Sunday Poster Session
Category: Stomach and Spleen
P2056 - Metabolic Profile Alterations as Early Indicators of GIST Recurrence and Imatinib Resistance
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Allen Luo, MD (he/him/his)
Keck School of Medicine of the University of Southern California, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2
1Keck School of Medicine of the University of Southern California, Moorpark, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors of the GI tract, occurring at a global rate of approximately 10–15 per million per year. Despite surgery and imatinib for high-risk cases, recurrence remains high, with a 5-year rate of 47%, often due to resistance from new kinase mutations. Imatinib affects lipid metabolism in patients with Chronic Myeloid Leukemia and GIST. This study examines metabolic trends in patients with recurrent GIST post-resection on imatinib and proposes that these biomarkers may help guide management in cases of resistance.
Methods: In this retrospective cohort study, we analyzed de‑identified patient records from the TriNetX database, which aggregates clinical data for more than 170 million patients across 145 healthcare systems in 18 countries. This study examined metabolic biomarkers including total cholesterol, triglycerides (TG), high density lipoprotein cholesterol (HDL-C), TG/HDL ratio, low density lipoprotein cholesterol (LDL-C), hemoglobin A1c, body mass index (BMI) and TSH.
Results: 36 patients were included in this analysis. On average, patients had resection surgery 25.9 months prior to recurrence diagnosis. Total cholesterol and LDL-C were significantly increasing (p< 0.05) with a high positive correlation (R=0.92, R=0.87) prior to time of recurrence. HDL-C was found to be significantly decreasing (p< 0.05) with a negative correlation (R=-0.70). BMI was also significantly elevated (p< 0.05) with a negligible correlation (R=-0.03). TG were found to have a significant high positive correlation (p< 0.05, R=0.93) and TSH was found to have a significant high negative correlation (p=0.049, R=-0.88). After recurrence was found, patients were started on 2nd and 3rd line therapies.
Discussion: This study found that patients who experienced GIST recurrence showed worsening metabolic profiles leading up to the diagnosis of recurrence. Specifically, total cholesterol, LDL, BMI, and triglycerides were trending up while HDL and TSH were trending down. Imatinib has been shown to have significant improvements in lipid and glycemic profiles in patients with GIST. As a result, the worsening of patients’ metabolic parameters leading up to the time of recurrence diagnosis may suggest imatinib resistance and recurrence. Therefore, we posit that these biomarkers can potentially be harnessed as tools for early detection of these events.
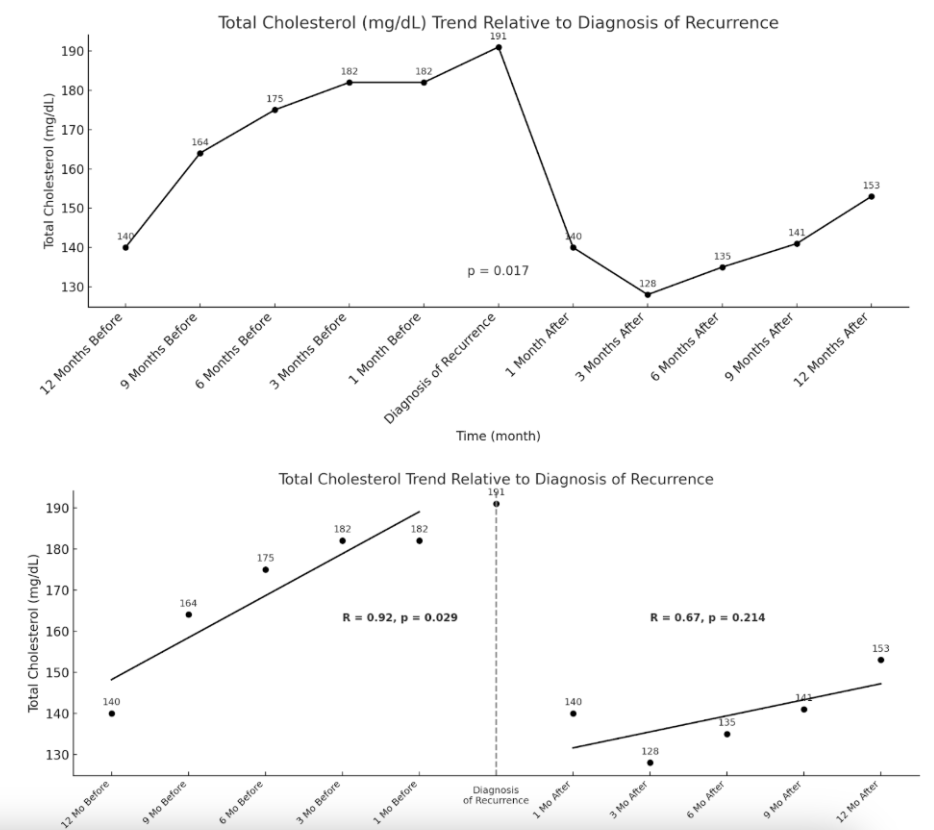
Figure: Figure 1. Total Cholesterol Trend Relative to Diagnosis of Recurrence

Figure: Figure 2. LDL-C Trend Relative to Diagnosis of Recurrence
Disclosures:
Allen Luo indicated no relevant financial relationships.
Allen Seylani indicated no relevant financial relationships.
Yohannes Haile indicated no relevant financial relationships.
Assal Sadighian indicated no relevant financial relationships.
Sadaf Sadighian indicated no relevant financial relationships.
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2. P2056 - Metabolic Profile Alterations as Early Indicators of GIST Recurrence and Imatinib Resistance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2
1Keck School of Medicine of the University of Southern California, Moorpark, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors of the GI tract, occurring at a global rate of approximately 10–15 per million per year. Despite surgery and imatinib for high-risk cases, recurrence remains high, with a 5-year rate of 47%, often due to resistance from new kinase mutations. Imatinib affects lipid metabolism in patients with Chronic Myeloid Leukemia and GIST. This study examines metabolic trends in patients with recurrent GIST post-resection on imatinib and proposes that these biomarkers may help guide management in cases of resistance.
Methods: In this retrospective cohort study, we analyzed de‑identified patient records from the TriNetX database, which aggregates clinical data for more than 170 million patients across 145 healthcare systems in 18 countries. This study examined metabolic biomarkers including total cholesterol, triglycerides (TG), high density lipoprotein cholesterol (HDL-C), TG/HDL ratio, low density lipoprotein cholesterol (LDL-C), hemoglobin A1c, body mass index (BMI) and TSH.
Results: 36 patients were included in this analysis. On average, patients had resection surgery 25.9 months prior to recurrence diagnosis. Total cholesterol and LDL-C were significantly increasing (p< 0.05) with a high positive correlation (R=0.92, R=0.87) prior to time of recurrence. HDL-C was found to be significantly decreasing (p< 0.05) with a negative correlation (R=-0.70). BMI was also significantly elevated (p< 0.05) with a negligible correlation (R=-0.03). TG were found to have a significant high positive correlation (p< 0.05, R=0.93) and TSH was found to have a significant high negative correlation (p=0.049, R=-0.88). After recurrence was found, patients were started on 2nd and 3rd line therapies.
Discussion: This study found that patients who experienced GIST recurrence showed worsening metabolic profiles leading up to the diagnosis of recurrence. Specifically, total cholesterol, LDL, BMI, and triglycerides were trending up while HDL and TSH were trending down. Imatinib has been shown to have significant improvements in lipid and glycemic profiles in patients with GIST. As a result, the worsening of patients’ metabolic parameters leading up to the time of recurrence diagnosis may suggest imatinib resistance and recurrence. Therefore, we posit that these biomarkers can potentially be harnessed as tools for early detection of these events.
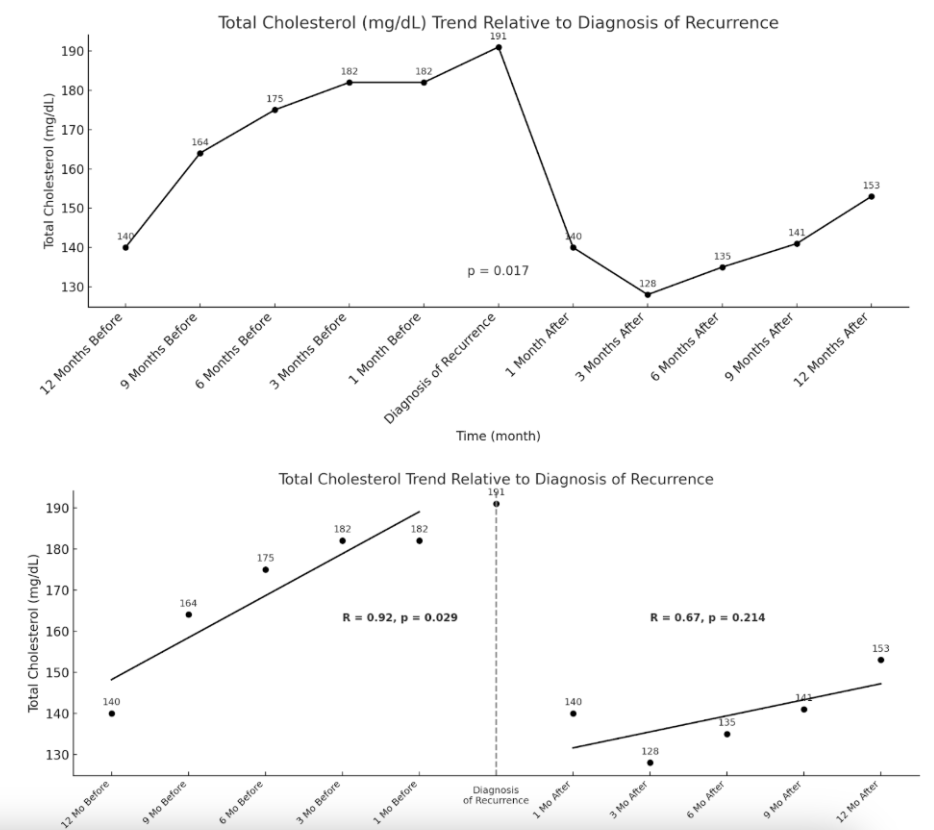
Figure: Figure 1. Total Cholesterol Trend Relative to Diagnosis of Recurrence

Figure: Figure 2. LDL-C Trend Relative to Diagnosis of Recurrence
Disclosures:
Allen Luo indicated no relevant financial relationships.
Allen Seylani indicated no relevant financial relationships.
Yohannes Haile indicated no relevant financial relationships.
Assal Sadighian indicated no relevant financial relationships.
Sadaf Sadighian indicated no relevant financial relationships.
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2. P2056 - Metabolic Profile Alterations as Early Indicators of GIST Recurrence and Imatinib Resistance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

