Sunday Poster Session
Category: Stomach and Spleen
P2110 - The Key to the Heart Is Through the Stomach: A Case of Gastrojejunal-Pericardial Fistula
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- WW
William H. Wheless, MD
Atrium Health Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
Areej Mazhar, DO, Andrew M. Dries, MD, Shailendra Chauhan, MD, Shreyans Doshi, MD, William H. Wheless, MD
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: We present a case of a rare complication of roux-en-Y reconstruction. While surgery has historically been the mainstay of management, we demonstrate success with minimally invasive esophagogastroduodenoscopy (EGD) with stent placement.
Case Description/
Methods: 66 year old female presented to the ER with symptoms of shortness of breath and chest pain. She has a history of hiatal hernia complicated by gastric necrosis requiring subtotal gastrectomy and Roux-en-Y reconstruction in May 2023. She was found to be in shock with pneumopericardium. CT imaging showed a herniated gastrojejunal (GJ) anastomosis above the diaphragm and concern for erosion into the pericardium. Esophagram confirmed communication between the GJ and pericardium; she also was noted to have a right sided pleural effusion.
She underwent pericardial drain and right chest tube placement with improvement. Pericardial cultures were positive for Candida glabrata and was managed with broad spectrum antimicrobials. EGD 1/20/25 showed an ulcerated anastomosis, two overlapping fully covered metal stents (23 mm x 15 cm and 23 mm X 12 cm) were placed. Esophagram showed no leak. CT chest on 1/28/25 was ordered to assess her pleural effusion for chest tube removal and showed migration of the stents to the jejunum. Repeat esophagram showed no contrast extravasation. Stents were removed by EGD 1/31/2025 and replaced with a single fully covered metal stent measuring 23 mm x 15 cm. Attempts to secure with clip x 2 were not successful. GJ ulcer was noted to be sealed by stent. Diet was advanced and pericardial drain was removed on 2/1/25. She was discharged to SNF on 2/11/25.
Discussion: This is an exceedingly rare complication that has been reported in the literature primarily in isolated case reports and case series after esophagectomy and less commonly Roux-en-Y gastric bypass. A case series published in 2021 included three cases of gastro-pericardial fistula that were all treated surgically. Length of hospital stays ranged form 26 days to 2 months. The length of stay from our case was 22 days after initial EGD. Complications same hospitalization included stent migration requiring EGD and replacement. In this case we demonstrate successful management of GJ enteric fistula with esophageal stent placement. Implications include a minimally invasive option with fewer complications, shorter hospital stays, and improved morbidity and mortality. Further clinical data are needed to confirm our findings.
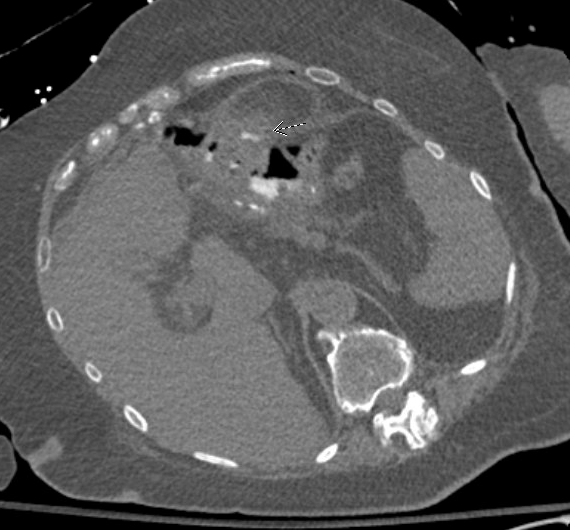
Figure: Figure 1. Gastric-pericardial fistula with very small amount of contrast accumulation in the pericardium following administration of positive enteric contrast, fistula favored to be localized to the pericardial base near the GJ anastomosis
Disclosures:
Areej Mazhar indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Shailendra Chauhan indicated no relevant financial relationships.
Shreyans Doshi indicated no relevant financial relationships.
William Wheless indicated no relevant financial relationships.
Areej Mazhar, DO, Andrew M. Dries, MD, Shailendra Chauhan, MD, Shreyans Doshi, MD, William H. Wheless, MD. P2110 - The Key to the Heart Is Through the Stomach: A Case of Gastrojejunal-Pericardial Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: We present a case of a rare complication of roux-en-Y reconstruction. While surgery has historically been the mainstay of management, we demonstrate success with minimally invasive esophagogastroduodenoscopy (EGD) with stent placement.
Case Description/
Methods: 66 year old female presented to the ER with symptoms of shortness of breath and chest pain. She has a history of hiatal hernia complicated by gastric necrosis requiring subtotal gastrectomy and Roux-en-Y reconstruction in May 2023. She was found to be in shock with pneumopericardium. CT imaging showed a herniated gastrojejunal (GJ) anastomosis above the diaphragm and concern for erosion into the pericardium. Esophagram confirmed communication between the GJ and pericardium; she also was noted to have a right sided pleural effusion.
She underwent pericardial drain and right chest tube placement with improvement. Pericardial cultures were positive for Candida glabrata and was managed with broad spectrum antimicrobials. EGD 1/20/25 showed an ulcerated anastomosis, two overlapping fully covered metal stents (23 mm x 15 cm and 23 mm X 12 cm) were placed. Esophagram showed no leak. CT chest on 1/28/25 was ordered to assess her pleural effusion for chest tube removal and showed migration of the stents to the jejunum. Repeat esophagram showed no contrast extravasation. Stents were removed by EGD 1/31/2025 and replaced with a single fully covered metal stent measuring 23 mm x 15 cm. Attempts to secure with clip x 2 were not successful. GJ ulcer was noted to be sealed by stent. Diet was advanced and pericardial drain was removed on 2/1/25. She was discharged to SNF on 2/11/25.
Discussion: This is an exceedingly rare complication that has been reported in the literature primarily in isolated case reports and case series after esophagectomy and less commonly Roux-en-Y gastric bypass. A case series published in 2021 included three cases of gastro-pericardial fistula that were all treated surgically. Length of hospital stays ranged form 26 days to 2 months. The length of stay from our case was 22 days after initial EGD. Complications same hospitalization included stent migration requiring EGD and replacement. In this case we demonstrate successful management of GJ enteric fistula with esophageal stent placement. Implications include a minimally invasive option with fewer complications, shorter hospital stays, and improved morbidity and mortality. Further clinical data are needed to confirm our findings.
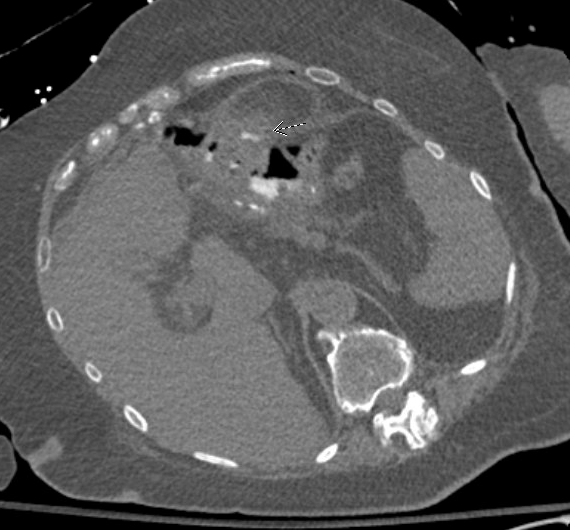
Figure: Figure 1. Gastric-pericardial fistula with very small amount of contrast accumulation in the pericardium following administration of positive enteric contrast, fistula favored to be localized to the pericardial base near the GJ anastomosis
Disclosures:
Areej Mazhar indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Shailendra Chauhan indicated no relevant financial relationships.
Shreyans Doshi indicated no relevant financial relationships.
William Wheless indicated no relevant financial relationships.
Areej Mazhar, DO, Andrew M. Dries, MD, Shailendra Chauhan, MD, Shreyans Doshi, MD, William H. Wheless, MD. P2110 - The Key to the Heart Is Through the Stomach: A Case of Gastrojejunal-Pericardial Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
