Sunday Poster Session
Category: Stomach and Spleen
P2030 - The MAFLD Paradox: Lower Risk of Marginal Ulcers but Elevated Mortality After Gastric Bypass
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rashid Abdel-Razeq, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Rashid Abdel-Razeq, MD1, Somtochukwu Onwuzo, MD2, Mohamad-Noor Abu-Hammour, MD3, Antoine Boustany, MD4, Chidera Onwuzo, MBBS5, Kojo-Frimpong B. Awuah, MD6
1Cleveland Clinic Foundation, Cleveland, OH; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Cleveland Clinic, Cleveland, OH; 4Division of Gastroenterology, Department of Internal Medicine, University of Florida College of Medicine, Jacksonville, FL; 5SUNY Upstate Medical University Hospital, Syracuse, NY; 6Allegheny Health Network, Pittsburgh, PA
Introduction: Roux-en-Y gastric bypass (RYGB) is a common bariatric procedure, offering significant benefits for weight loss and metabolic function among patients with obesity. However, the presence of comorbid diseases such as metabolic dysfunction-associated fatty liver disease (MAFLD) may significantly alter the post-operative outcomes given the systematic inflammation and metabolic derangements associated with this condition. Marginal ulcers are a known complication following RYGB with an incidence that can reach up to 36%. Although several studies have assessed complications among RYGB patients, none of them specifically deal with how MAFLD affects mortality and the risk of marginal ulcers post-surgery, making this a relatively unexplored area. These are critical parameters, as they greatly impact recovery, quality of life, and health in the long term. This study aims to compare the incidence of marginal ulcers in patients with and without MAFLD undergoing RYGB.
Methods: This retrospective cohort study utilized TriNetX Global Collaborative Network to evaluate outcomes in adult patients who underwent RYGB. First cohort consisted of patients with MAFLD (n=13,165) and those without MAFLD (n=29,448). Propensity score matching was applied to balance baseline characteristics and comorbidities resulting in 12,435 patients in each cohort after matching. The outcomes evaluated within one year following surgery, were marginal ulcers and mortality. Statistical analyses included risk comparisons, Kaplan-Meier survival analysis, and hazard ratios, with significance defined as p < 0.05.
Results: The incidence of marginal ulcers was significantly lower in patients with NAFLD compared to those without MAFLD (3.9% vs. 4.9%; OR: 0.78, 95% CI: 0.69–0.89, p < 0.001). Mortality was higher in the MAFLD cohort (0.6%) compared to the non-MAFLD cohort (0.4%), though this difference did not reach statistical significance (OR: 1.36, 95% CI: 0.95–1.94, p = 0.088). These findings highlight that MAFLD may influence post-gastric bypass outcomes, offering potential protection against marginal ulcers but with a trend toward increased mortality.
Discussion: MAFLD was associated with a significantly lower risk of marginal ulcers following RYGB, suggesting a potential protective effect. However, a trend toward increased mortality in the MAFLD cohort, though not statistically significant, highlights the need for further research to understand the underlying mechanisms and optimize perioperative management in this population.
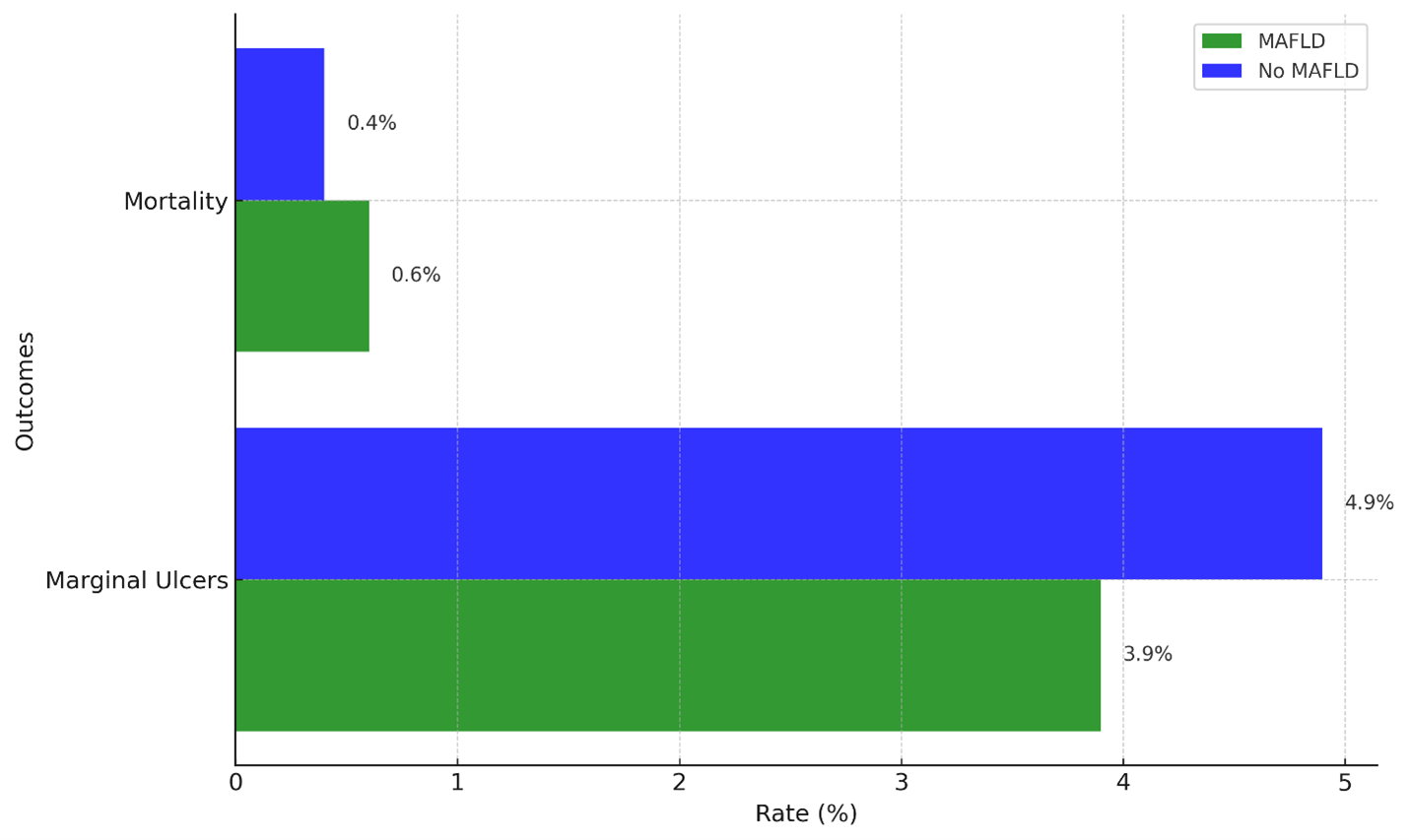
Figure: Figure 1 Comparison of marginal ulcer and mortality rates within one-year post-gastric bypass surgery between MAFLD and No MAFLD cohorts, showing lower marginal ulcer rates but a trend toward higher mortality in the MAFLD group.
Disclosures:
Rashid Abdel-Razeq indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq, MD1, Somtochukwu Onwuzo, MD2, Mohamad-Noor Abu-Hammour, MD3, Antoine Boustany, MD4, Chidera Onwuzo, MBBS5, Kojo-Frimpong B. Awuah, MD6. P2030 - The MAFLD Paradox: Lower Risk of Marginal Ulcers but Elevated Mortality After Gastric Bypass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Cleveland Clinic, Cleveland, OH; 4Division of Gastroenterology, Department of Internal Medicine, University of Florida College of Medicine, Jacksonville, FL; 5SUNY Upstate Medical University Hospital, Syracuse, NY; 6Allegheny Health Network, Pittsburgh, PA
Introduction: Roux-en-Y gastric bypass (RYGB) is a common bariatric procedure, offering significant benefits for weight loss and metabolic function among patients with obesity. However, the presence of comorbid diseases such as metabolic dysfunction-associated fatty liver disease (MAFLD) may significantly alter the post-operative outcomes given the systematic inflammation and metabolic derangements associated with this condition. Marginal ulcers are a known complication following RYGB with an incidence that can reach up to 36%. Although several studies have assessed complications among RYGB patients, none of them specifically deal with how MAFLD affects mortality and the risk of marginal ulcers post-surgery, making this a relatively unexplored area. These are critical parameters, as they greatly impact recovery, quality of life, and health in the long term. This study aims to compare the incidence of marginal ulcers in patients with and without MAFLD undergoing RYGB.
Methods: This retrospective cohort study utilized TriNetX Global Collaborative Network to evaluate outcomes in adult patients who underwent RYGB. First cohort consisted of patients with MAFLD (n=13,165) and those without MAFLD (n=29,448). Propensity score matching was applied to balance baseline characteristics and comorbidities resulting in 12,435 patients in each cohort after matching. The outcomes evaluated within one year following surgery, were marginal ulcers and mortality. Statistical analyses included risk comparisons, Kaplan-Meier survival analysis, and hazard ratios, with significance defined as p < 0.05.
Results: The incidence of marginal ulcers was significantly lower in patients with NAFLD compared to those without MAFLD (3.9% vs. 4.9%; OR: 0.78, 95% CI: 0.69–0.89, p < 0.001). Mortality was higher in the MAFLD cohort (0.6%) compared to the non-MAFLD cohort (0.4%), though this difference did not reach statistical significance (OR: 1.36, 95% CI: 0.95–1.94, p = 0.088). These findings highlight that MAFLD may influence post-gastric bypass outcomes, offering potential protection against marginal ulcers but with a trend toward increased mortality.
Discussion: MAFLD was associated with a significantly lower risk of marginal ulcers following RYGB, suggesting a potential protective effect. However, a trend toward increased mortality in the MAFLD cohort, though not statistically significant, highlights the need for further research to understand the underlying mechanisms and optimize perioperative management in this population.
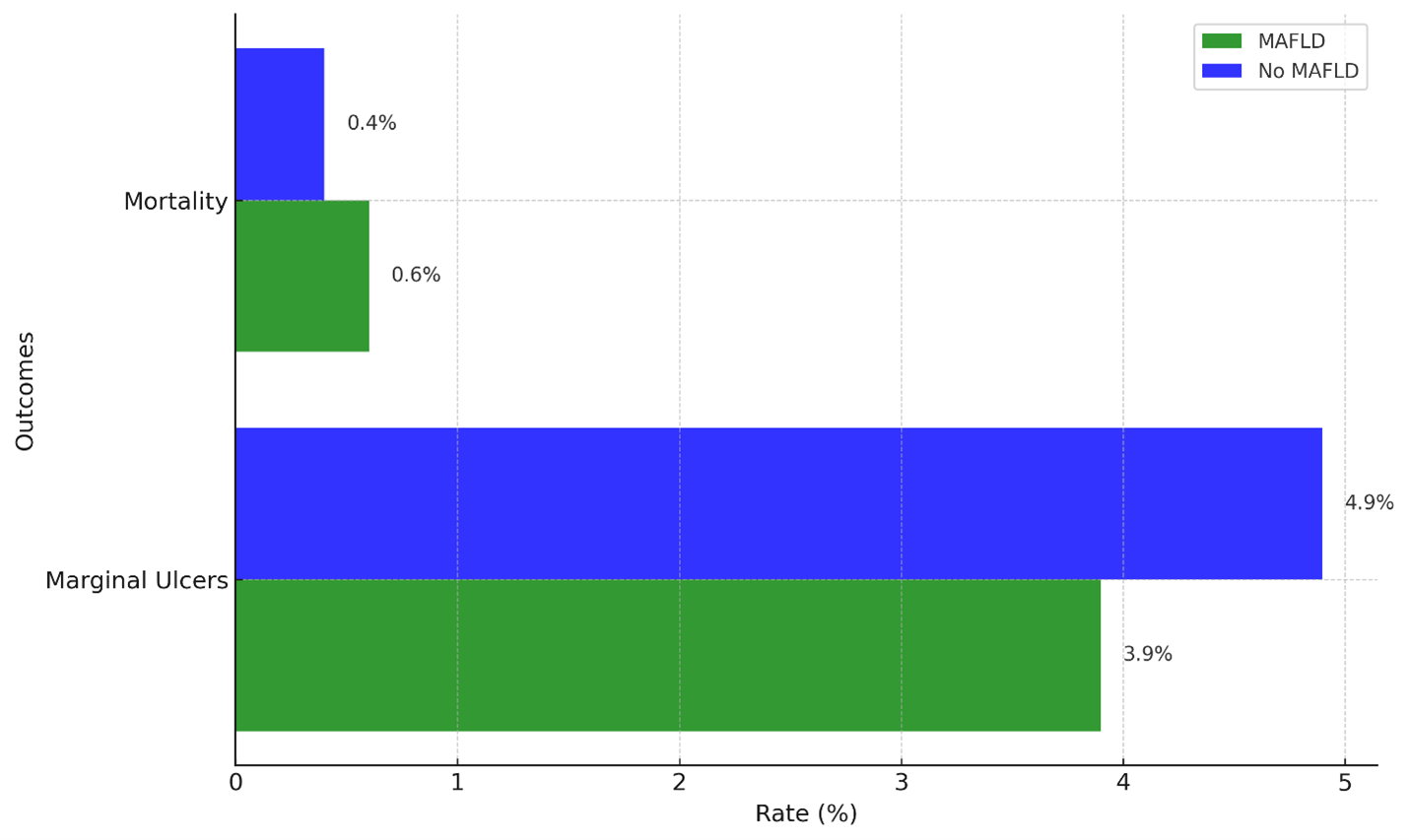
Figure: Figure 1 Comparison of marginal ulcer and mortality rates within one-year post-gastric bypass surgery between MAFLD and No MAFLD cohorts, showing lower marginal ulcer rates but a trend toward higher mortality in the MAFLD group.
Disclosures:
Rashid Abdel-Razeq indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq, MD1, Somtochukwu Onwuzo, MD2, Mohamad-Noor Abu-Hammour, MD3, Antoine Boustany, MD4, Chidera Onwuzo, MBBS5, Kojo-Frimpong B. Awuah, MD6. P2030 - The MAFLD Paradox: Lower Risk of Marginal Ulcers but Elevated Mortality After Gastric Bypass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
