Sunday Poster Session
Category: Stomach and Spleen
P2034 - Revealing Prevalence and Mortality Risk of Gastrointestinal Malignancies After Solid Organ Transplantation: Insights From a National Data Registry
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Medora Doris Rodrigues, MD, MPH
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Medora Doris. Rodrigues, MD, MPH1, Jonathan Scott, MD2, Brian T. Lee, MD3, Anthony Firek, MD2, Mena Saad, DO4, Sanya Dhama, MD5, Wichit Srikureja, MD6, Khalid Mumtaz, MBBS, MSc1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Riverside University Health System, Riverside, CA; 3Hoag Liver Program, Hoag Digestive Health Institute, Hoag Hospital, Newport Beach, CA, Newport Beach, CA; 4Riverside University Health System, Moreno Valley, CA; 5UCR, Riverside, CA; 6Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Solid organ transplant recipients (SOTRs) are at increased risk for malignancies and, gastrointestinal (GI) malignancies-related mortality in this population is not well characterized. We aimed to evaluate post-transplant GI malignancy-related mortality using a national EHR database.
Methods: We performed a retrospective cohort study using the TriNetX Health Research Platform. Adult recipients of liver, kidney, heart, or lung transplants (2005-2025) without prior malignancy were included. GI cancers were identified using ICD codes. The primary outcome was mortality. Cox regression compared mortality by transplant type and GI malignancy.
Results: Of 83,021 SOTRs, 2,445 developed GI malignancy. They were older (59.7 ± 12.6 vs. 49.8 ± 16.7 years), more often male (66.6% vs. 60.4%), and more frequently White (58.6% vs. 49.6%) than those without malignancy (all p< 0.0001). Liver transplant recipients were disproportionately represented in the GI malignancy group (44.72% of cases, p < 0.0001). Nicotine dependence (13.9% vs. 8.07%), and alcohol-related disorders (15.49% vs. 7.86%) were more prevalent among those with GI malignancies (all p < 0.0001). Use of cyclosporine (12% vs. 9%, p < 0.0001) and Sirolimus (15% vs. 8%, p < 0.0001) was higher in the malignancy group. Mortality was 33% in the GI malignancy group vs. 15% in the non-malignancy group (RR 2.20, p< 0.0001).
Among SOTRs with GI malignancy, mortality was highest in renal transplant recipients, including esophageal (64%, HR 5.77), stomach (54.3%, HR 10.24), pancreatic (52%, HR 7.38), and colon cancers (39.5%, HR 3.79). Lung recipients also had worse outcomes, particularly with stomach (87%, HR 3.35), liver/ bile duct (73.5%, HR 3.18), and colon cancers (57.4%, HR 2.66). In contrast, liver recipients had lower mortality, including for liver/ bile duct cancers (21%, HR 1.14), possibly due to organ-specific surveillance or immunosuppressive regimens. Heart recipients had intermediate outcomes, with colon cancer mortality at 45.6% (HR 2.56).
Discussion: GI malignancies in SOTRs have markedly variable survival outcomes depending on cancer type and transplanted organ, with lung and renal recipients facing the highest mortality from stomach and colon cancers. Further research into transplant and malignancy-specific screening protocols and integrating these insights into post-transplant care pathways may enable earlier detection and improved survival in this high-risk population.
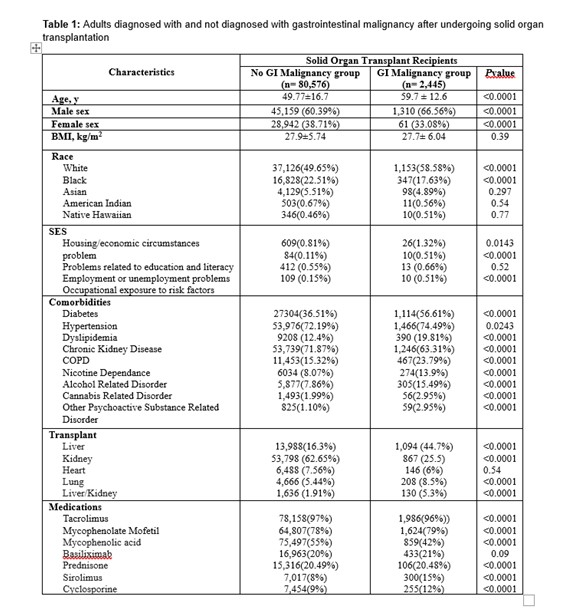
Figure: Adults diagnosed with and not diagnosed with gastrointestinal malignancy after undergoing solid organ transplantation.
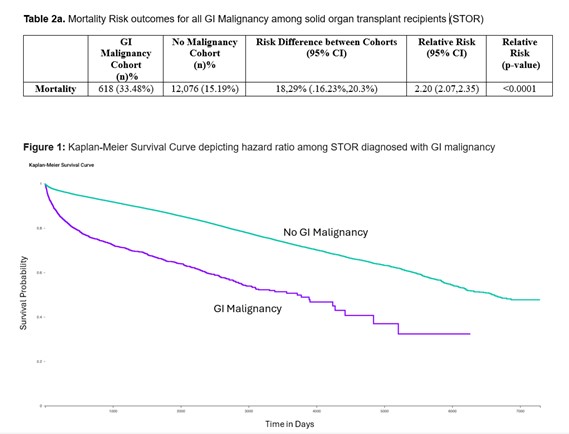
Figure: Mortality Risk outcome for all GI Malignancy among solid organ transplant recipients (STOR)
Disclosures:
Medora Rodrigues indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Brian Lee: Cook Medical – Advisor or Review Panel Member. Gilead Sciences – Consultant. Madrigal Pharmaceuticals – Advisor or Review Panel Member.
Anthony Firek indicated no relevant financial relationships.
Mena Saad indicated no relevant financial relationships.
Sanya Dhama indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Medora Doris. Rodrigues, MD, MPH1, Jonathan Scott, MD2, Brian T. Lee, MD3, Anthony Firek, MD2, Mena Saad, DO4, Sanya Dhama, MD5, Wichit Srikureja, MD6, Khalid Mumtaz, MBBS, MSc1. P2034 - Revealing Prevalence and Mortality Risk of Gastrointestinal Malignancies After Solid Organ Transplantation: Insights From a National Data Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Riverside University Health System, Riverside, CA; 3Hoag Liver Program, Hoag Digestive Health Institute, Hoag Hospital, Newport Beach, CA, Newport Beach, CA; 4Riverside University Health System, Moreno Valley, CA; 5UCR, Riverside, CA; 6Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Solid organ transplant recipients (SOTRs) are at increased risk for malignancies and, gastrointestinal (GI) malignancies-related mortality in this population is not well characterized. We aimed to evaluate post-transplant GI malignancy-related mortality using a national EHR database.
Methods: We performed a retrospective cohort study using the TriNetX Health Research Platform. Adult recipients of liver, kidney, heart, or lung transplants (2005-2025) without prior malignancy were included. GI cancers were identified using ICD codes. The primary outcome was mortality. Cox regression compared mortality by transplant type and GI malignancy.
Results: Of 83,021 SOTRs, 2,445 developed GI malignancy. They were older (59.7 ± 12.6 vs. 49.8 ± 16.7 years), more often male (66.6% vs. 60.4%), and more frequently White (58.6% vs. 49.6%) than those without malignancy (all p< 0.0001). Liver transplant recipients were disproportionately represented in the GI malignancy group (44.72% of cases, p < 0.0001). Nicotine dependence (13.9% vs. 8.07%), and alcohol-related disorders (15.49% vs. 7.86%) were more prevalent among those with GI malignancies (all p < 0.0001). Use of cyclosporine (12% vs. 9%, p < 0.0001) and Sirolimus (15% vs. 8%, p < 0.0001) was higher in the malignancy group. Mortality was 33% in the GI malignancy group vs. 15% in the non-malignancy group (RR 2.20, p< 0.0001).
Among SOTRs with GI malignancy, mortality was highest in renal transplant recipients, including esophageal (64%, HR 5.77), stomach (54.3%, HR 10.24), pancreatic (52%, HR 7.38), and colon cancers (39.5%, HR 3.79). Lung recipients also had worse outcomes, particularly with stomach (87%, HR 3.35), liver/ bile duct (73.5%, HR 3.18), and colon cancers (57.4%, HR 2.66). In contrast, liver recipients had lower mortality, including for liver/ bile duct cancers (21%, HR 1.14), possibly due to organ-specific surveillance or immunosuppressive regimens. Heart recipients had intermediate outcomes, with colon cancer mortality at 45.6% (HR 2.56).
Discussion: GI malignancies in SOTRs have markedly variable survival outcomes depending on cancer type and transplanted organ, with lung and renal recipients facing the highest mortality from stomach and colon cancers. Further research into transplant and malignancy-specific screening protocols and integrating these insights into post-transplant care pathways may enable earlier detection and improved survival in this high-risk population.
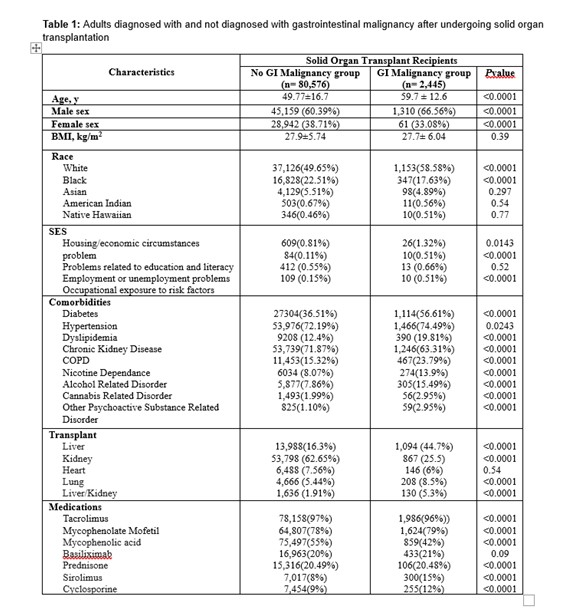
Figure: Adults diagnosed with and not diagnosed with gastrointestinal malignancy after undergoing solid organ transplantation.
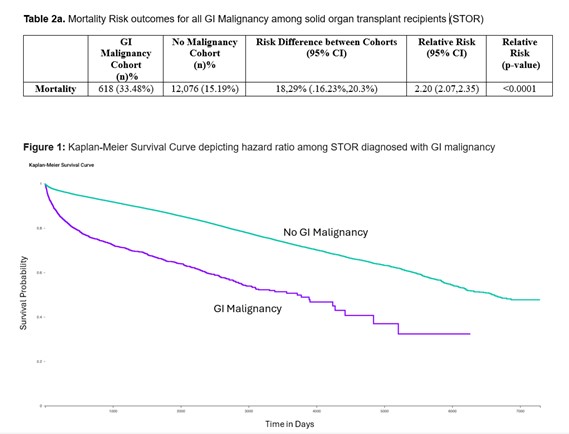
Figure: Mortality Risk outcome for all GI Malignancy among solid organ transplant recipients (STOR)
Disclosures:
Medora Rodrigues indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Brian Lee: Cook Medical – Advisor or Review Panel Member. Gilead Sciences – Consultant. Madrigal Pharmaceuticals – Advisor or Review Panel Member.
Anthony Firek indicated no relevant financial relationships.
Mena Saad indicated no relevant financial relationships.
Sanya Dhama indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Medora Doris. Rodrigues, MD, MPH1, Jonathan Scott, MD2, Brian T. Lee, MD3, Anthony Firek, MD2, Mena Saad, DO4, Sanya Dhama, MD5, Wichit Srikureja, MD6, Khalid Mumtaz, MBBS, MSc1. P2034 - Revealing Prevalence and Mortality Risk of Gastrointestinal Malignancies After Solid Organ Transplantation: Insights From a National Data Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
