Monday Poster Session
Category: Biliary/Pancreas
P2229 - The Efficacy and Safety of Magnetic Compression Anastomosis in the Management of Biliary Obstruction: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hasan Al-Obaidi, MD
University of Toledo College of Medicine and Life Sciences
Toledo, OH
Presenting Author(s)
Sana Rabeeah, MD1, Hasan Al-Obaidi, MD2, Nooraldin Merza, MD2, Ali Wakil, MD3, Vikash Kumar, MD4, Sudheer Dhoop, MD5, Hayder Alamily, MD6, Bisher Sawaf, MD7, Pratiksha Moliya, MD8, Eunice Kwak, MD9, Manthanabhai Patel, MD2, Ali Nawras, MD1
1The University of Toledo, Toledo, OH; 2University of Toledo College of Medicine and Life Sciences, Toledo, OH; 3Brooklyn Hospital Center, Brooklyn, NY; 4Creighton University School of Medicine, Phoenix, AZ; 5University of Toledo, Toledo, OH; 6University of Colorado Anschutz Medical Campus, Denver, CO; 7University of Toledo Medical Center, Toledo, OH; 8University of Nebraska Medical Center, Omaha, NE; 9University of Toledo Health Sciences Campus, Toledo, OH
Introduction:
Background:
Biliary obstruction can lead to significant clinical complications, including jaundice, cholangitis, and malabsorption. While endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic biliary drainage (PTBD) are effective first-line treatments, they often fail in cases of complete ductal occlusion. Magnetic compression anastomosis (MCA) has emerged as a minimally invasive alternative for recanalizing obstructed ducts. This meta-analysis aims to evaluate MCA’s efficacy, complication rates, and clinical utility across diverse patient populations.
Methods: A comprehensive search of observational studies was conducted, with inclusion criteria focusing on studies evaluating MCA in biliary strictures. Technical success, recurrence rates, adverse events, procedural time, and time to recanalization were extracted and analyzed. A random-effects model was used for meta-analysis, with subgroup analyses to evaluate outcomes for first line versus salvage MCA. Sensitivity analyses were performed to assess the impact of study design and publication bias.
Results: Twenty-four studies with 403 biliary strictures were included. MCA demonstrated a high overall technical success rate (91.7%), with first-line use showing slightly higher success (95.9%) than salvage MCA. Procedural time and time to recanalization were comparable across subgroups. Complication rates, including cholangitis (7.4%), were low, and recurrence rates were higher for salvage MCA (13%) compared to first-line use (6.8%), though not statistically significant.
Discussion: MCA is a highly effective, minimally invasive option for refractory biliary strictures, offering high technical success rates even after failed conventional therapies. However, heterogeneity among studies and a lack of randomized controlled trials limit definitive conclusions. Standardized protocols and prospective studies are needed to further refine MCA’s clinical applications and establish its role as a standard therapy.
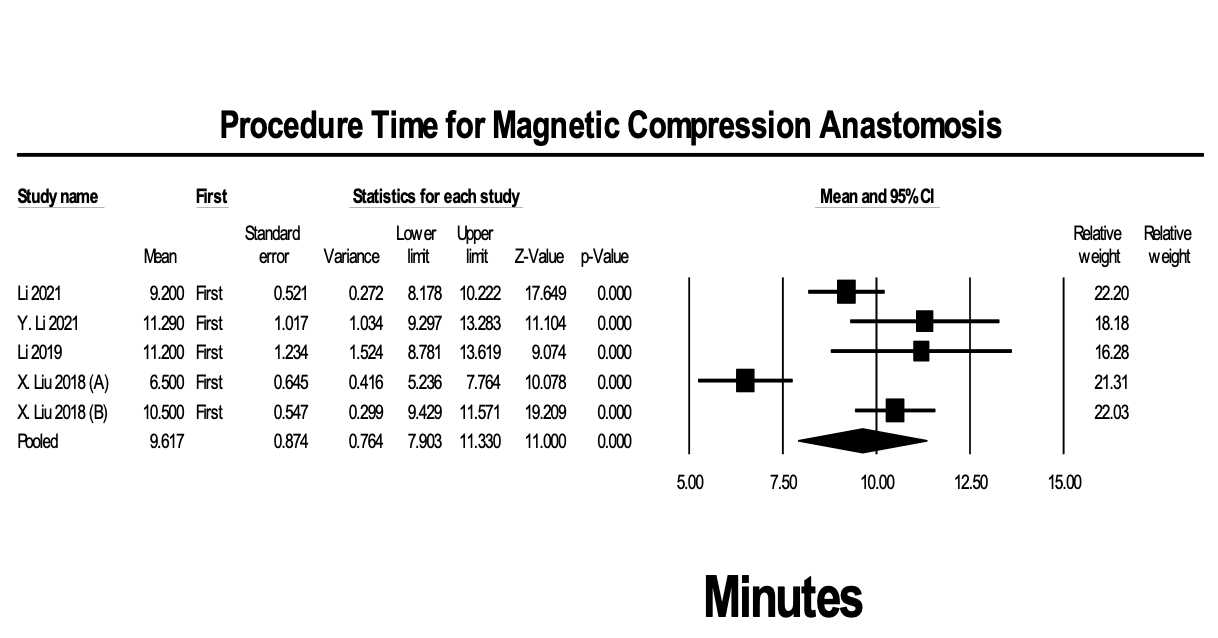
Figure: Figure1: Forest plot for procedural time.
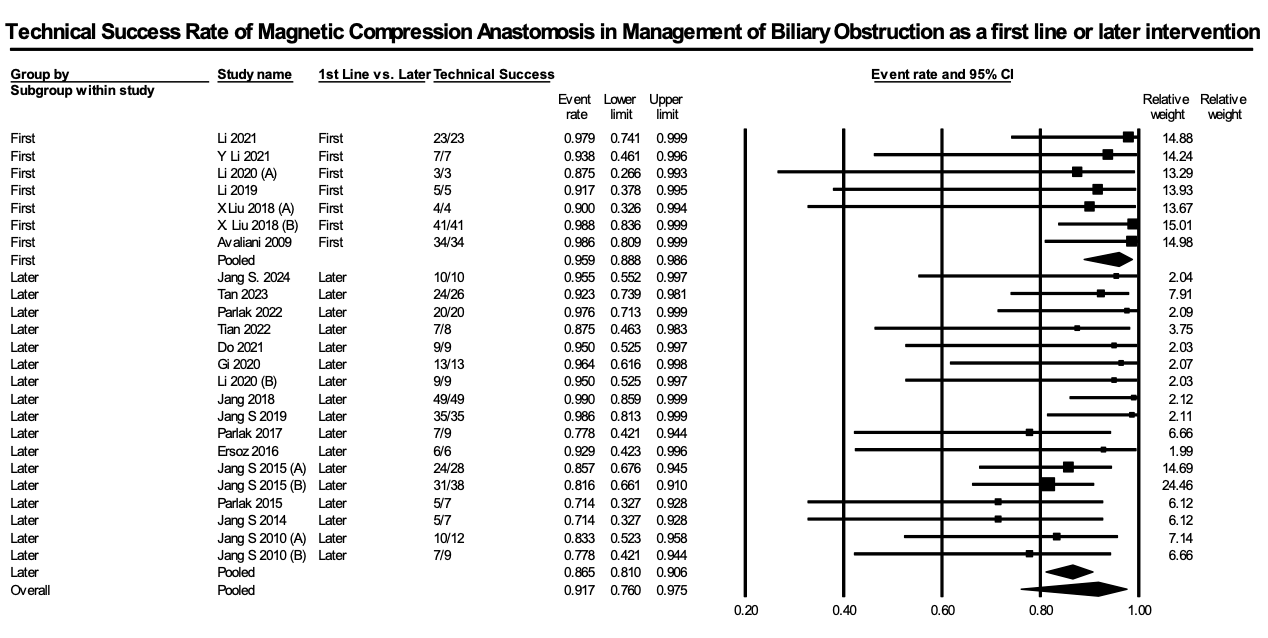
Figure: Figure 2: Forest plot for technical success rate.
Disclosures:
Sana Rabeeah indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Nooraldin Merza indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sudheer Dhoop indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Pratiksha Moliya indicated no relevant financial relationships.
Eunice Kwak indicated no relevant financial relationships.
Manthanabhai Patel indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Sana Rabeeah, MD1, Hasan Al-Obaidi, MD2, Nooraldin Merza, MD2, Ali Wakil, MD3, Vikash Kumar, MD4, Sudheer Dhoop, MD5, Hayder Alamily, MD6, Bisher Sawaf, MD7, Pratiksha Moliya, MD8, Eunice Kwak, MD9, Manthanabhai Patel, MD2, Ali Nawras, MD1. P2229 - The Efficacy and Safety of Magnetic Compression Anastomosis in the Management of Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The University of Toledo, Toledo, OH; 2University of Toledo College of Medicine and Life Sciences, Toledo, OH; 3Brooklyn Hospital Center, Brooklyn, NY; 4Creighton University School of Medicine, Phoenix, AZ; 5University of Toledo, Toledo, OH; 6University of Colorado Anschutz Medical Campus, Denver, CO; 7University of Toledo Medical Center, Toledo, OH; 8University of Nebraska Medical Center, Omaha, NE; 9University of Toledo Health Sciences Campus, Toledo, OH
Introduction:
Background:
Biliary obstruction can lead to significant clinical complications, including jaundice, cholangitis, and malabsorption. While endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic biliary drainage (PTBD) are effective first-line treatments, they often fail in cases of complete ductal occlusion. Magnetic compression anastomosis (MCA) has emerged as a minimally invasive alternative for recanalizing obstructed ducts. This meta-analysis aims to evaluate MCA’s efficacy, complication rates, and clinical utility across diverse patient populations.
Methods: A comprehensive search of observational studies was conducted, with inclusion criteria focusing on studies evaluating MCA in biliary strictures. Technical success, recurrence rates, adverse events, procedural time, and time to recanalization were extracted and analyzed. A random-effects model was used for meta-analysis, with subgroup analyses to evaluate outcomes for first line versus salvage MCA. Sensitivity analyses were performed to assess the impact of study design and publication bias.
Results: Twenty-four studies with 403 biliary strictures were included. MCA demonstrated a high overall technical success rate (91.7%), with first-line use showing slightly higher success (95.9%) than salvage MCA. Procedural time and time to recanalization were comparable across subgroups. Complication rates, including cholangitis (7.4%), were low, and recurrence rates were higher for salvage MCA (13%) compared to first-line use (6.8%), though not statistically significant.
Discussion: MCA is a highly effective, minimally invasive option for refractory biliary strictures, offering high technical success rates even after failed conventional therapies. However, heterogeneity among studies and a lack of randomized controlled trials limit definitive conclusions. Standardized protocols and prospective studies are needed to further refine MCA’s clinical applications and establish its role as a standard therapy.
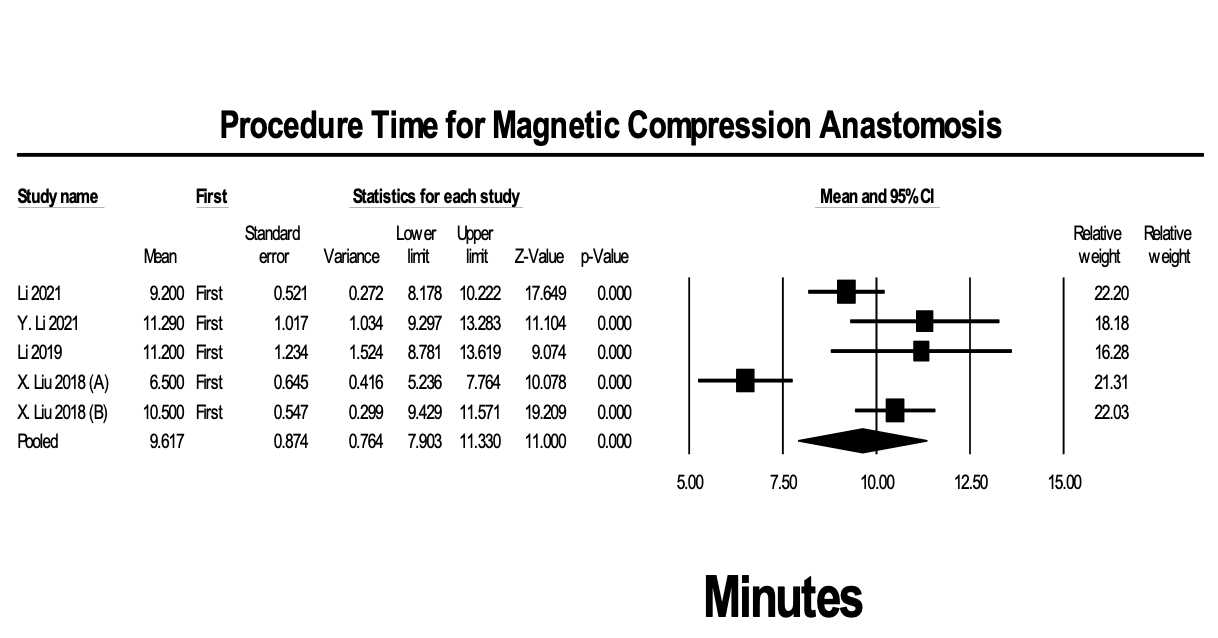
Figure: Figure1: Forest plot for procedural time.
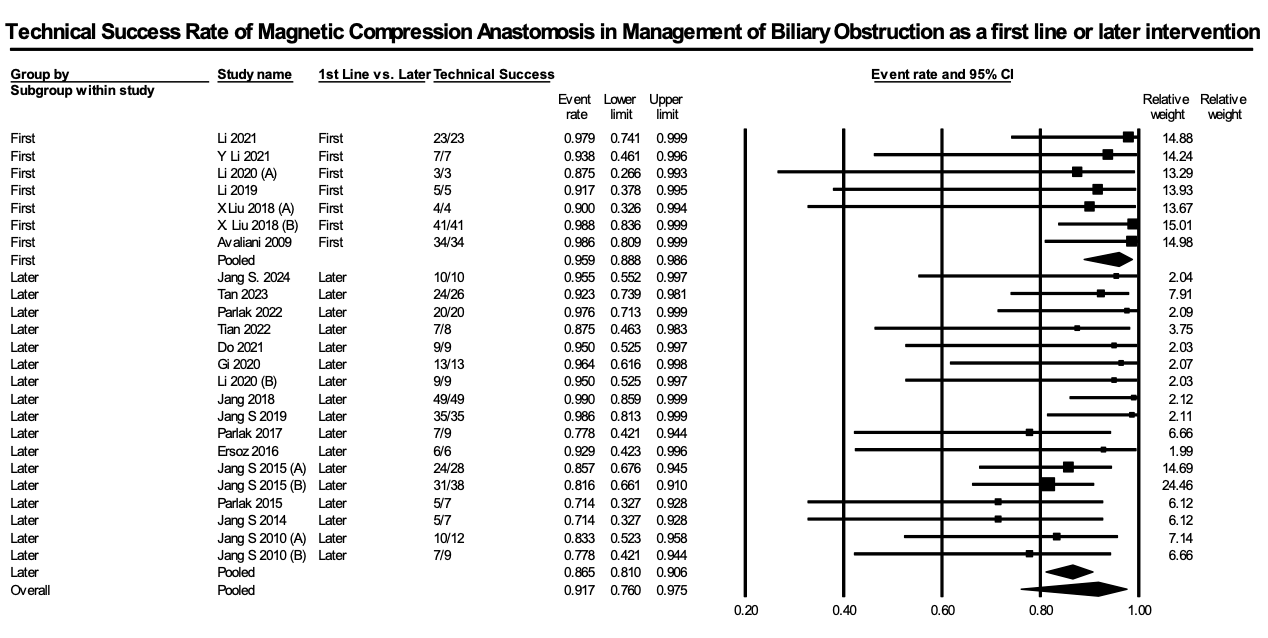
Figure: Figure 2: Forest plot for technical success rate.
Disclosures:
Sana Rabeeah indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Nooraldin Merza indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sudheer Dhoop indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Pratiksha Moliya indicated no relevant financial relationships.
Eunice Kwak indicated no relevant financial relationships.
Manthanabhai Patel indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Sana Rabeeah, MD1, Hasan Al-Obaidi, MD2, Nooraldin Merza, MD2, Ali Wakil, MD3, Vikash Kumar, MD4, Sudheer Dhoop, MD5, Hayder Alamily, MD6, Bisher Sawaf, MD7, Pratiksha Moliya, MD8, Eunice Kwak, MD9, Manthanabhai Patel, MD2, Ali Nawras, MD1. P2229 - The Efficacy and Safety of Magnetic Compression Anastomosis in the Management of Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
