Monday Poster Session
Category: Biliary/Pancreas
P2232 - The Impact of Socioeconomic and Demographic Factors on Treatment Outcomes in Patients With Pancreatic Fluid Collections
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GS
Gurmun Singh Brar, MD
University of Toronto
Toronto, ON, Canada
Presenting Author(s)
Gurmun Brar, MD1, Maryam Mahjoob, 1, Kareem Khalaf, 2, Jeffrey Mosko, MD2, Christopher Teshima, MD2, Gary May, MD2, Natalia Calo, MD2
1University of Toronto, Toronto, ON, Canada; 2Unity Health Toronto, Toronto, ON, Canada
Introduction: Pancreatic fluid collections (PFCs) cause significant morbidity and contribute to healthcare burden. While minimally invasive drainage improves outcomes, the influence of social determinants of health (SDOH) on access, treatment, and outcomes remains underexplored. We aimed to evaluate associations between SDOH and long-term outcomes in patients undergoing PFC drainage at a tertiary care center.
Methods: We conducted a retrospective cohort study of consecutive adults who underwent PFC drainage at St. Michael’s Hospital, Toronto, from January 2016 to February 2024. Patient postal codes were linked to 2021 Canadian Census data to estimate income, housing, education, language, and Indigenous identity. Outcomes included clinical improvement (defined as the resolution of the drainage indication), radiologic resolution, and hospital readmission. Bivariate and multivariable logistic regression analyses were performed to assess associations.
Results: Among 193 patients (median age 53.9 years, 63.7% male), 91.1% underwent initial endoscopic drainage, most commonly for infection (27.0%). Bivariate analysis revealed that Indigenous identity was associated with greater use of percutaneous drainage (p=0.026), as well as higher rates of abdominal pain (p=0.010), opioid (p=0.001), and antibiotic prescriptions (p=0.017) at discharge. Substance use disorder (SUD) was associated with alcohol-related pancreatitis (p< 0.001), pain at discharge (p=0.022), prolonged PFC duration (p=0.005), and higher readmission rates (p=0.012). Lower median income was associated with lower rates of additional endoscopic drainage (p=0.043).
In multivariable models, Indigenous identity (OR 0.864 [0.779–0.958], p=0.005), shelter cost (OR 0.251 [0.093–0.671], p=0.006), and post-secondary education (OR 0.938 [0.892–0.987], p=0.014) were associated with lower odds of clinical improvement. Higher income (OR 1.100 [1.019–1.189], p=0.015) and spending >30% of income on shelter (OR 1.124 [1.057–1.195], p< 0.001) predicted greater improvement. SUD was linked to reduced odds of radiologic resolution (OR 0.436 [0.183–0.999], p=0.049). The income-to-shelter cost ratio predicted readmission (OR 1.031 [1.004–1.060], p=0.028).
Discussion: SDOH, including Indigenous identity, income, shelter cost, and SUD, were associated with disparities in the treatment and outcomes of PFC drainage. These findings support the integration of social risk screening and equity-focused care pathways to improve outcomes among vulnerable populations.
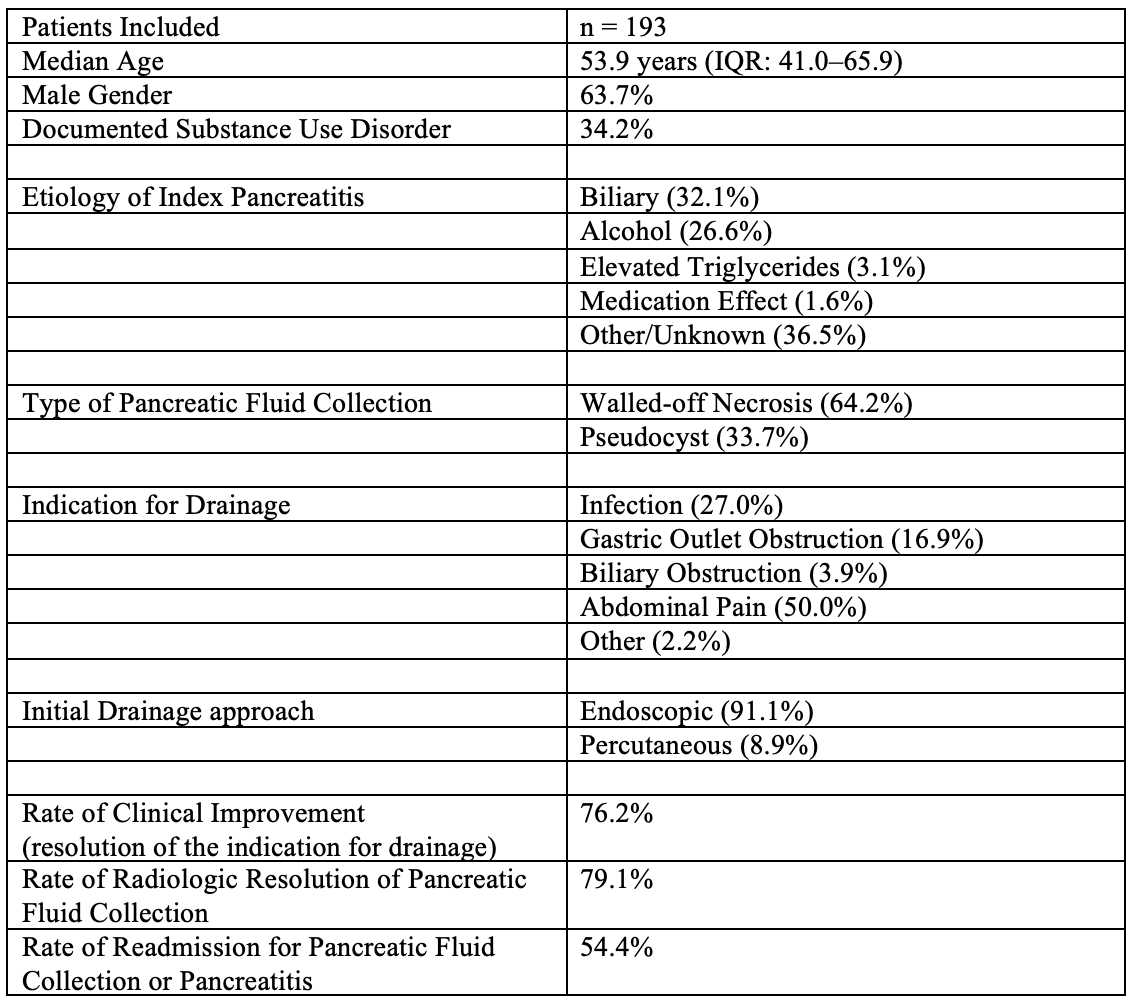
Figure: Table 1. Patient characteristics and key clinical outcomes of patients who underwent pancreatic fluid collection drainage (n=193)
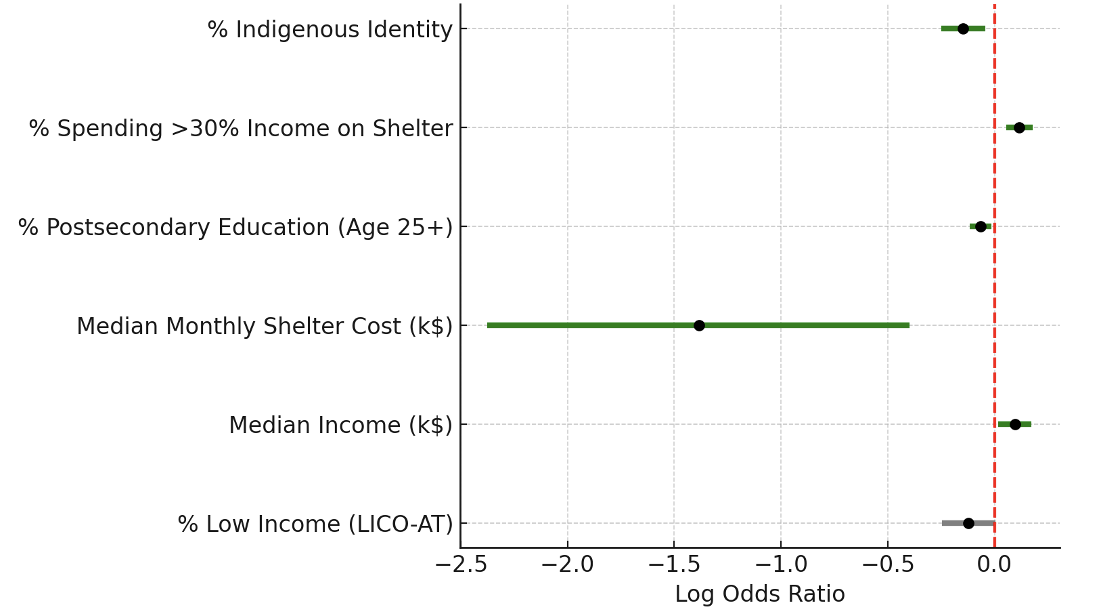
Figure: Figure 1. Forest plot of multivariable logistic regression: Social determinants predicting clinical improvement after pancreatic fluid collection drainage
Disclosures:
Gurmun Brar indicated no relevant financial relationships.
Maryam Mahjoob indicated no relevant financial relationships.
Kareem Khalaf indicated no relevant financial relationships.
Jeffrey Mosko indicated no relevant financial relationships.
Christopher Teshima indicated no relevant financial relationships.
Gary May indicated no relevant financial relationships.
Natalia Calo indicated no relevant financial relationships.
Gurmun Brar, MD1, Maryam Mahjoob, 1, Kareem Khalaf, 2, Jeffrey Mosko, MD2, Christopher Teshima, MD2, Gary May, MD2, Natalia Calo, MD2. P2232 - The Impact of Socioeconomic and Demographic Factors on Treatment Outcomes in Patients With Pancreatic Fluid Collections, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Toronto, Toronto, ON, Canada; 2Unity Health Toronto, Toronto, ON, Canada
Introduction: Pancreatic fluid collections (PFCs) cause significant morbidity and contribute to healthcare burden. While minimally invasive drainage improves outcomes, the influence of social determinants of health (SDOH) on access, treatment, and outcomes remains underexplored. We aimed to evaluate associations between SDOH and long-term outcomes in patients undergoing PFC drainage at a tertiary care center.
Methods: We conducted a retrospective cohort study of consecutive adults who underwent PFC drainage at St. Michael’s Hospital, Toronto, from January 2016 to February 2024. Patient postal codes were linked to 2021 Canadian Census data to estimate income, housing, education, language, and Indigenous identity. Outcomes included clinical improvement (defined as the resolution of the drainage indication), radiologic resolution, and hospital readmission. Bivariate and multivariable logistic regression analyses were performed to assess associations.
Results: Among 193 patients (median age 53.9 years, 63.7% male), 91.1% underwent initial endoscopic drainage, most commonly for infection (27.0%). Bivariate analysis revealed that Indigenous identity was associated with greater use of percutaneous drainage (p=0.026), as well as higher rates of abdominal pain (p=0.010), opioid (p=0.001), and antibiotic prescriptions (p=0.017) at discharge. Substance use disorder (SUD) was associated with alcohol-related pancreatitis (p< 0.001), pain at discharge (p=0.022), prolonged PFC duration (p=0.005), and higher readmission rates (p=0.012). Lower median income was associated with lower rates of additional endoscopic drainage (p=0.043).
In multivariable models, Indigenous identity (OR 0.864 [0.779–0.958], p=0.005), shelter cost (OR 0.251 [0.093–0.671], p=0.006), and post-secondary education (OR 0.938 [0.892–0.987], p=0.014) were associated with lower odds of clinical improvement. Higher income (OR 1.100 [1.019–1.189], p=0.015) and spending >30% of income on shelter (OR 1.124 [1.057–1.195], p< 0.001) predicted greater improvement. SUD was linked to reduced odds of radiologic resolution (OR 0.436 [0.183–0.999], p=0.049). The income-to-shelter cost ratio predicted readmission (OR 1.031 [1.004–1.060], p=0.028).
Discussion: SDOH, including Indigenous identity, income, shelter cost, and SUD, were associated with disparities in the treatment and outcomes of PFC drainage. These findings support the integration of social risk screening and equity-focused care pathways to improve outcomes among vulnerable populations.
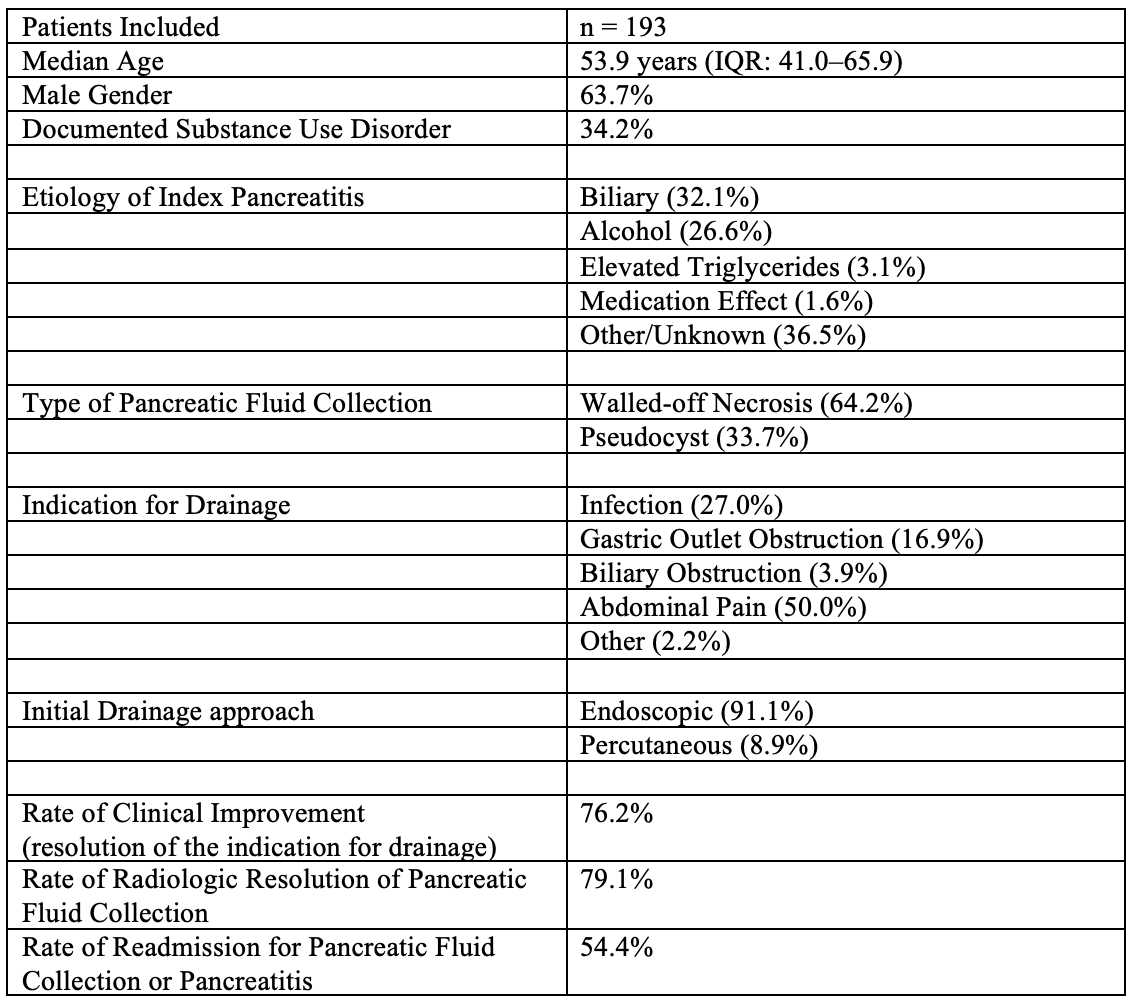
Figure: Table 1. Patient characteristics and key clinical outcomes of patients who underwent pancreatic fluid collection drainage (n=193)
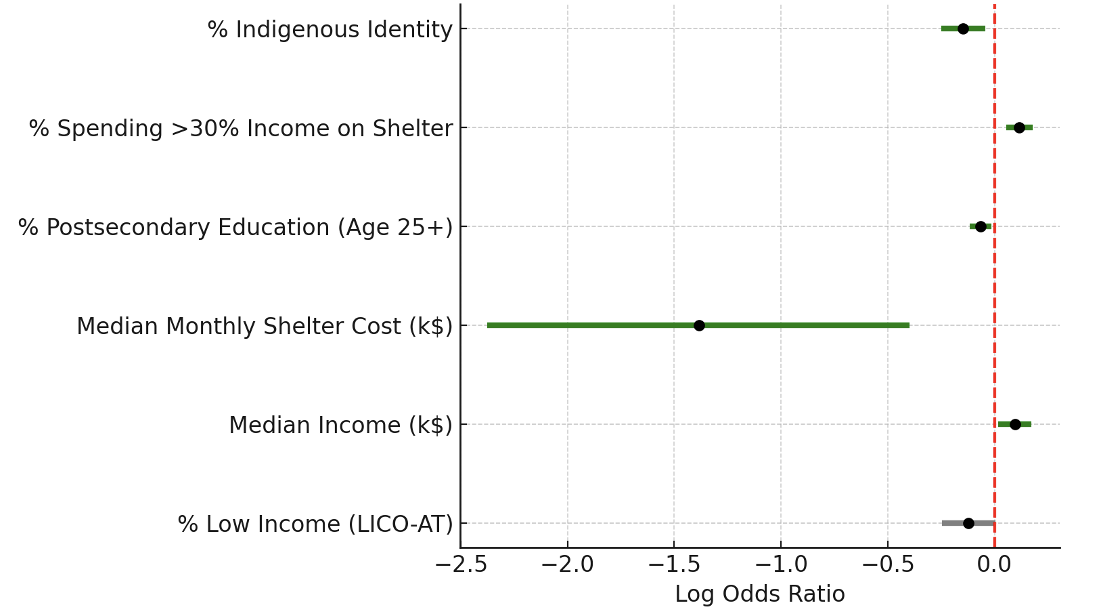
Figure: Figure 1. Forest plot of multivariable logistic regression: Social determinants predicting clinical improvement after pancreatic fluid collection drainage
Disclosures:
Gurmun Brar indicated no relevant financial relationships.
Maryam Mahjoob indicated no relevant financial relationships.
Kareem Khalaf indicated no relevant financial relationships.
Jeffrey Mosko indicated no relevant financial relationships.
Christopher Teshima indicated no relevant financial relationships.
Gary May indicated no relevant financial relationships.
Natalia Calo indicated no relevant financial relationships.
Gurmun Brar, MD1, Maryam Mahjoob, 1, Kareem Khalaf, 2, Jeffrey Mosko, MD2, Christopher Teshima, MD2, Gary May, MD2, Natalia Calo, MD2. P2232 - The Impact of Socioeconomic and Demographic Factors on Treatment Outcomes in Patients With Pancreatic Fluid Collections, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
