Monday Poster Session
Category: Biliary/Pancreas
P2246 - Metastatic Cholangiocarcinoma to the Duodenum Causing Perforation and Obstruction: A Rare and Catastrophic Manifestation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aakash Aakash, MD (he/him/his)
Florida State University
Cape Coral, FL
Presenting Author(s)
Fnu Aakash, MD1, Osama Abdur Rehman, MD1, Gautam Maddineni, MD1, Vivek Singh, MBBS2, Fnu Arti, MD3, Aasta Kumari, MD4, Sunny Kumar, MD5, Lane Sager, DO2, Shivam Singla, MBBS, MD6
1Florida State University, Cape Coral, FL; 2FLORIDA STATE UNIVERSITY, Cape Coral, FL; 3Saint Francis Medical Center, Monroe, LA; 4North Central Bronx Hospital, New York, NY; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Tidal Health Peninsula Regional, Salisbury, MD, Salisbury, MD
Introduction: Cholangiocarcinoma is a rare and aggressive malignancy originating from the biliary epithelium. It typically metastasizes to the liver, peritoneum, and lymph nodes. Gastrointestinal tract involvement is uncommon, and duodenal metastasis with perforation has rarely been reported. We present a rare case of metastatic biliary-type cholangiocarcinoma involving the duodenum, complicated by malignant perforation and gastric outlet obstruction.
Case Description/
Methods: A 74-year-old man with alcoholic cirrhosis and prior hepatocellular carcinoma presented with fatigue, hematemesis, and melena over two weeks. Laboratory evaluation revealed severe normocytic anemia (Hb 5.6 g/dL, Hct 19.4%), requiring transfusion. Esophagogastroduodenoscopy (EGD) showed a large ulcerated exophytic mass in the duodenal bulb. Biopsies demonstrated poorly differentiated carcinoma consistent with biliary-type cholangiocarcinoma. His hospital course was marked by recurrent melena, anorexia, and worsening constipation. Abdominal CT demonstrated duodenal wall thickening, a nodular cirrhotic liver, gastric distention, and signs concerning perforation. Repeat EGD showed an infiltrative mass nearly obstructing the duodenal lumen, with visual evidence of malignant perforation. A fully covered self-expanding metal stent (FCSEMS) was successfully deployed endoscopically to bridge the defect and relieve the obstruction. Post-procedural fluoroscopy showed no contrast extravasation.
Discussion: This case highlights a highly unusual presentation of metastatic cholangiocarcinoma to the duodenum with subsequent perforation—a complication likely resulting from transmural tumor invasion and necrosis. Duodenal involvement in cholangiocarcinoma
is exceedingly rare and may be overlooked, particularly in patients with overlapping hepatobiliary disease. Histopathology was essential for definitive diagnosis. Given the patient's limited surgical options, endoscopic stenting provided effective palliation by sealing the perforation and resolving the obstruction. This case underscores the importance of maintaining a broad differential for upper GI bleeding in patients with prior hepatobiliary malignancy. Early endoscopic assessment and minimally invasive therapeutic strategies can relieve symptoms and improve outcomes in complex oncologic presentations.
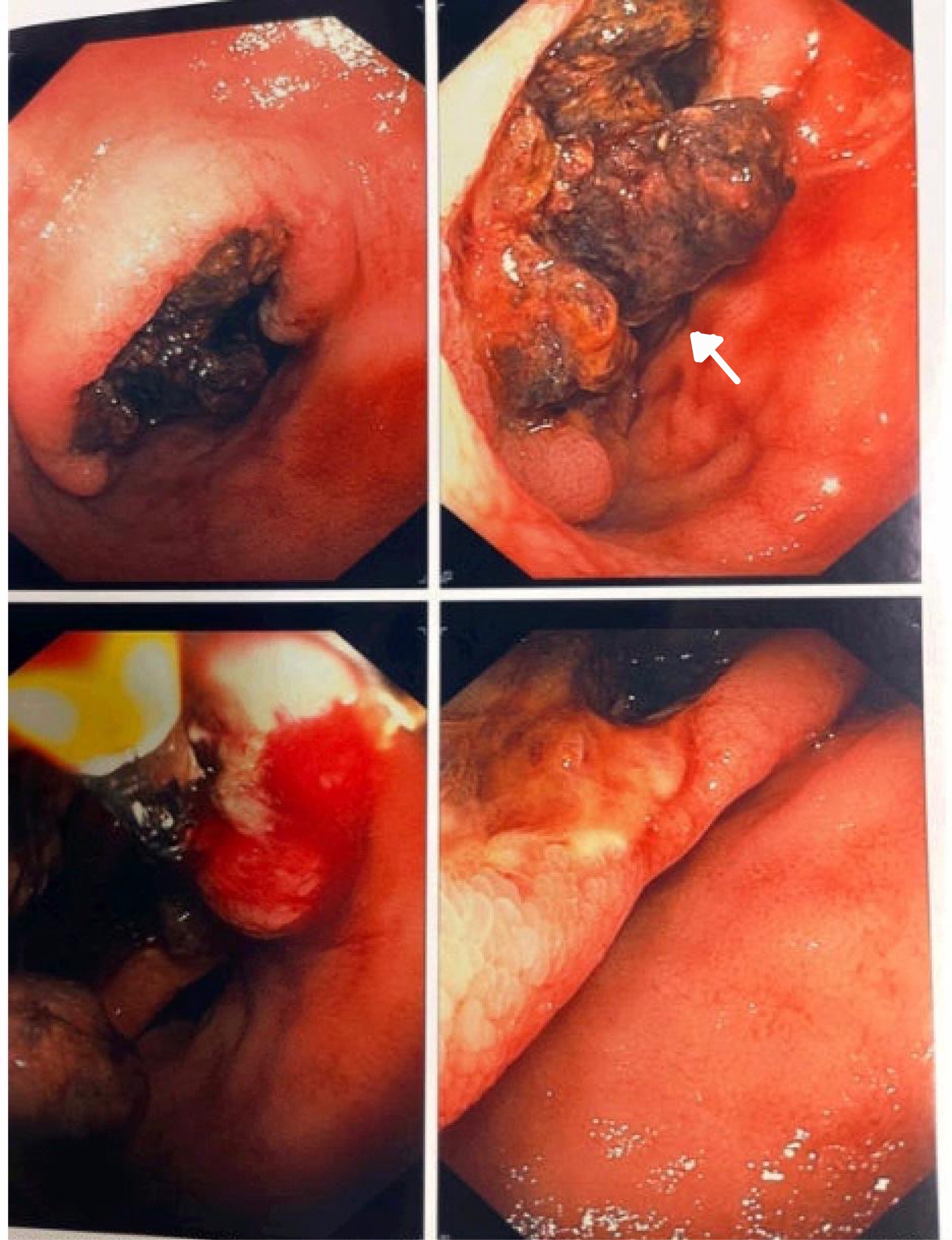
Figure: Figure 1: Endoscopic view showing a large infiltrative mass with deep central ulceration, causing near complete duodenal obstruction.

Figure: Figure 2: CT image showing ''mass 67.8 x 67.3 mm causing duodenal obstruction and erosion.''
Disclosures:
Fnu Aakash indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Vivek Singh indicated no relevant financial relationships.
Fnu Arti indicated no relevant financial relationships.
Aasta Kumari indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Lane Sager indicated no relevant financial relationships.
Shivam Singla indicated no relevant financial relationships.
Fnu Aakash, MD1, Osama Abdur Rehman, MD1, Gautam Maddineni, MD1, Vivek Singh, MBBS2, Fnu Arti, MD3, Aasta Kumari, MD4, Sunny Kumar, MD5, Lane Sager, DO2, Shivam Singla, MBBS, MD6. P2246 - Metastatic Cholangiocarcinoma to the Duodenum Causing Perforation and Obstruction: A Rare and Catastrophic Manifestation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Florida State University, Cape Coral, FL; 2FLORIDA STATE UNIVERSITY, Cape Coral, FL; 3Saint Francis Medical Center, Monroe, LA; 4North Central Bronx Hospital, New York, NY; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Tidal Health Peninsula Regional, Salisbury, MD, Salisbury, MD
Introduction: Cholangiocarcinoma is a rare and aggressive malignancy originating from the biliary epithelium. It typically metastasizes to the liver, peritoneum, and lymph nodes. Gastrointestinal tract involvement is uncommon, and duodenal metastasis with perforation has rarely been reported. We present a rare case of metastatic biliary-type cholangiocarcinoma involving the duodenum, complicated by malignant perforation and gastric outlet obstruction.
Case Description/
Methods: A 74-year-old man with alcoholic cirrhosis and prior hepatocellular carcinoma presented with fatigue, hematemesis, and melena over two weeks. Laboratory evaluation revealed severe normocytic anemia (Hb 5.6 g/dL, Hct 19.4%), requiring transfusion. Esophagogastroduodenoscopy (EGD) showed a large ulcerated exophytic mass in the duodenal bulb. Biopsies demonstrated poorly differentiated carcinoma consistent with biliary-type cholangiocarcinoma. His hospital course was marked by recurrent melena, anorexia, and worsening constipation. Abdominal CT demonstrated duodenal wall thickening, a nodular cirrhotic liver, gastric distention, and signs concerning perforation. Repeat EGD showed an infiltrative mass nearly obstructing the duodenal lumen, with visual evidence of malignant perforation. A fully covered self-expanding metal stent (FCSEMS) was successfully deployed endoscopically to bridge the defect and relieve the obstruction. Post-procedural fluoroscopy showed no contrast extravasation.
Discussion: This case highlights a highly unusual presentation of metastatic cholangiocarcinoma to the duodenum with subsequent perforation—a complication likely resulting from transmural tumor invasion and necrosis. Duodenal involvement in cholangiocarcinoma
is exceedingly rare and may be overlooked, particularly in patients with overlapping hepatobiliary disease. Histopathology was essential for definitive diagnosis. Given the patient's limited surgical options, endoscopic stenting provided effective palliation by sealing the perforation and resolving the obstruction. This case underscores the importance of maintaining a broad differential for upper GI bleeding in patients with prior hepatobiliary malignancy. Early endoscopic assessment and minimally invasive therapeutic strategies can relieve symptoms and improve outcomes in complex oncologic presentations.
Figure: Figure 1: Endoscopic view showing a large infiltrative mass with deep central ulceration, causing near complete duodenal obstruction.

Figure: Figure 2: CT image showing ''mass 67.8 x 67.3 mm causing duodenal obstruction and erosion.''
Disclosures:
Fnu Aakash indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Vivek Singh indicated no relevant financial relationships.
Fnu Arti indicated no relevant financial relationships.
Aasta Kumari indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Lane Sager indicated no relevant financial relationships.
Shivam Singla indicated no relevant financial relationships.
Fnu Aakash, MD1, Osama Abdur Rehman, MD1, Gautam Maddineni, MD1, Vivek Singh, MBBS2, Fnu Arti, MD3, Aasta Kumari, MD4, Sunny Kumar, MD5, Lane Sager, DO2, Shivam Singla, MBBS, MD6. P2246 - Metastatic Cholangiocarcinoma to the Duodenum Causing Perforation and Obstruction: A Rare and Catastrophic Manifestation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
