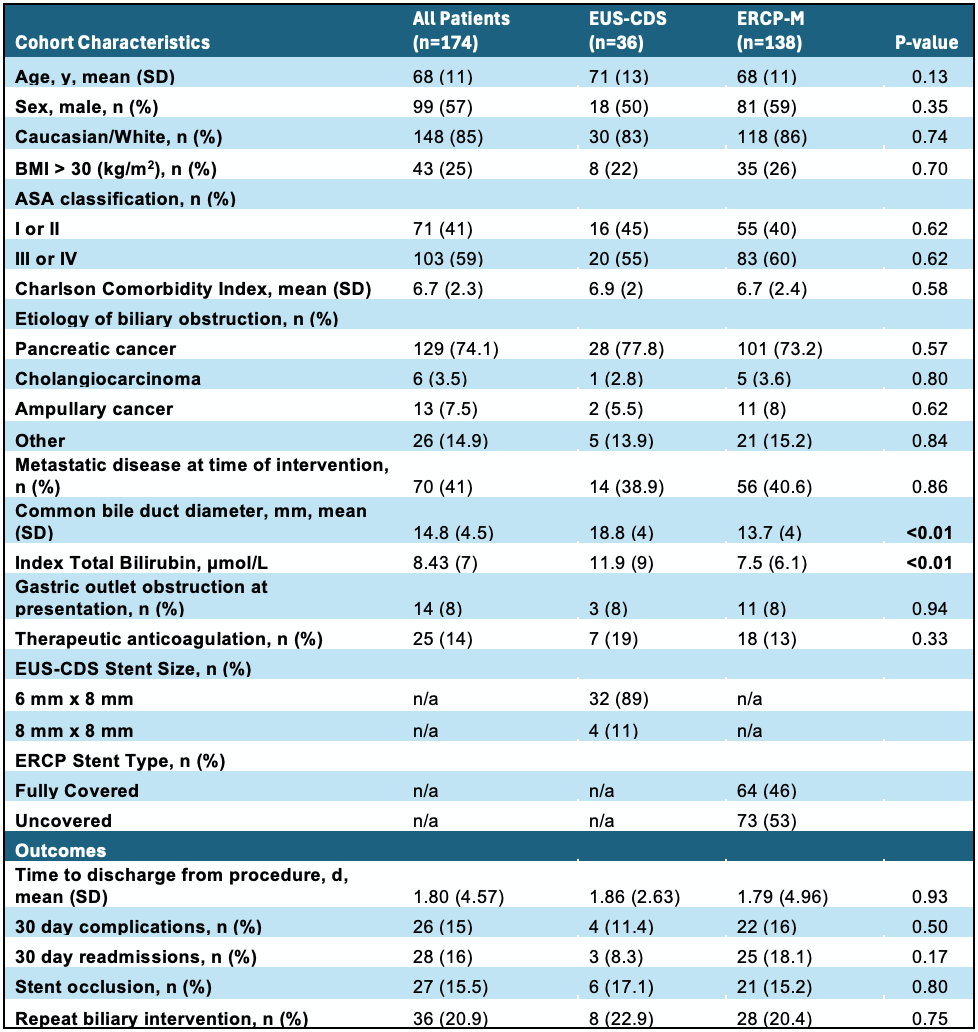
Figure: Table 1. Cohort Characteristics and Outcomes
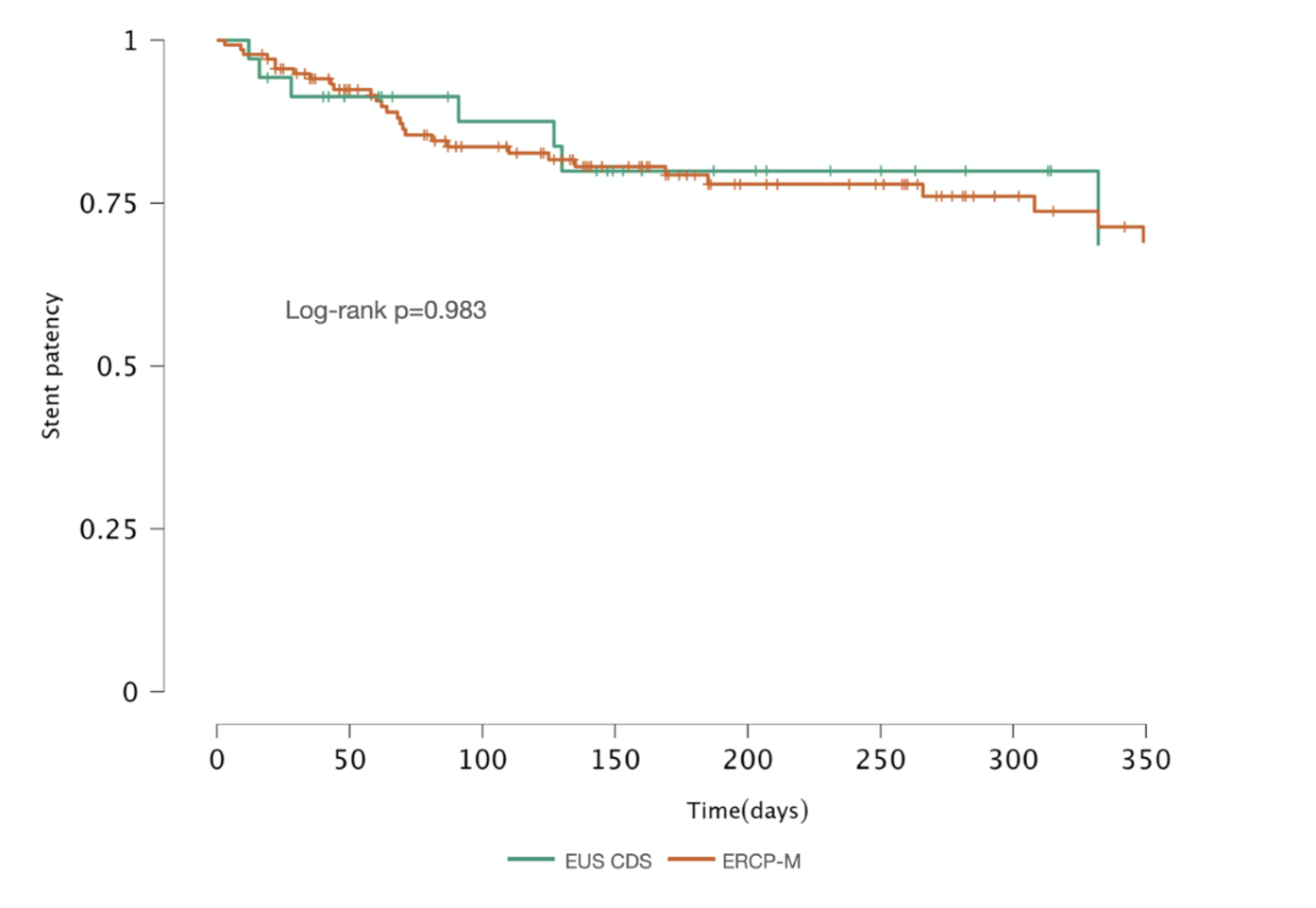
Figure: Figure 1. Kaplan Meier Stent Patency for ERCP-M and EUS-CDS
Disclosures:
David Jonason indicated no relevant financial relationships.
Daniel Holten indicated no relevant financial relationships.
Adam Bria indicated no relevant financial relationships.
Emily Fellows indicated no relevant financial relationships.
Christopher Ko indicated no relevant financial relationships.
John Morris indicated no relevant financial relationships.
David Jonason, MD1, Daniel Holten, MD1, Adam Bria, MD1, Emily Fellows, MD2, Christopher Ko, MD1, John Morris, MD1. P2237 - EUS-Guided Choledochoduodenostomy vs ERCP Transpapillary Metal Stenting for Distal Malignant Biliary Obstruction: Outcomes From a Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Endoscopic retrograde cholangiopancreatography with metal stenting (ERCP-M) is standard care to treat distal malignant biliary obstruction (dMBO). Endoscopic ultrasound-guided choledochoduodenostomy (EUS-CDS) with a lumen apposing metal stent has emerged as rescue therapy when ERCP-M fails and as a potential alternative first line therapy. Studies show comparable results, but involved endoscopists experienced in EUS biliary drainage (EUS-BD). We review outcomes of EUS-CDS for dMBO at our institution, with minimal prior EUS-BD experience.
Methods: Adult patients with dMBO treated by two endoscopists (4 EUS-CDS total, prior to study) with ERCP-M or EUS-CDS from 1/1/22 to 7/30/24 were included for retrospective analysis. Demographics, comorbidities, cancer type/extent, clinical success (bilirubin decrease > 30% by 1 week or > 50% by 30 days), 30-day complication/readmission rates, and biliary reintervention rates were compared between cohorts. One year stent patency (time from index procedure to first reintervention, death, or surgery) was assessed by Kaplan-Meier method with log rank. Predictors of stent dysfunction were evaluated by univariable and multivariable Cox regression.
Results: A total of 174 patients were included; 36 EUS-CDS, 138 ERCP-M. EUS-CDS technical success was 97%; 75% (27/36 cases) were performed as first line. Cases were restricted to a bile duct diameter ≥ 14 mm. Cohort characteristics were similar (Table 1) except for greater bile duct diameter and bilirubin in the EUS-CDS group. Both groups achieved high clinical success; 98% ERCP-M, 100% EUS-CDS. One-year stent patency did not significantly differ between cohorts (Fig. 1). There was no difference in time to discharge, 30-day complication/readmission rates, stent occlusion or need for repeat biliary intervention. The most common 30-day complication was cholangitis (n=3, 75%) after EUS-CDS and pancreatitis (n=10, 45%) after ERCP-M. On univariable analysis, BMI (for every 10 kg/m2 increase), metastatic disease and prior chemotherapy (HR 1.52, 2.2, 2.15, respectively) were associated with higher reintervention. BMI and metastatic disease remained significant on multivariable analysis (HR 1.74 and 2.18). There was no difference in reintervention between groups after adjusting for these covariables.
Discussion: Our experience suggests that EUS-CDS, with proper training, is adoptable for therapeutic endoscopists without prior EUS-BD expertise with outcomes comparable to ERCP-M for salvage and first line treatment of dMBO.
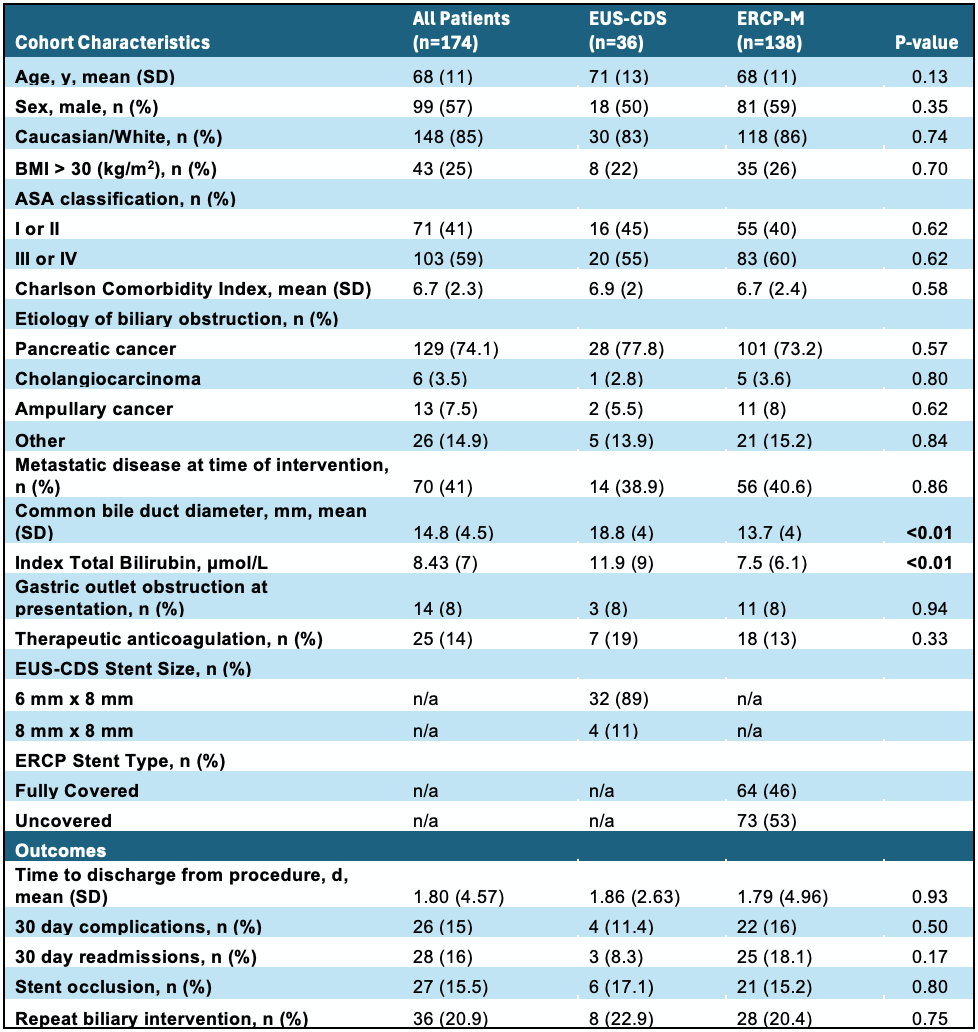
Figure: Table 1. Cohort Characteristics and Outcomes
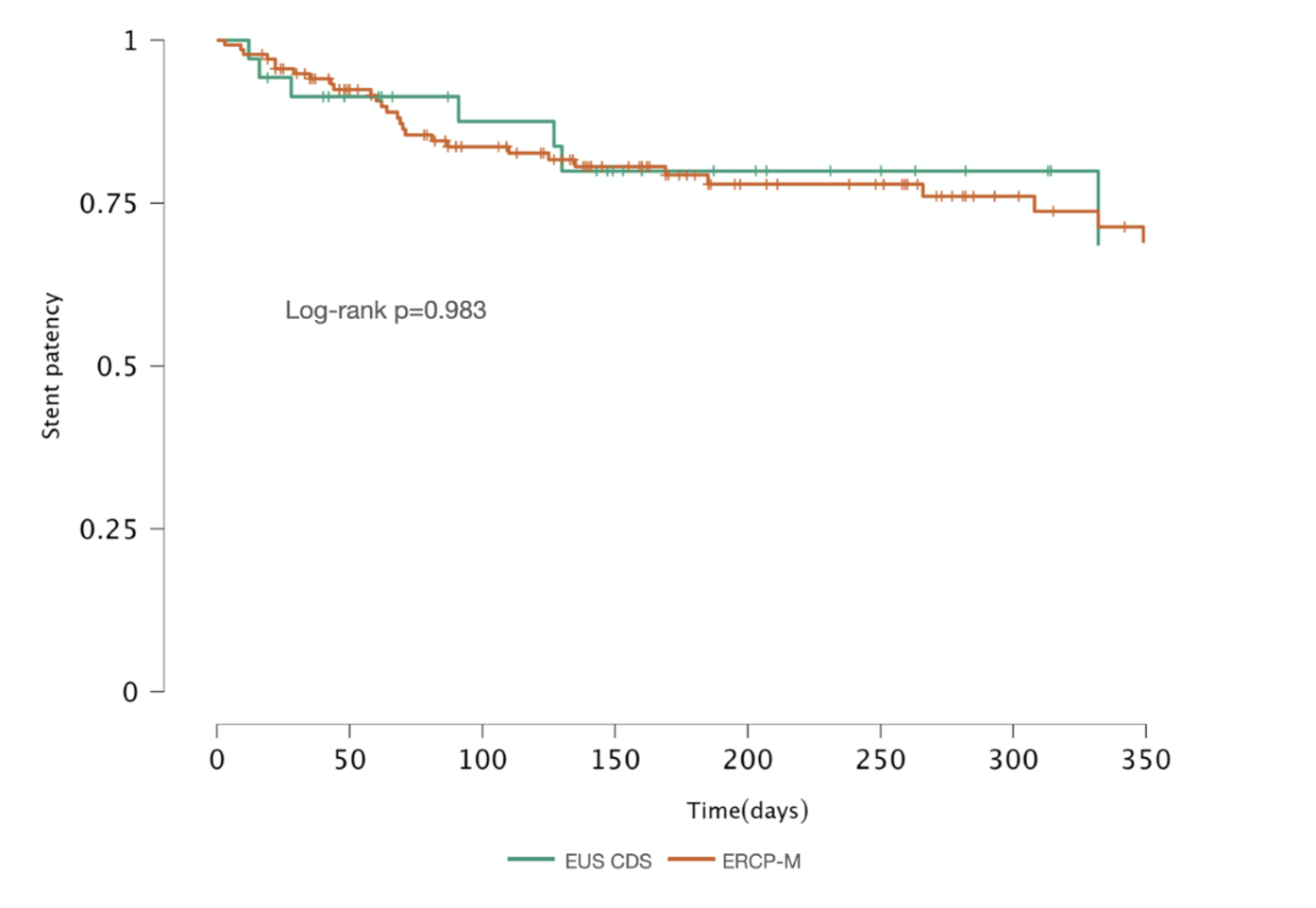
Figure: Figure 1. Kaplan Meier Stent Patency for ERCP-M and EUS-CDS
Disclosures:
David Jonason indicated no relevant financial relationships.
Daniel Holten indicated no relevant financial relationships.
Adam Bria indicated no relevant financial relationships.
Emily Fellows indicated no relevant financial relationships.
Christopher Ko indicated no relevant financial relationships.
John Morris indicated no relevant financial relationships.
David Jonason, MD1, Daniel Holten, MD1, Adam Bria, MD1, Emily Fellows, MD2, Christopher Ko, MD1, John Morris, MD1. P2237 - EUS-Guided Choledochoduodenostomy vs ERCP Transpapillary Metal Stenting for Distal Malignant Biliary Obstruction: Outcomes From a Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
