Sunday Poster Session
Category: Stomach and Spleen
P2114 - A Rare Breakdown: Stent Fracture-Induced Small Bowel Obstruction in a Patient With Malignant Gastric Outlet Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Hany Habib, MD
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Hany Habib, MD1, Dheera Grover, MD2, Himsikhar Khataniar, MD2, Prateek Harne, MD3, Manish K. Dhawan, MD4
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Allegheny Health Network, Pittsburgh, PA
Introduction: Duodenal stenting is a widely used palliative treatment for malignant gastric outlet obstruction (mGOO). Stent fracture is a rare complication that may result in migration and distal small bowel obstruction, necessitating surgical intervention.
Case Description/
Methods: A 56-year-old woman with advanced-stage low-grade serous ovarian cancer complicated by mGOO underwent endoscopic placement of a fully covered esophageal stent (20 mm × 15 mm) traversing the pylorus into the duodenal bulb, secured with sutures. The stent was placed as a removable option to relieve obstruction while preserving gastric and duodenal anatomy for potential future surgical resection. Four months later, she presented with bilious vomiting, inability to tolerate oral intake, and obstipation. CT of the abdomen and pelvis with contrast revealed fracture of the previously placed stent, with the proximal fragment displaced into the gastric lumen and the distal fragment migrated distally, causing small bowel obstruction (Figure 1), necessitating exploratory laparotomy. A retrocolic gastrojejunostomy was created, and the proximal stent fragment was extracted via gastrotomy. The distal fragment was found embedded within a segment of small bowel involved with mesenteric tumor implants; this segment was resected en bloc, followed by a stapled side-to-side small bowel anastomosis. Her postoperative course was uneventful. The nasogastric tube was removed on postoperative day seven after a successful clamp trial, and she was discharged home tolerating a regular diet.
Discussion: Duodenal stent fracture is a rare but clinically significant complication in the palliative management of mGOO, with reported rates ranging from 0.9% to 2.3%. Risk factors include mechanical stress, tumor burden, and procedural instrumentation. While covered stents reduce the risk of tumor ingrowth, they are more prone to migration; uncovered stents, by contrast, offer greater anchorage but carry a higher risk of obstruction. This case highlights the importance of considering stent-related complications in patients presenting with recurrent obstructive symptoms after prior endoscopic stenting, particularly when unconventional stent types or anatomically complex regions are involved.
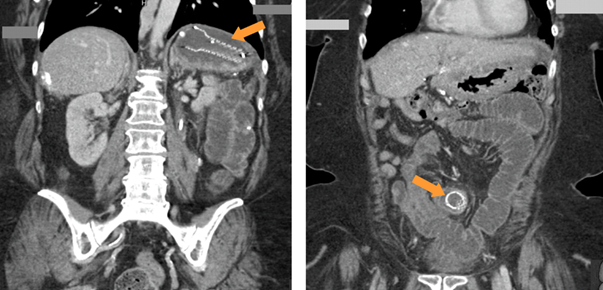
Figure: Figure 1: Coronal CT images of the abdomen. (Left) The proximal fractured stent fragment is seen within the gastric lumen (arrow), associated with gastric distension. (Right) The distal fragment is visualized within a dilated small bowel loop (arrow).
Disclosures:
Hany Habib indicated no relevant financial relationships.
Dheera Grover: NA – NA.
Himsikhar Khataniar indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Manish Dhawan indicated no relevant financial relationships.
Hany Habib, MD1, Dheera Grover, MD2, Himsikhar Khataniar, MD2, Prateek Harne, MD3, Manish K. Dhawan, MD4. P2114 - A Rare Breakdown: Stent Fracture-Induced Small Bowel Obstruction in a Patient With Malignant Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Allegheny Health Network, Pittsburgh, PA
Introduction: Duodenal stenting is a widely used palliative treatment for malignant gastric outlet obstruction (mGOO). Stent fracture is a rare complication that may result in migration and distal small bowel obstruction, necessitating surgical intervention.
Case Description/
Methods: A 56-year-old woman with advanced-stage low-grade serous ovarian cancer complicated by mGOO underwent endoscopic placement of a fully covered esophageal stent (20 mm × 15 mm) traversing the pylorus into the duodenal bulb, secured with sutures. The stent was placed as a removable option to relieve obstruction while preserving gastric and duodenal anatomy for potential future surgical resection. Four months later, she presented with bilious vomiting, inability to tolerate oral intake, and obstipation. CT of the abdomen and pelvis with contrast revealed fracture of the previously placed stent, with the proximal fragment displaced into the gastric lumen and the distal fragment migrated distally, causing small bowel obstruction (Figure 1), necessitating exploratory laparotomy. A retrocolic gastrojejunostomy was created, and the proximal stent fragment was extracted via gastrotomy. The distal fragment was found embedded within a segment of small bowel involved with mesenteric tumor implants; this segment was resected en bloc, followed by a stapled side-to-side small bowel anastomosis. Her postoperative course was uneventful. The nasogastric tube was removed on postoperative day seven after a successful clamp trial, and she was discharged home tolerating a regular diet.
Discussion: Duodenal stent fracture is a rare but clinically significant complication in the palliative management of mGOO, with reported rates ranging from 0.9% to 2.3%. Risk factors include mechanical stress, tumor burden, and procedural instrumentation. While covered stents reduce the risk of tumor ingrowth, they are more prone to migration; uncovered stents, by contrast, offer greater anchorage but carry a higher risk of obstruction. This case highlights the importance of considering stent-related complications in patients presenting with recurrent obstructive symptoms after prior endoscopic stenting, particularly when unconventional stent types or anatomically complex regions are involved.
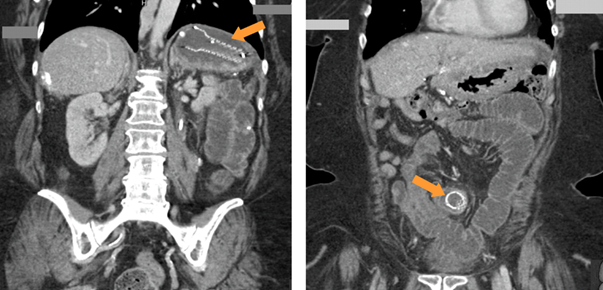
Figure: Figure 1: Coronal CT images of the abdomen. (Left) The proximal fractured stent fragment is seen within the gastric lumen (arrow), associated with gastric distension. (Right) The distal fragment is visualized within a dilated small bowel loop (arrow).
Disclosures:
Hany Habib indicated no relevant financial relationships.
Dheera Grover: NA – NA.
Himsikhar Khataniar indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Manish Dhawan indicated no relevant financial relationships.
Hany Habib, MD1, Dheera Grover, MD2, Himsikhar Khataniar, MD2, Prateek Harne, MD3, Manish K. Dhawan, MD4. P2114 - A Rare Breakdown: Stent Fracture-Induced Small Bowel Obstruction in a Patient With Malignant Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
