Sunday Poster Session
Category: Stomach and Spleen
P2042 - Open Surgical Technique Is Associated with Increased Risk of Candy Cane Syndrome: A Matched Case-Control Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tsola Efejuku, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Tsola Efejuku, MD1, Olivia Reszczynski, MD2, Tala Mahmoud, MD1, Donovan Hui, MD1, Thomas Shin, MD, PhD1, Alexander Podboy, MD2
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA
Introduction: Candy Cane Syndrome (CCS) is a complication of Roux-en-Y gastric bypass (RYGB) caused by a long or mispositioned blind afferent Roux limb distal to the gastrojejunostomy. This can result in abdominal pain, nausea, vomiting, and GERD, with symptom onset occurring weeks to years postoperatively. Diagnosis is reached through a combination of symptoms, upper GI series imaging, and endoscopy. As treatment options evolve, identifying patient characteristics associated with CCS is critical.
Methods: We conducted a retrospective propensity score–matched case-control study to compare patients with CCS to controls without CCS. Controls were matched 4:1 to cases based on age, sex, race, and BMI at the time of surgery using propensity scores. Clinical characteristics, comorbidities, ASA classification, and surgical approach were compared using standard statistical methods. All analyses were performed using R (version 4.5.0).
Results: Forty patients were included (8 CCS cases and 32 matched controls). No differences were observed in the matched variables: age (57.6 vs. 57.1 years, p=0.90), sex (87.5% vs. 90.6% female, p=1.00), race (87.5% White in both groups, p=1.00), or BMI (36.5 vs. 40.0 kg/m², p=0.40). CCS patients had significantly lower rates of hypertension (25% vs. 84.4%, p=0.001) and diabetes (0% vs. 46.8%, p=0.013). There were no differences in hyperlipidemia (p=0.45) or ASA classification (p=0.11). A logistic regression analysis was performed to identify factors independently associated with CCS. BMI was included in the model to adjust for residual imbalance, as matching was suboptimal for this variable. After adjustment, BMI was not significantly associated with CCS (OR 0.96, 95% CI: 0.87–1.06, p=0.445). In contrast, surgical approach was significantly associated with CCS, with patients who underwent an open approach having substantially higher odds of developing the condition (OR 32.2, 95% CI: 2.65–390.2, p=0.006).
Discussion: Our findings suggest that surgical approach may play a role in the development of CCS, with open surgery being significantly associated with increased odds of CCS. While comorbidities such as hypertension and diabetes were less common among CCS patients. Despite the use of propensity score matching to control for confounding, the sample size limits the precision and generalizability of these findings. Larger studies are warranted to validate these associations, inform surgical strategies to reduce CCS, and broaden the utility of endoscopic intervention for revision.
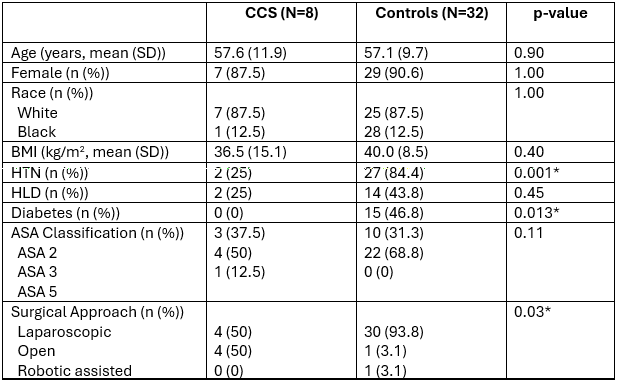
Figure: Table 1: Demographic table of CCS vs Control cases.
CCS: candy cane syndrome,; D: standard deviation; BMI: body mass index; HTN: hypertension; HLD: hyperlipidemia, ASA: American Society of Anesthesiologists
* represents statistical significance
Disclosures:
Tsola Efejuku indicated no relevant financial relationships.
Olivia Reszczynski indicated no relevant financial relationships.
Tala Mahmoud indicated no relevant financial relationships.
Donovan Hui indicated no relevant financial relationships.
Thomas Shin indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Tsola Efejuku, MD1, Olivia Reszczynski, MD2, Tala Mahmoud, MD1, Donovan Hui, MD1, Thomas Shin, MD, PhD1, Alexander Podboy, MD2. P2042 - Open Surgical Technique Is Associated with Increased Risk of Candy Cane Syndrome: A Matched Case-Control Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA
Introduction: Candy Cane Syndrome (CCS) is a complication of Roux-en-Y gastric bypass (RYGB) caused by a long or mispositioned blind afferent Roux limb distal to the gastrojejunostomy. This can result in abdominal pain, nausea, vomiting, and GERD, with symptom onset occurring weeks to years postoperatively. Diagnosis is reached through a combination of symptoms, upper GI series imaging, and endoscopy. As treatment options evolve, identifying patient characteristics associated with CCS is critical.
Methods: We conducted a retrospective propensity score–matched case-control study to compare patients with CCS to controls without CCS. Controls were matched 4:1 to cases based on age, sex, race, and BMI at the time of surgery using propensity scores. Clinical characteristics, comorbidities, ASA classification, and surgical approach were compared using standard statistical methods. All analyses were performed using R (version 4.5.0).
Results: Forty patients were included (8 CCS cases and 32 matched controls). No differences were observed in the matched variables: age (57.6 vs. 57.1 years, p=0.90), sex (87.5% vs. 90.6% female, p=1.00), race (87.5% White in both groups, p=1.00), or BMI (36.5 vs. 40.0 kg/m², p=0.40). CCS patients had significantly lower rates of hypertension (25% vs. 84.4%, p=0.001) and diabetes (0% vs. 46.8%, p=0.013). There were no differences in hyperlipidemia (p=0.45) or ASA classification (p=0.11). A logistic regression analysis was performed to identify factors independently associated with CCS. BMI was included in the model to adjust for residual imbalance, as matching was suboptimal for this variable. After adjustment, BMI was not significantly associated with CCS (OR 0.96, 95% CI: 0.87–1.06, p=0.445). In contrast, surgical approach was significantly associated with CCS, with patients who underwent an open approach having substantially higher odds of developing the condition (OR 32.2, 95% CI: 2.65–390.2, p=0.006).
Discussion: Our findings suggest that surgical approach may play a role in the development of CCS, with open surgery being significantly associated with increased odds of CCS. While comorbidities such as hypertension and diabetes were less common among CCS patients. Despite the use of propensity score matching to control for confounding, the sample size limits the precision and generalizability of these findings. Larger studies are warranted to validate these associations, inform surgical strategies to reduce CCS, and broaden the utility of endoscopic intervention for revision.
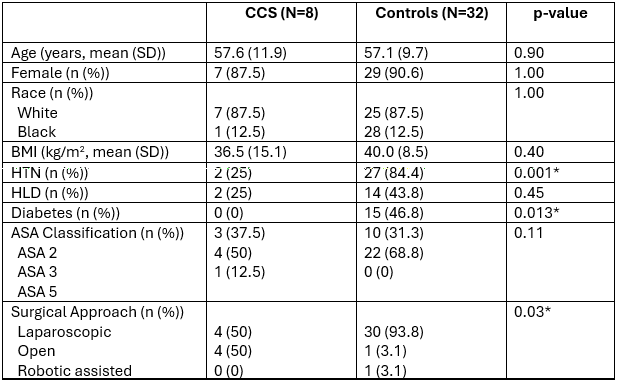
Figure: Table 1: Demographic table of CCS vs Control cases.
CCS: candy cane syndrome,; D: standard deviation; BMI: body mass index; HTN: hypertension; HLD: hyperlipidemia, ASA: American Society of Anesthesiologists
* represents statistical significance
Disclosures:
Tsola Efejuku indicated no relevant financial relationships.
Olivia Reszczynski indicated no relevant financial relationships.
Tala Mahmoud indicated no relevant financial relationships.
Donovan Hui indicated no relevant financial relationships.
Thomas Shin indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Tsola Efejuku, MD1, Olivia Reszczynski, MD2, Tala Mahmoud, MD1, Donovan Hui, MD1, Thomas Shin, MD, PhD1, Alexander Podboy, MD2. P2042 - Open Surgical Technique Is Associated with Increased Risk of Candy Cane Syndrome: A Matched Case-Control Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
