Sunday Poster Session
Category: Stomach and Spleen
P2123 - Cascade Stomach-Associated Dyspepsia Improved With Post-Prandial Forward Fold Stretching and PPI
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jesse A. Fletcher, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jesse A. Fletcher, MD, Justin Howard, MD
University of Minnesota, Minneapolis, MN
Introduction: Cascade, or “Cup-and-spill,” stomach is a unique anatomical variant in which the fundus of the stomach is folded over the body in a dorsal direction resulting in a pooling of ingested material in the fundus before eventually “cascading” into the body. Associated upper gastrointestinal symptoms often require surgical intervention and there is little mention of non-invasive anatomical correction for symptom relief in the literature. Herein, we describe a case of cascade stomach associated dyspepsia improved with post prandial forward fold stretching in combination with a proton pump inhibitor.
Case Description/
Methods: A 68-year-old female with a notable history of prior appendectomy, hysterectomy, and bilateral inguinal hernia repairs presented with a year and a half of intermittent dyspepsia and vomiting without any change in bowel pattern. Infectious and inflammatory laboratory testing, magnetic resonance elastography, and colonoscopy were largely unremarkable. Esophagogastroduodenoscopy revealed LA grade A reflux esophagitis and a J-shaped stomach with a submucosal band demarcation between the body and fundus (Figure 1). Subsequent X-ray upper gastrointestinal series confirmed the diagnosis of cascade stomach by showing contrast pooling within a posteriorly oriented proximal stomach that had minimal flow while standing supine unless the patient underwent torso flexion (Figure 2). There was no mucosal abnormality, filing defect, or stricture within the stomach and contrast easily flowed into the duodenum without abnormality. She was prescribed a proton pump inhibitor, advised to engage in forward fold stretching after meals, and avoid lying supine for several hours after meals. On follow-up approximately four months from her initial clinic visit, she reported an improvement in her symptoms.
Discussion: There is no current treatment guideline for cascade stomach associated dyspepsia and previously described conservative management with pharmacologic agents and dietary changes is often variable and inconsistent. As such, patients are often referred for surgical intervention for correction of cascade morphology. This case demonstrates that non-invasive anatomical correction via post prandial forward fold stretching in conjunction with other more common conservative measures may be successful in limiting the need for invasive intervention.
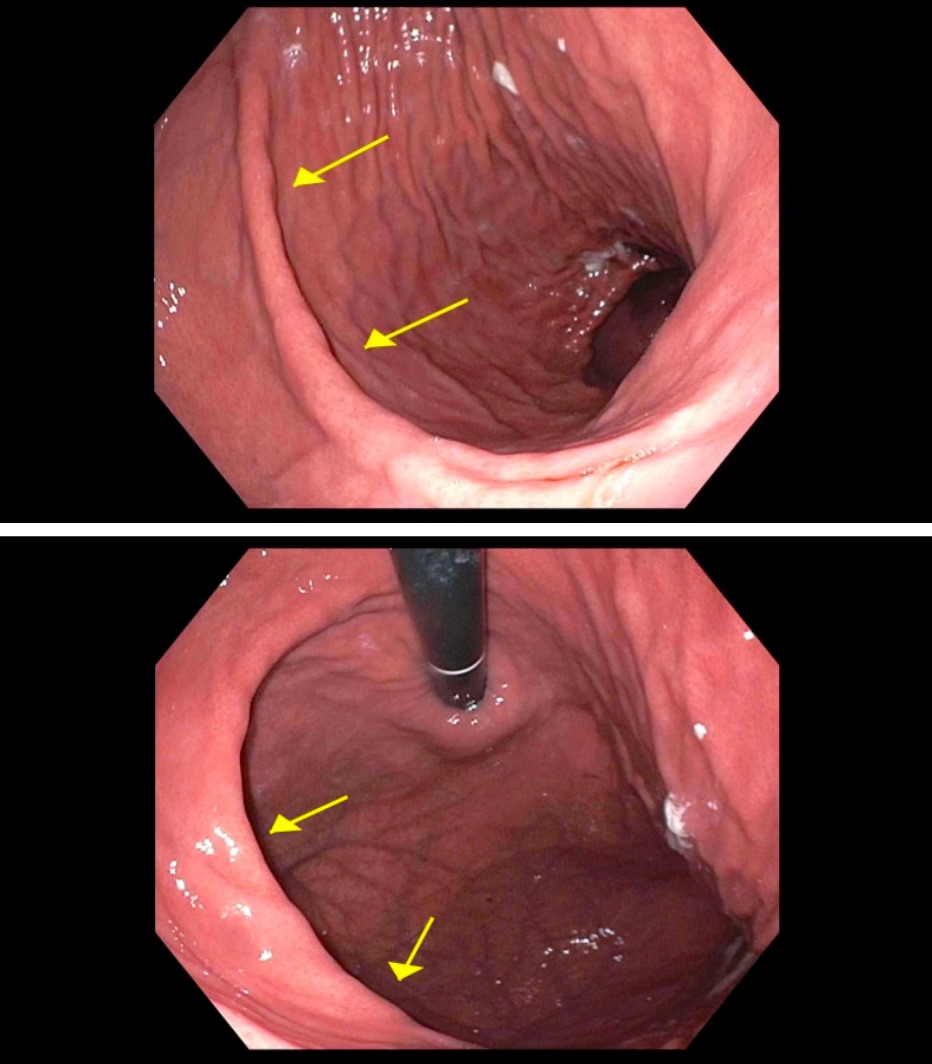
Figure: Figure 1. Images from esophagogastroduodenoscopy with arrows highlighting demarcation between gastric body and fundus.
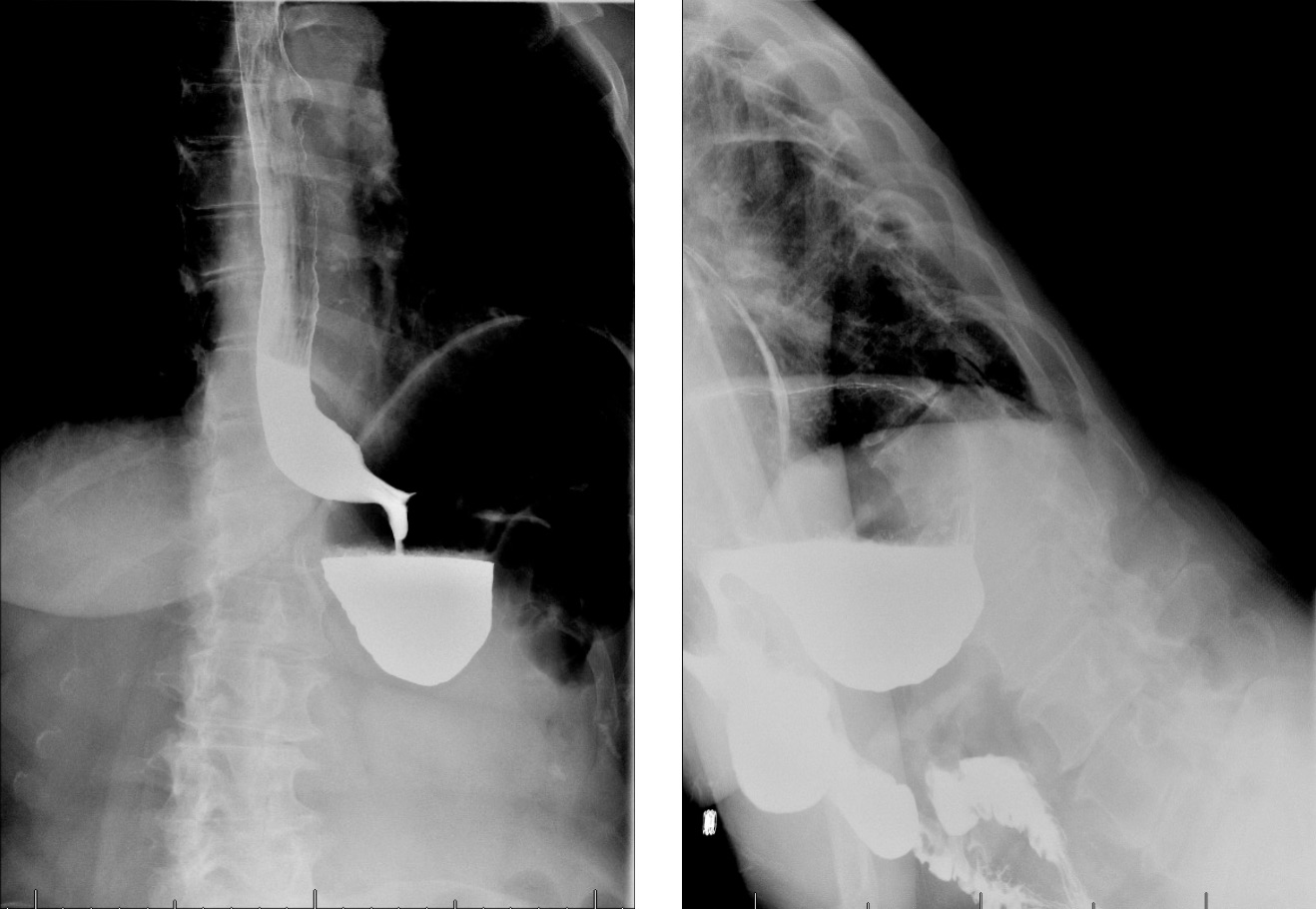
Figure: Figure 2. Images from XR upper gastrointestinal series showing contrast pooling in gastric fundus and subsequent forward flow of contrast from gastric fundus to body with torso flexion.
Disclosures:
Jesse Fletcher indicated no relevant financial relationships.
Justin Howard indicated no relevant financial relationships.
Jesse A. Fletcher, MD, Justin Howard, MD. P2123 - Cascade Stomach-Associated Dyspepsia Improved With Post-Prandial Forward Fold Stretching and PPI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Minnesota, Minneapolis, MN
Introduction: Cascade, or “Cup-and-spill,” stomach is a unique anatomical variant in which the fundus of the stomach is folded over the body in a dorsal direction resulting in a pooling of ingested material in the fundus before eventually “cascading” into the body. Associated upper gastrointestinal symptoms often require surgical intervention and there is little mention of non-invasive anatomical correction for symptom relief in the literature. Herein, we describe a case of cascade stomach associated dyspepsia improved with post prandial forward fold stretching in combination with a proton pump inhibitor.
Case Description/
Methods: A 68-year-old female with a notable history of prior appendectomy, hysterectomy, and bilateral inguinal hernia repairs presented with a year and a half of intermittent dyspepsia and vomiting without any change in bowel pattern. Infectious and inflammatory laboratory testing, magnetic resonance elastography, and colonoscopy were largely unremarkable. Esophagogastroduodenoscopy revealed LA grade A reflux esophagitis and a J-shaped stomach with a submucosal band demarcation between the body and fundus (Figure 1). Subsequent X-ray upper gastrointestinal series confirmed the diagnosis of cascade stomach by showing contrast pooling within a posteriorly oriented proximal stomach that had minimal flow while standing supine unless the patient underwent torso flexion (Figure 2). There was no mucosal abnormality, filing defect, or stricture within the stomach and contrast easily flowed into the duodenum without abnormality. She was prescribed a proton pump inhibitor, advised to engage in forward fold stretching after meals, and avoid lying supine for several hours after meals. On follow-up approximately four months from her initial clinic visit, she reported an improvement in her symptoms.
Discussion: There is no current treatment guideline for cascade stomach associated dyspepsia and previously described conservative management with pharmacologic agents and dietary changes is often variable and inconsistent. As such, patients are often referred for surgical intervention for correction of cascade morphology. This case demonstrates that non-invasive anatomical correction via post prandial forward fold stretching in conjunction with other more common conservative measures may be successful in limiting the need for invasive intervention.
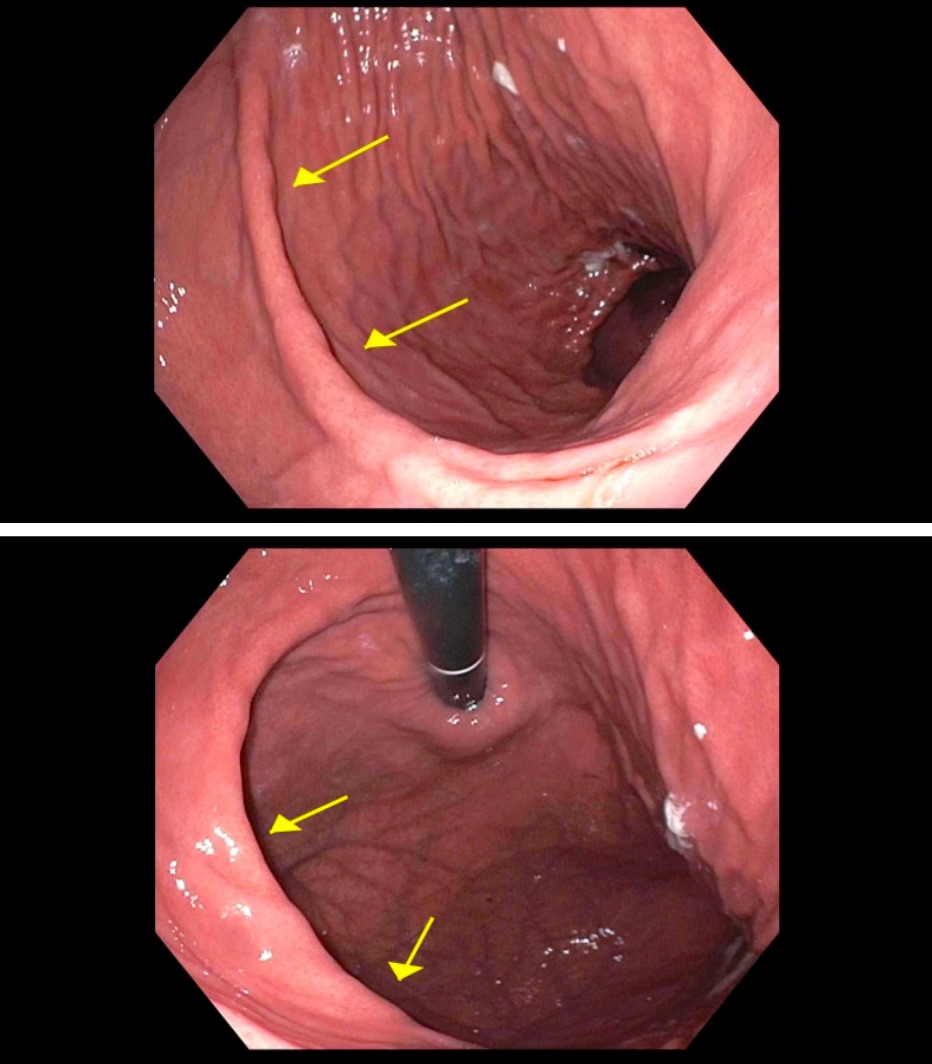
Figure: Figure 1. Images from esophagogastroduodenoscopy with arrows highlighting demarcation between gastric body and fundus.
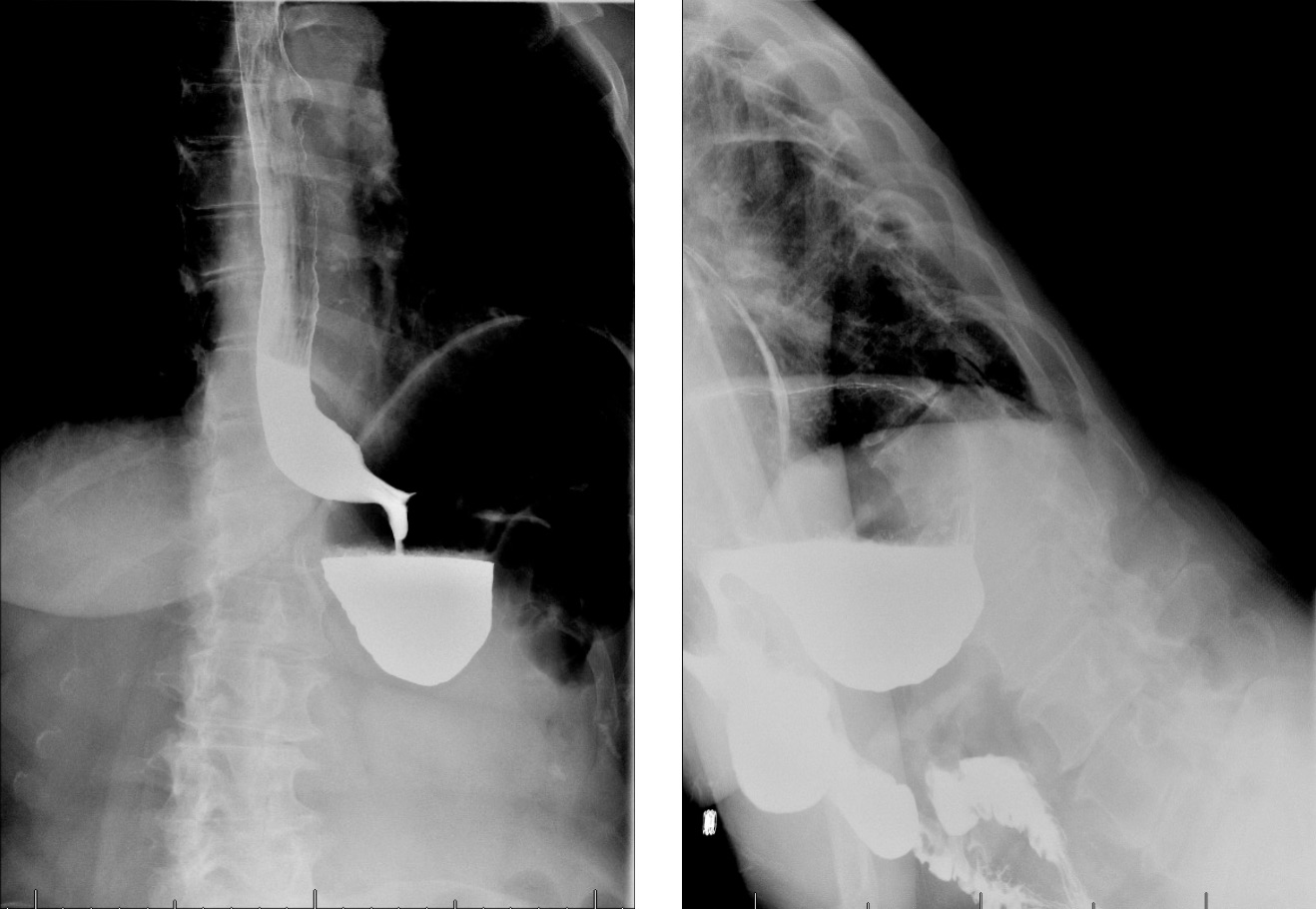
Figure: Figure 2. Images from XR upper gastrointestinal series showing contrast pooling in gastric fundus and subsequent forward flow of contrast from gastric fundus to body with torso flexion.
Disclosures:
Jesse Fletcher indicated no relevant financial relationships.
Justin Howard indicated no relevant financial relationships.
Jesse A. Fletcher, MD, Justin Howard, MD. P2123 - Cascade Stomach-Associated Dyspepsia Improved With Post-Prandial Forward Fold Stretching and PPI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

