Sunday Poster Session
Category: Stomach and Spleen
P2131 - What Lies Beneath: A Case of Acute Buried Bumper Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Muhammad A. Khan, MD (he/him/his)
Montefiore Medical Center, Albert Einstein College of Medicine
Franklin Square, NY
Presenting Author(s)
Muhammad A. Khan, MD1, Sonia Mukhtar, MD1, Wareesha Zaidi, MD2
1Montefiore Medical Center, Albert Einstein College of Medicine, Franklin Square, NY; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a minimally invasive method for long-term enteral feeding. Though generally safe, PEG placement may lead to complications. Early complications, such as infection or bleeding, are common, while serious late complications, though rare, include gastrocutaneous fistulas and buried bumper syndrome (BBS). Although classically a late complication, BBS may present acutely in rare cases. We report a rare case of early-onset BBS, underscoring the need for early recognition and prompt intervention.
Case Description/
Methods: A 56-year-old woman with bipolar disorder and schizophrenia was admitted for altered mental status with catatonic features. Extensive neurological and infectious workup was unrevealing. She underwent multiple trials of lorazepam, IV steroids, IVIG, and electroconvulsive therapy with partial improvement. Due to persistent poor oral intake, a PEG tube was placed. She developed fever, abdominal pain, and leukocytosis. CT abdomen and pelvis revealed multiple abdominal wall fluid collections surrounding the PEG tract and the migration of the internal bumper into the abdominal wall, confirming diagnosis of Buried Bumper Syndrome (BBS) (Figure 1a). The PEG tube was removed (Figure 1b), and the abscesses were drained. She was treated with antibiotics. Due to poor oral intake, total parenteral nutrition (TPN) was initiated. Follow-up imaging revealed resolution of abdominal wall collections. Her mental status and oral intake improved; she was cleared for a minced diet and was discharged in stable condition.
Discussion: BBS is caused by migration of the internal bumper into the gastrostomy tract. It typically results from excessive tension, improper tube positioning, or inadvertent traction. Risk factors include poor tube design, chronic cough, low BMI, and immunocompromised status. BBS occurs in 0.3–2.4% of cases and often presents with leakage or tube dysfunction. Diagnosis is primarily clinical but can be supported by imaging; endoscopy is the gold standard. Orsi’s classification divides BBS into: Grade I (partial migration, mild/no symptoms), Grade II (dysfunction and leakage), and Grade III (complete obstruction). Treatment is grade-dependent—endoscopic for Grade I, surgical for Grades II/III. Early cases may preclude conservative management. In our case, BBS developed unusually early (day 8) and was managed endoscopically. Early recognition and daily tube monitoring are essential for prevention.
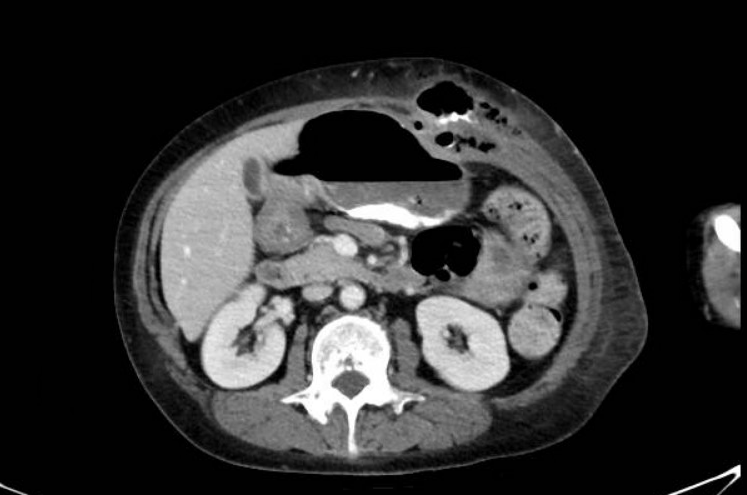
Figure: Figure 1a
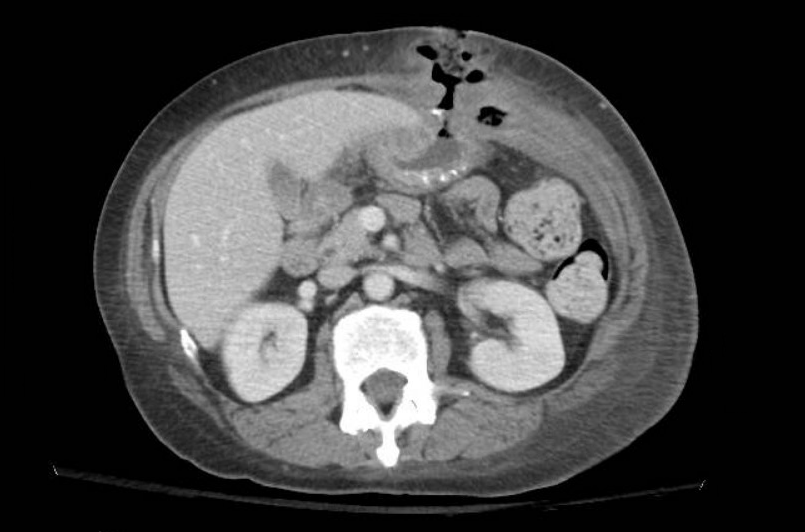
Figure: Figure 1b
Disclosures:
Muhammad Khan indicated no relevant financial relationships.
Sonia Mukhtar indicated no relevant financial relationships.
Wareesha Zaidi indicated no relevant financial relationships.
Muhammad A. Khan, MD1, Sonia Mukhtar, MD1, Wareesha Zaidi, MD2. P2131 - What Lies Beneath: A Case of Acute Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, Franklin Square, NY; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a minimally invasive method for long-term enteral feeding. Though generally safe, PEG placement may lead to complications. Early complications, such as infection or bleeding, are common, while serious late complications, though rare, include gastrocutaneous fistulas and buried bumper syndrome (BBS). Although classically a late complication, BBS may present acutely in rare cases. We report a rare case of early-onset BBS, underscoring the need for early recognition and prompt intervention.
Case Description/
Methods: A 56-year-old woman with bipolar disorder and schizophrenia was admitted for altered mental status with catatonic features. Extensive neurological and infectious workup was unrevealing. She underwent multiple trials of lorazepam, IV steroids, IVIG, and electroconvulsive therapy with partial improvement. Due to persistent poor oral intake, a PEG tube was placed. She developed fever, abdominal pain, and leukocytosis. CT abdomen and pelvis revealed multiple abdominal wall fluid collections surrounding the PEG tract and the migration of the internal bumper into the abdominal wall, confirming diagnosis of Buried Bumper Syndrome (BBS) (Figure 1a). The PEG tube was removed (Figure 1b), and the abscesses were drained. She was treated with antibiotics. Due to poor oral intake, total parenteral nutrition (TPN) was initiated. Follow-up imaging revealed resolution of abdominal wall collections. Her mental status and oral intake improved; she was cleared for a minced diet and was discharged in stable condition.
Discussion: BBS is caused by migration of the internal bumper into the gastrostomy tract. It typically results from excessive tension, improper tube positioning, or inadvertent traction. Risk factors include poor tube design, chronic cough, low BMI, and immunocompromised status. BBS occurs in 0.3–2.4% of cases and often presents with leakage or tube dysfunction. Diagnosis is primarily clinical but can be supported by imaging; endoscopy is the gold standard. Orsi’s classification divides BBS into: Grade I (partial migration, mild/no symptoms), Grade II (dysfunction and leakage), and Grade III (complete obstruction). Treatment is grade-dependent—endoscopic for Grade I, surgical for Grades II/III. Early cases may preclude conservative management. In our case, BBS developed unusually early (day 8) and was managed endoscopically. Early recognition and daily tube monitoring are essential for prevention.
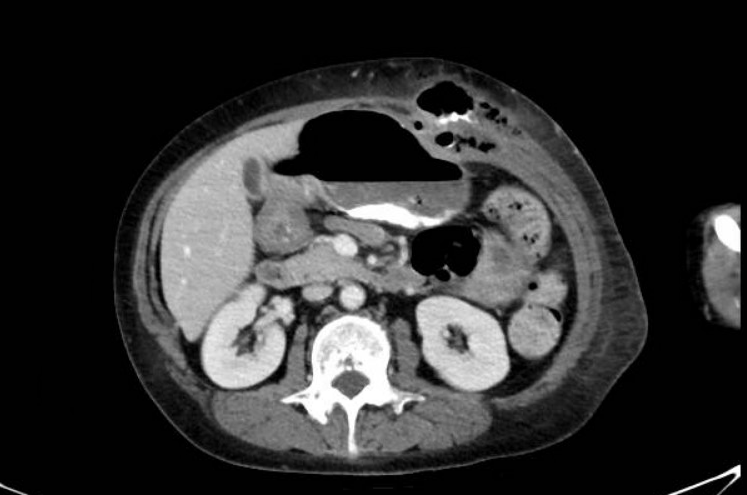
Figure: Figure 1a
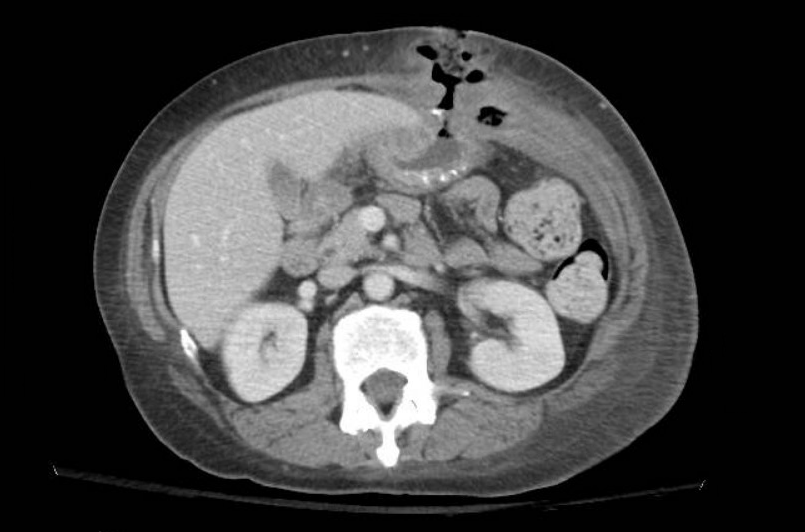
Figure: Figure 1b
Disclosures:
Muhammad Khan indicated no relevant financial relationships.
Sonia Mukhtar indicated no relevant financial relationships.
Wareesha Zaidi indicated no relevant financial relationships.
Muhammad A. Khan, MD1, Sonia Mukhtar, MD1, Wareesha Zaidi, MD2. P2131 - What Lies Beneath: A Case of Acute Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
