Sunday Poster Session
Category: Stomach and Spleen
P2070 - A Rare Presentation of Merkel Cell Carcinoma With Gastric Metastasis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- CD
Crystal Dorgalli, DO, MS
HCA Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Sarvanand Patel, MD1, Crystal Dorgalli, DO, MS1, Jennifer Hou, MD, PhD2, Fadi Totah, DO1, Tae Hun Kim, MD1, Pejman Solaimani, MD1
1HCA Riverside Community Hospital, Riverside, CA; 2HCA Healthcare Riverside Community Hospital, Riverside, CA
Introduction: Merkel cell carcinoma (MCC) is a rare and aggressive neoplasm of the skin. MCC impacts approximately 0.7 per 100,000 individuals each year, and the incidence is rising. Notably age, male gender, exposure to ultraviolet light, and immunosuppression are risk factors. MCC typically involves the head, neck, and extremities; less than 1% of cases involve gastric metastasis. In the United States, the 5-year survival rate for stage IV MCC is poor at 14%. Given the rarity of this disease, guidelines on the management for gastrointestinal (GI) involvement are limited. Thus, we present a case of MCC with gastric metastasis and performed a literature review of cases over the past decade to further enhance our understanding of this disease.
Case Description/
Methods: Herein, we present a case of a 77-year-old man with prior history of MCC who presented with acute anemia and melena. Physical exam revealed a fungating left neck mass. Labs showed low hemoglobin at 6.3 gm/dL. Upper endoscopy showed a large fungating mass in the gastric body (Fig. 1); pathology showed MCC (Fig. 2). The patient declined further surgical management of the gastric mass. He opted for adjuvant palliative radiation and chemotherapy.
Discussion: Based on current predictions that around 3200 individuals will be diagnosed with MCC each year in the United States alone, this further gives impetus for the need for effective diagnostic and treatment modalities given the highly aggressive character of this disease. To our knowledge, there have been approximately 30 cases of MCC with gastric metastasis reported to date. Our case report adds to the growing body of evidence over the past decade that MCC with gastric involvement continues to have poor prognosis. Most patients with gastric metastases present with melena and anemia (nine of twelve cases).
Endoscopy showed a range of mucosal lesions across cases. All eleven cases were cytokeratin-20 positive on histology (one case did not mention whether CK20 staining was done). Non-surgical management was pursued for most patients due to poor performance status (n=6); five patients underwent gastric resection; and one patient underwent embolization of tumor arteries. Chemotherapy was administered to four patients. Immunotherapy (with gastric resection) was used for two patients. Currently, there is no standardized treatment for MCC with gastric metastases. Given its aggressive nature, high clinical suspicion and close surveillance are necessary to improve outcomes.
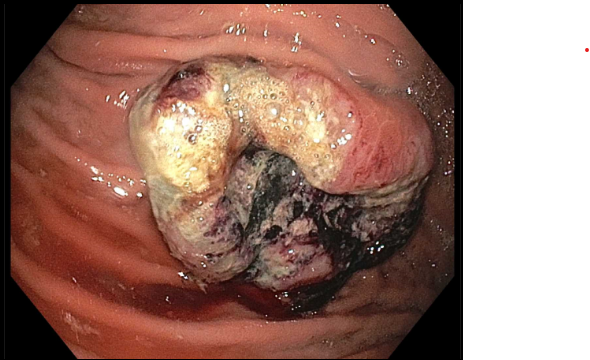
Figure: Figure 1. Endoscopic evaluation. Upper endoscopy showed a large fungating mass on the anterior wall of the gastric body. There was oozing blood, however no stigmata of active bleeding.
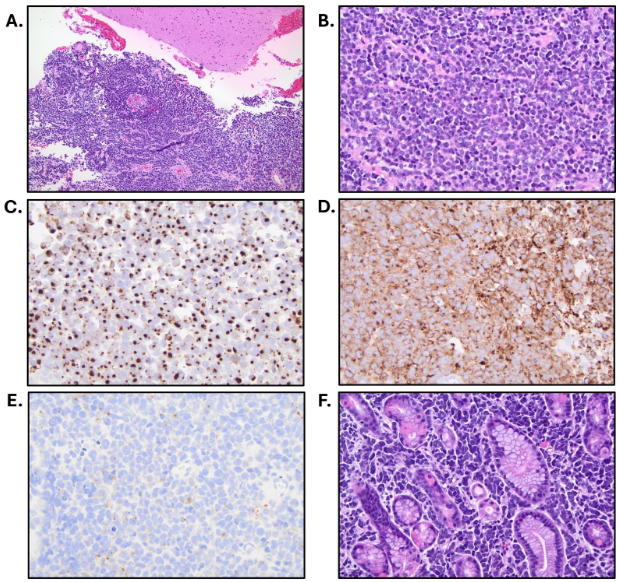
Figure: Figure 2. Histological findings reveal gastric metastasis of Merkel cell carcinoma. A) Sheets of neoplasm adjacent to brain parenchyma (200x). B) Sheets of neoplasm with high nuclear to cytoplasmic ratio, coarsely granular chromatin pattern, and high mitotic activity (400x). C) CK20 - perinuclear dot positivity. D) Synaptophysin positive. E) Chromogranin A positive. F) Sheets of neoplasm infiltrating between gastric oxyntic type mucosa (400x).
Disclosures:
Sarvanand Patel indicated no relevant financial relationships.
Crystal Dorgalli indicated no relevant financial relationships.
Jennifer Hou indicated no relevant financial relationships.
Fadi Totah indicated no relevant financial relationships.
Tae Hun Kim indicated no relevant financial relationships.
Pejman Solaimani indicated no relevant financial relationships.
Sarvanand Patel, MD1, Crystal Dorgalli, DO, MS1, Jennifer Hou, MD, PhD2, Fadi Totah, DO1, Tae Hun Kim, MD1, Pejman Solaimani, MD1. P2070 - A Rare Presentation of Merkel Cell Carcinoma With Gastric Metastasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sarvanand Patel, MD1, Crystal Dorgalli, DO, MS1, Jennifer Hou, MD, PhD2, Fadi Totah, DO1, Tae Hun Kim, MD1, Pejman Solaimani, MD1
1HCA Riverside Community Hospital, Riverside, CA; 2HCA Healthcare Riverside Community Hospital, Riverside, CA
Introduction: Merkel cell carcinoma (MCC) is a rare and aggressive neoplasm of the skin. MCC impacts approximately 0.7 per 100,000 individuals each year, and the incidence is rising. Notably age, male gender, exposure to ultraviolet light, and immunosuppression are risk factors. MCC typically involves the head, neck, and extremities; less than 1% of cases involve gastric metastasis. In the United States, the 5-year survival rate for stage IV MCC is poor at 14%. Given the rarity of this disease, guidelines on the management for gastrointestinal (GI) involvement are limited. Thus, we present a case of MCC with gastric metastasis and performed a literature review of cases over the past decade to further enhance our understanding of this disease.
Case Description/
Methods: Herein, we present a case of a 77-year-old man with prior history of MCC who presented with acute anemia and melena. Physical exam revealed a fungating left neck mass. Labs showed low hemoglobin at 6.3 gm/dL. Upper endoscopy showed a large fungating mass in the gastric body (Fig. 1); pathology showed MCC (Fig. 2). The patient declined further surgical management of the gastric mass. He opted for adjuvant palliative radiation and chemotherapy.
Discussion: Based on current predictions that around 3200 individuals will be diagnosed with MCC each year in the United States alone, this further gives impetus for the need for effective diagnostic and treatment modalities given the highly aggressive character of this disease. To our knowledge, there have been approximately 30 cases of MCC with gastric metastasis reported to date. Our case report adds to the growing body of evidence over the past decade that MCC with gastric involvement continues to have poor prognosis. Most patients with gastric metastases present with melena and anemia (nine of twelve cases).
Endoscopy showed a range of mucosal lesions across cases. All eleven cases were cytokeratin-20 positive on histology (one case did not mention whether CK20 staining was done). Non-surgical management was pursued for most patients due to poor performance status (n=6); five patients underwent gastric resection; and one patient underwent embolization of tumor arteries. Chemotherapy was administered to four patients. Immunotherapy (with gastric resection) was used for two patients. Currently, there is no standardized treatment for MCC with gastric metastases. Given its aggressive nature, high clinical suspicion and close surveillance are necessary to improve outcomes.
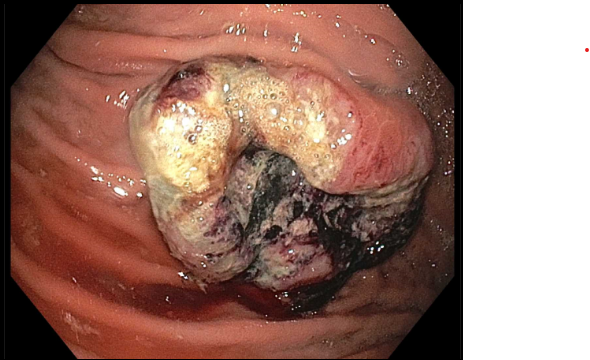
Figure: Figure 1. Endoscopic evaluation. Upper endoscopy showed a large fungating mass on the anterior wall of the gastric body. There was oozing blood, however no stigmata of active bleeding.
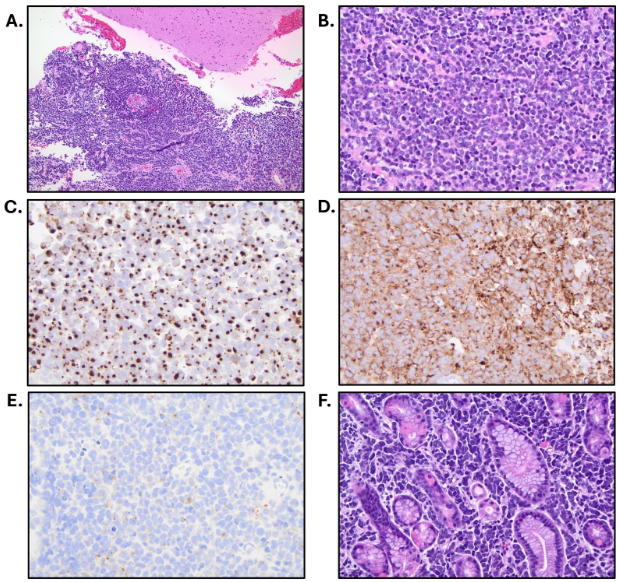
Figure: Figure 2. Histological findings reveal gastric metastasis of Merkel cell carcinoma. A) Sheets of neoplasm adjacent to brain parenchyma (200x). B) Sheets of neoplasm with high nuclear to cytoplasmic ratio, coarsely granular chromatin pattern, and high mitotic activity (400x). C) CK20 - perinuclear dot positivity. D) Synaptophysin positive. E) Chromogranin A positive. F) Sheets of neoplasm infiltrating between gastric oxyntic type mucosa (400x).
Disclosures:
Sarvanand Patel indicated no relevant financial relationships.
Crystal Dorgalli indicated no relevant financial relationships.
Jennifer Hou indicated no relevant financial relationships.
Fadi Totah indicated no relevant financial relationships.
Tae Hun Kim indicated no relevant financial relationships.
Pejman Solaimani indicated no relevant financial relationships.
Sarvanand Patel, MD1, Crystal Dorgalli, DO, MS1, Jennifer Hou, MD, PhD2, Fadi Totah, DO1, Tae Hun Kim, MD1, Pejman Solaimani, MD1. P2070 - A Rare Presentation of Merkel Cell Carcinoma With Gastric Metastasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


