Sunday Poster Session
Category: Stomach and Spleen
P2109 - Masquerading as Boerhaave: A Gastric Perforation at the GE Junction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishika Trivedi, MD
DHR Health
McAllen, TX
Presenting Author(s)
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Asif Zamir, MD, FACG3
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, Edinburg, TX
Introduction: Pneumomediastinum is often attributed to esophageal perforation, particularly in the setting of Boerhaave syndrome. However, gastric perforations near surgically altered anatomies, such as Nissen fundoplication, can mimic this presentation. We present a rare case of contained gastric perforation at the gastroesophageal (GE) junction. Initially radiographically occult and ultimately diagnosed through delayed imaging and managed with endoscopic clipping.
Case Description/
Methods: A 31-year-old male with a history of mood disorder and prior Nissen fundoplication presented with acute retrosternal chest pain and dyspnea following a forceful coughing episode during a flu-like illness. He was tachycardic (heart rate 123), tachypneic (respiratory rate 30), and required 4L/min oxygen. Initial non-contrast CT chest demonstrated pneumomediastinum, perigastric stranding, and hiatal hernia with no clear perforation. Barium swallow with oral contrast again showed no extravasation. Due to further clinical deterioration, a subsequent non-contrast CT chest performed after the oral contrast had time to transit. It revealed extraluminal contrast pooling at the GE junction. This confirmed the gastric leak. Emergency upper endoscopy revealed a 1.5 cm deep linear ulcer on the posteroinferior fundus, due to the GE junction. It had fibrotic edges and mucosal edema suggestive of a chronic process. Sever through the scope clips (six Mantis and one resolution) were deployed, achieving complete closure. There was no residual leak on the confirmatory contrast study (Figure 1). The patient's respiratory status improved, and he was successfully managed with a full recovery.
Discussion: This case illustrates that gastric perforation near the GE junction, particularly in patients with prior Nissen fundoplication, can closely mimic Boerhaave syndrome. This case highlights that not all pneumomediastinum originates from the esophagus. Delayed imaging in the supine position can reveal subtle gastrointestinal leaks. Early endoscopic evaluation is critical when clinical suspicion persists despite the non-diagnostic imaging, promoting recognition. This may obviate the need for surgery in selected cases of gastric perforation.
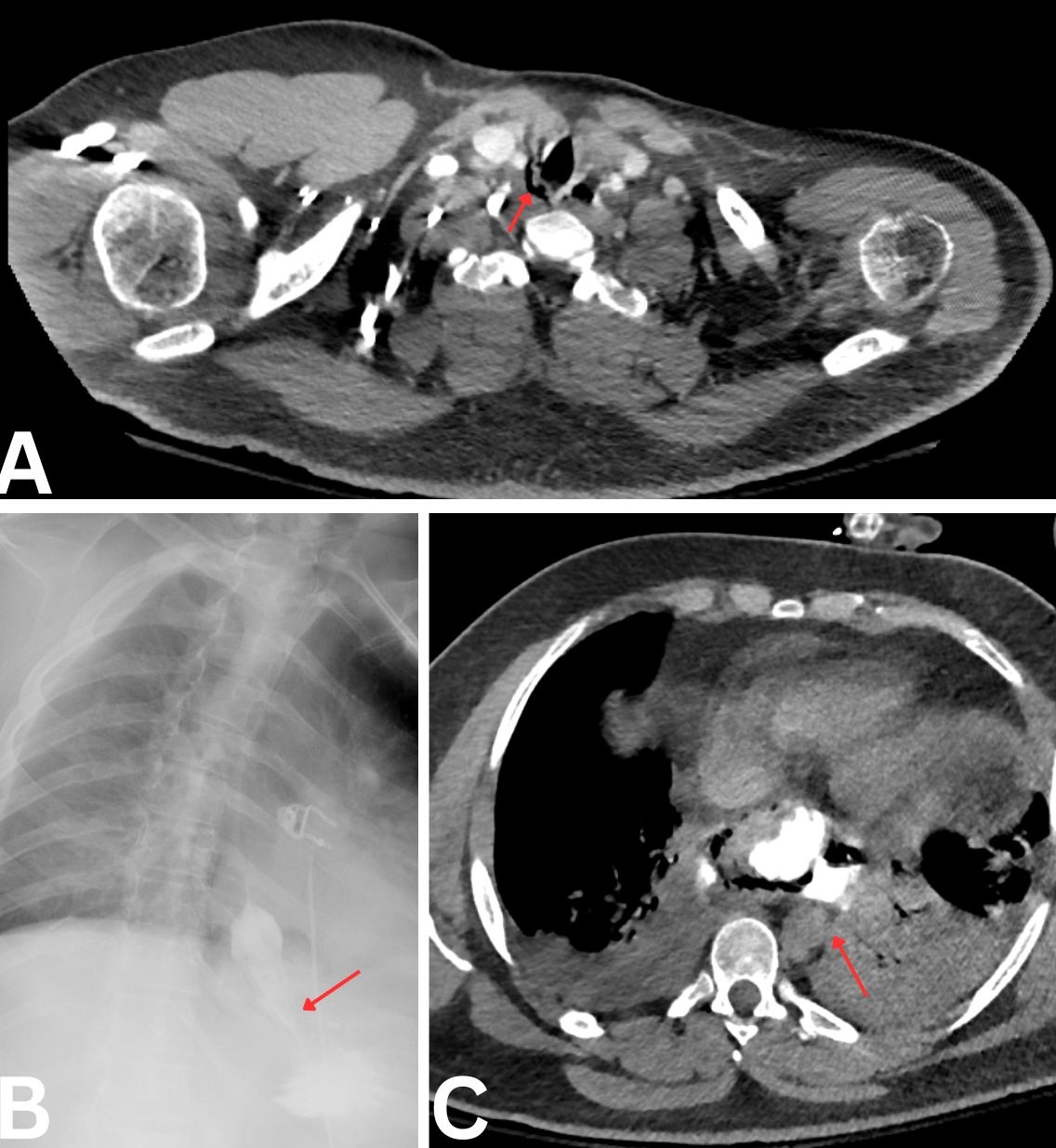
Figure: Figure 1.
A) CT Chest w/o contrast: Pneumomediastinum with hiatal hernia and perigastric stranding near the gastroesophageal junction, concerning for viscus perforation.
B) Gastrografin esophagogram without contrast extravasation.
C) CT Chest w/o contrast: Delayed imaging showing extraluminal oral contrast near the gastroesophageal junction.
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Asif Zamir, MD, FACG3. P2109 - Masquerading as Boerhaave: A Gastric Perforation at the GE Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, Edinburg, TX
Introduction: Pneumomediastinum is often attributed to esophageal perforation, particularly in the setting of Boerhaave syndrome. However, gastric perforations near surgically altered anatomies, such as Nissen fundoplication, can mimic this presentation. We present a rare case of contained gastric perforation at the gastroesophageal (GE) junction. Initially radiographically occult and ultimately diagnosed through delayed imaging and managed with endoscopic clipping.
Case Description/
Methods: A 31-year-old male with a history of mood disorder and prior Nissen fundoplication presented with acute retrosternal chest pain and dyspnea following a forceful coughing episode during a flu-like illness. He was tachycardic (heart rate 123), tachypneic (respiratory rate 30), and required 4L/min oxygen. Initial non-contrast CT chest demonstrated pneumomediastinum, perigastric stranding, and hiatal hernia with no clear perforation. Barium swallow with oral contrast again showed no extravasation. Due to further clinical deterioration, a subsequent non-contrast CT chest performed after the oral contrast had time to transit. It revealed extraluminal contrast pooling at the GE junction. This confirmed the gastric leak. Emergency upper endoscopy revealed a 1.5 cm deep linear ulcer on the posteroinferior fundus, due to the GE junction. It had fibrotic edges and mucosal edema suggestive of a chronic process. Sever through the scope clips (six Mantis and one resolution) were deployed, achieving complete closure. There was no residual leak on the confirmatory contrast study (Figure 1). The patient's respiratory status improved, and he was successfully managed with a full recovery.
Discussion: This case illustrates that gastric perforation near the GE junction, particularly in patients with prior Nissen fundoplication, can closely mimic Boerhaave syndrome. This case highlights that not all pneumomediastinum originates from the esophagus. Delayed imaging in the supine position can reveal subtle gastrointestinal leaks. Early endoscopic evaluation is critical when clinical suspicion persists despite the non-diagnostic imaging, promoting recognition. This may obviate the need for surgery in selected cases of gastric perforation.
Figure: Figure 1.
A) CT Chest w/o contrast: Pneumomediastinum with hiatal hernia and perigastric stranding near the gastroesophageal junction, concerning for viscus perforation.
B) Gastrografin esophagogram without contrast extravasation.
C) CT Chest w/o contrast: Delayed imaging showing extraluminal oral contrast near the gastroesophageal junction.
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Asif Zamir, MD, FACG3. P2109 - Masquerading as Boerhaave: A Gastric Perforation at the GE Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
