Sunday Poster Session
Category: Stomach and Spleen
P2130 - Gastric Metastases From Uveal Melanoma: A Rare Manifestation of an Aggressive Malignancy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Akira Folk, DO (she/her/hers)
Banner - University of Arizona Tucson
Tucson, AZ
Presenting Author(s)
Akira Folk, DO1, Ria Ghose Kundu, MD2, David Sedlock, MD2, Navroop Nagra, MD2
1Banner - University of Arizona Tucson, Tucson, AZ; 2HonorHealth, Scottsdale, AZ
Introduction: Uveal melanoma is the most common primary intraocular malignancy in adults, accounting for approximately 85% of ocular melanomas. Despite advances in local control of the primary tumor through enucleation, brachytherapy, or proton beam radiotherapy, nearly 50% of patients develop distant metastases, most commonly to the liver. Hepatic involvement often portends a poor prognosis, with median survival ranging from 6 to 12 months once metastasis is identified. Extrahepatic spread is significantly less common, and gastrointestinal (GI) tract involvement—particularly to the stomach—is exceedingly rare, with only a handful of cases reported in the literature.
Case Description/
Methods: We present the case of a 71-year-old male with a history of primary uveal melanoma, initially diagnosed and treated with plaque brachytherapy two years prior. Despite the initial favorable response of the primary tumor to treatment, subsequent surveillance imaging revealed a large, isolated hepatic metastasis. At the time of detection, the patient reported right upper quadrant abdominal pain with intractable nausea and vomiting. Esophagogastroduodenoscopy was performed and revealed multiple mucosal papules, ranging from 2 mm to 8 mm in size, within the gastric body (Figure 1). Biopsies of these lesions confirmed metastatic melanoma, with immunohistochemical staining positive for SOX-10 and Melan-A (Figure 2).
Discussion: This case highlights the aggressive nature of uveal melanoma and its potential for unpredictable metastatic spread. While hepatic metastases are well-known and expected, gastric involvement is rare and often overlooked due to nonspecific or absent GI symptoms. The mechanisms behind this unusual pattern remain unclear, though hematogenous dissemination—possibly via the portal circulation—is likely. Circulating tumor cells may lodge in gastric mucosal capillaries, leading to metastatic deposits in the stomach wall.
Recognizing such atypical metastases is important, especially in patients with known uveal melanoma presenting with unexplained GI symptoms. Endoscopic evaluation and histopathologic confirmation are critical for diagnosis and management. By presenting this rare occurrence, our case adds to the limited literature on gastric metastases from uveal melanoma and underscores the need to maintain a broad differential when evaluating GI lesions in patients with known malignancies. Further research is needed to clarify mechanisms of spread and guide surveillance strategies in this high-risk population.
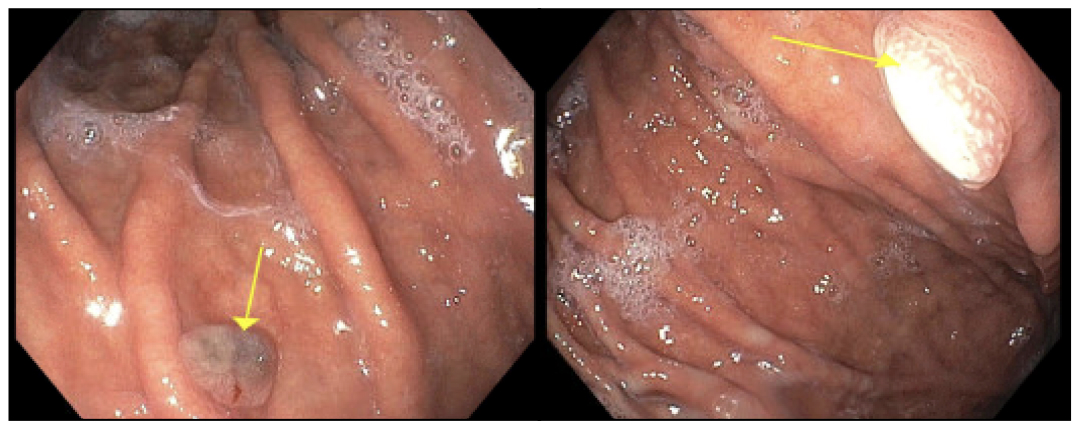
Figure: Figure 1. Endoscopic images showing multiple 2-8 mm papules without active bleeding or stigmata of recent bleeding in the gastric body.
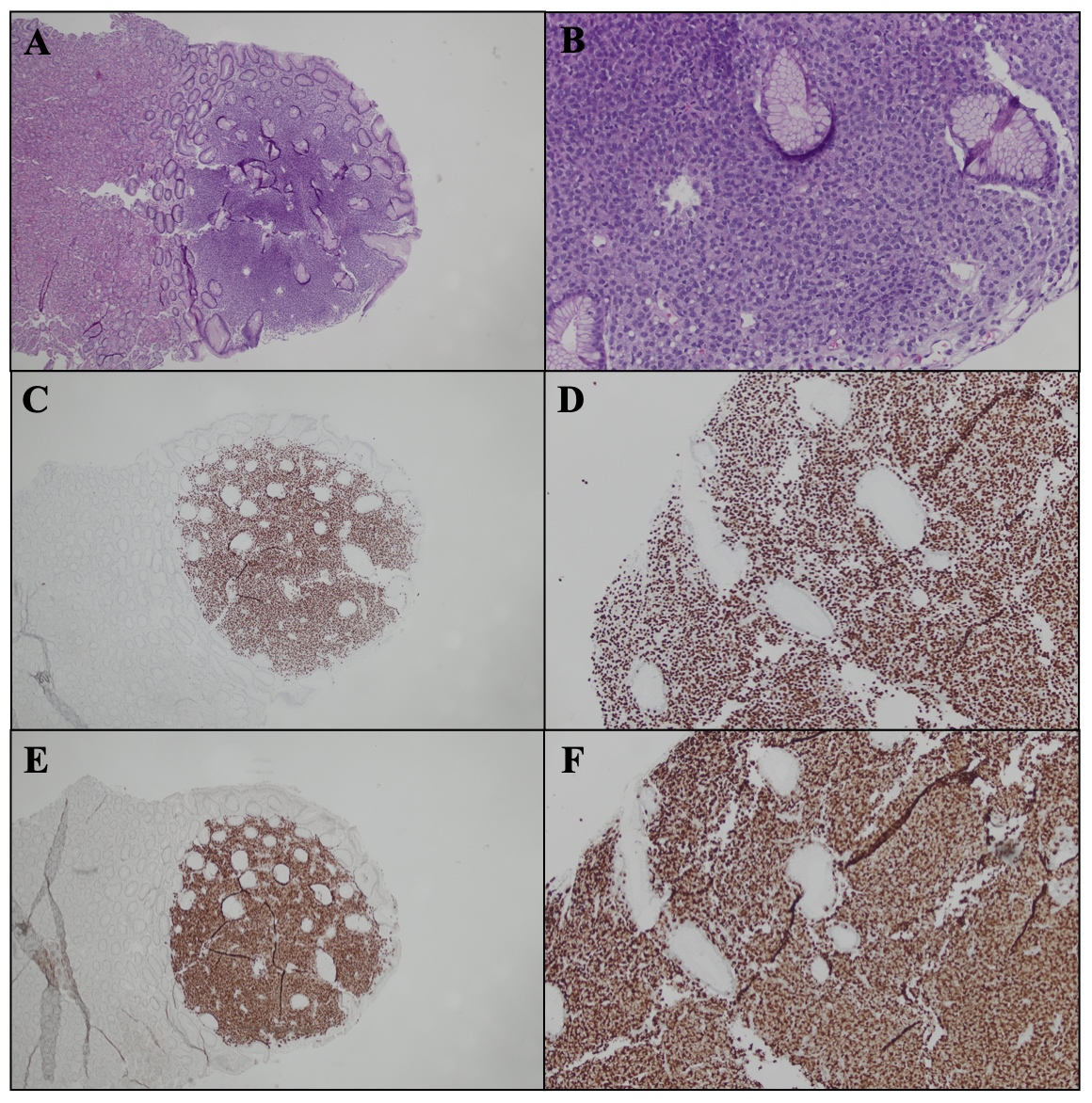
Figure: Figure 2. Representative images of gastric mucosa involved by metastatic malignant melanoma. (A, B) Hematoxylin and eosin-stained sections from low (A) to high (B) power demonstrating infiltration by malignant cells. (C–F) Immunohistochemical staining for SOX-10 (C, D) and Melan-A (E, F) highlighting the neoplastic melanocytic population.
Disclosures:
Akira Folk indicated no relevant financial relationships.
Ria Ghose Kundu indicated no relevant financial relationships.
David Sedlock indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Akira Folk, DO1, Ria Ghose Kundu, MD2, David Sedlock, MD2, Navroop Nagra, MD2. P2130 - Gastric Metastases From Uveal Melanoma: A Rare Manifestation of an Aggressive Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Banner - University of Arizona Tucson, Tucson, AZ; 2HonorHealth, Scottsdale, AZ
Introduction: Uveal melanoma is the most common primary intraocular malignancy in adults, accounting for approximately 85% of ocular melanomas. Despite advances in local control of the primary tumor through enucleation, brachytherapy, or proton beam radiotherapy, nearly 50% of patients develop distant metastases, most commonly to the liver. Hepatic involvement often portends a poor prognosis, with median survival ranging from 6 to 12 months once metastasis is identified. Extrahepatic spread is significantly less common, and gastrointestinal (GI) tract involvement—particularly to the stomach—is exceedingly rare, with only a handful of cases reported in the literature.
Case Description/
Methods: We present the case of a 71-year-old male with a history of primary uveal melanoma, initially diagnosed and treated with plaque brachytherapy two years prior. Despite the initial favorable response of the primary tumor to treatment, subsequent surveillance imaging revealed a large, isolated hepatic metastasis. At the time of detection, the patient reported right upper quadrant abdominal pain with intractable nausea and vomiting. Esophagogastroduodenoscopy was performed and revealed multiple mucosal papules, ranging from 2 mm to 8 mm in size, within the gastric body (Figure 1). Biopsies of these lesions confirmed metastatic melanoma, with immunohistochemical staining positive for SOX-10 and Melan-A (Figure 2).
Discussion: This case highlights the aggressive nature of uveal melanoma and its potential for unpredictable metastatic spread. While hepatic metastases are well-known and expected, gastric involvement is rare and often overlooked due to nonspecific or absent GI symptoms. The mechanisms behind this unusual pattern remain unclear, though hematogenous dissemination—possibly via the portal circulation—is likely. Circulating tumor cells may lodge in gastric mucosal capillaries, leading to metastatic deposits in the stomach wall.
Recognizing such atypical metastases is important, especially in patients with known uveal melanoma presenting with unexplained GI symptoms. Endoscopic evaluation and histopathologic confirmation are critical for diagnosis and management. By presenting this rare occurrence, our case adds to the limited literature on gastric metastases from uveal melanoma and underscores the need to maintain a broad differential when evaluating GI lesions in patients with known malignancies. Further research is needed to clarify mechanisms of spread and guide surveillance strategies in this high-risk population.
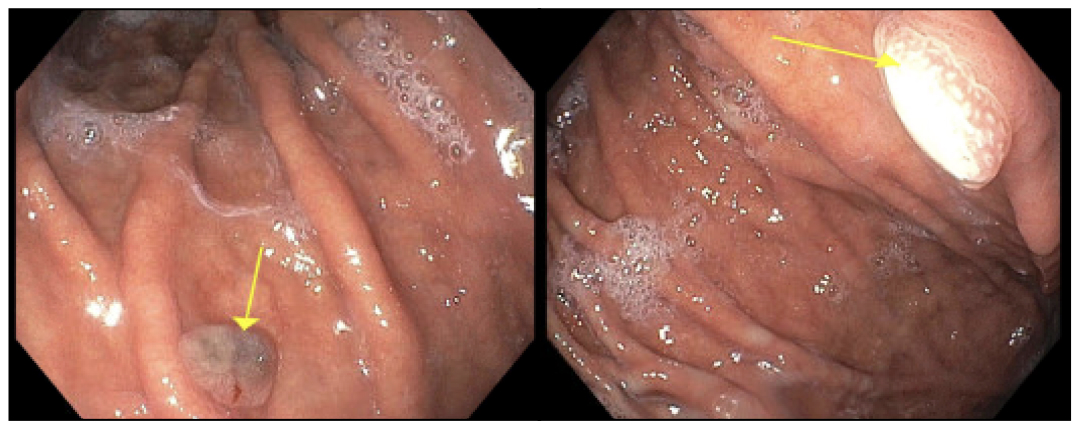
Figure: Figure 1. Endoscopic images showing multiple 2-8 mm papules without active bleeding or stigmata of recent bleeding in the gastric body.
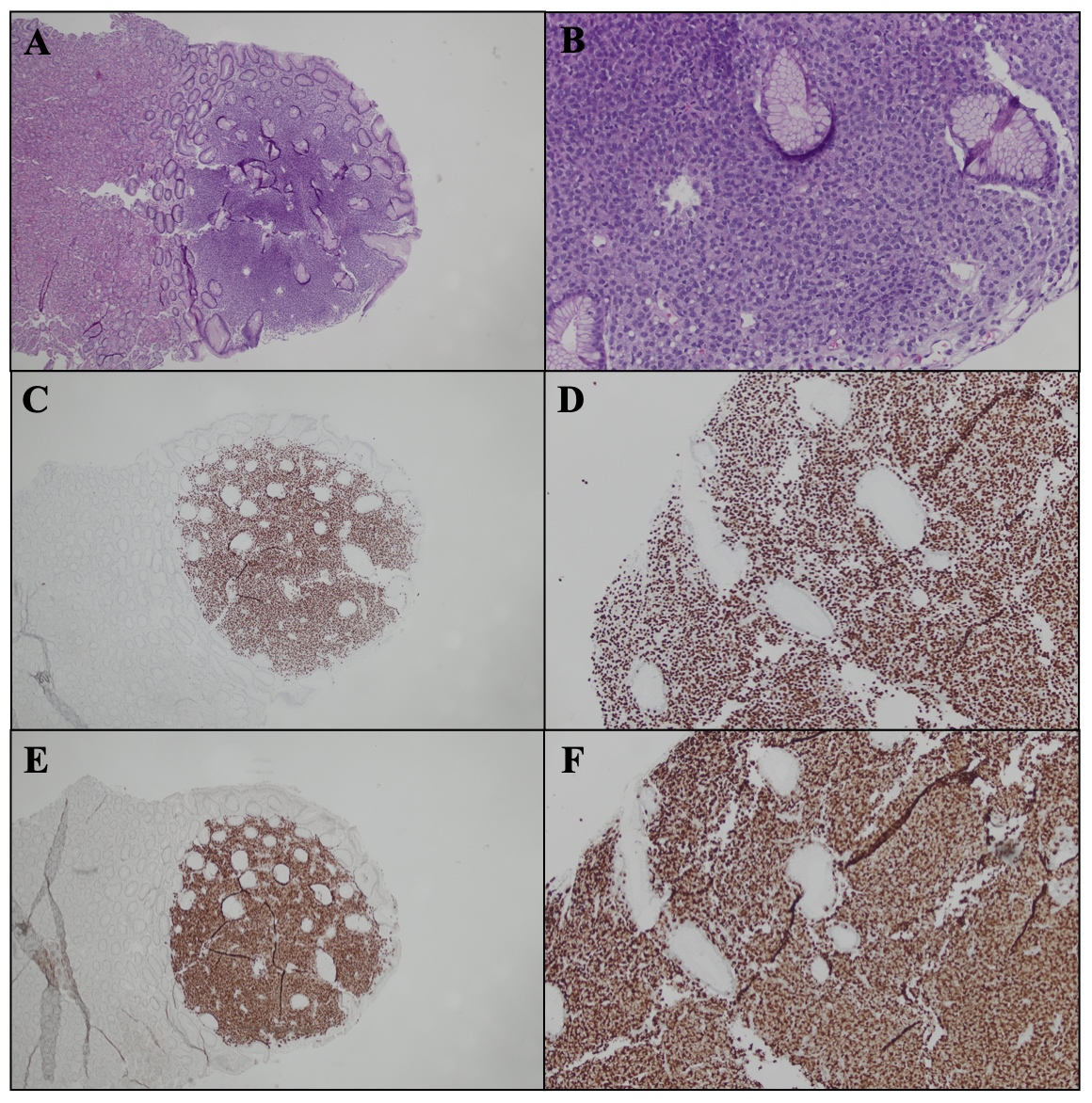
Figure: Figure 2. Representative images of gastric mucosa involved by metastatic malignant melanoma. (A, B) Hematoxylin and eosin-stained sections from low (A) to high (B) power demonstrating infiltration by malignant cells. (C–F) Immunohistochemical staining for SOX-10 (C, D) and Melan-A (E, F) highlighting the neoplastic melanocytic population.
Disclosures:
Akira Folk indicated no relevant financial relationships.
Ria Ghose Kundu indicated no relevant financial relationships.
David Sedlock indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Akira Folk, DO1, Ria Ghose Kundu, MD2, David Sedlock, MD2, Navroop Nagra, MD2. P2130 - Gastric Metastases From Uveal Melanoma: A Rare Manifestation of an Aggressive Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
