Monday Poster Session
Category: Biliary/Pancreas
P2359 - An Unusual Cause of Biliary Obstruction: Hepatic Artery Pseudoaneurysm – A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Susan Feldman, MD (she/her/hers)
Prisma Health, University of South Carolina School of Medicine
Columbia, SC
Presenting Author(s)
Susan Feldman, MD, Aidan Warner, MD, Gabriella Gee, BS
University of South Carolina School of Medicine, Columbia, SC
Introduction: Hepatic artery pseudoaneurysms (HAPs) are rare vascular abnormalities that can present with life-threatening complications. While most HAPs occur secondary to hepatobiliary procedures or trauma, less common etiologies include malignancy and infection. A subset of HAPs can rupture into the biliary tract, resulting in hemobilia—a rare cause of upper gastrointestinal bleeding and obstructive jaundice. We present a case of HAP rupture resulting in hemobilia and biliary obstruction.
Case Description/
Methods: An 88-year-old woman with chronic lymphocytic leukemia (CLL) presented with melena and progressive jaundice. She had sustained a mechanical fall three days prior. Labs revealed anemia (Hgb 9.6), thrombocytopenia (Plt 27), leukocytosis (WBC 27.1), and a cholestatic liver injury pattern: AST 710, ALT 747, total bilirubin 8.9, direct bilirubin 6.7. ERCP revealed blood and sludge within the biliary tree; plastic stents were placed in the common bile duct and pancreatic duct. CT imaging showed an enhancing lesion concerning for a ruptured hepatic artery aneurysm. Interventional radiology confirmed a right hepatic artery pseudoaneurysm, which was successfully embolized with coils. Post-procedure, the patient developed worsening transaminitis and hyperbilirubinemia, consistent with hepatic ischemia. Despite supportive care, the patient was unable to recover.
Discussion: HAPs are exceedingly rare, comprising less than 20% of all visceral artery aneurysms, with rupture posing a high mortality risk. When ruptured into the biliary tract, they may cause "Quincke’s triad," described as jaundice, upper GI bleeding, and right upper quadrant pain. In this case, the patient’s CLL-associated thrombocytopenia likely exacerbated bleeding. Furthermore, embolization, while life-saving and necessary to this patient, carries its own risk for hepatic ischemia. This case highlights the need for considering vascular sources in atypical GI bleeds with cholestatic labs and highlights the rapid deterioration possible with HAP rupture. Timely diagnosis with cross-sectional imaging and prompt endovascular intervention remain essential to improve outcomes.
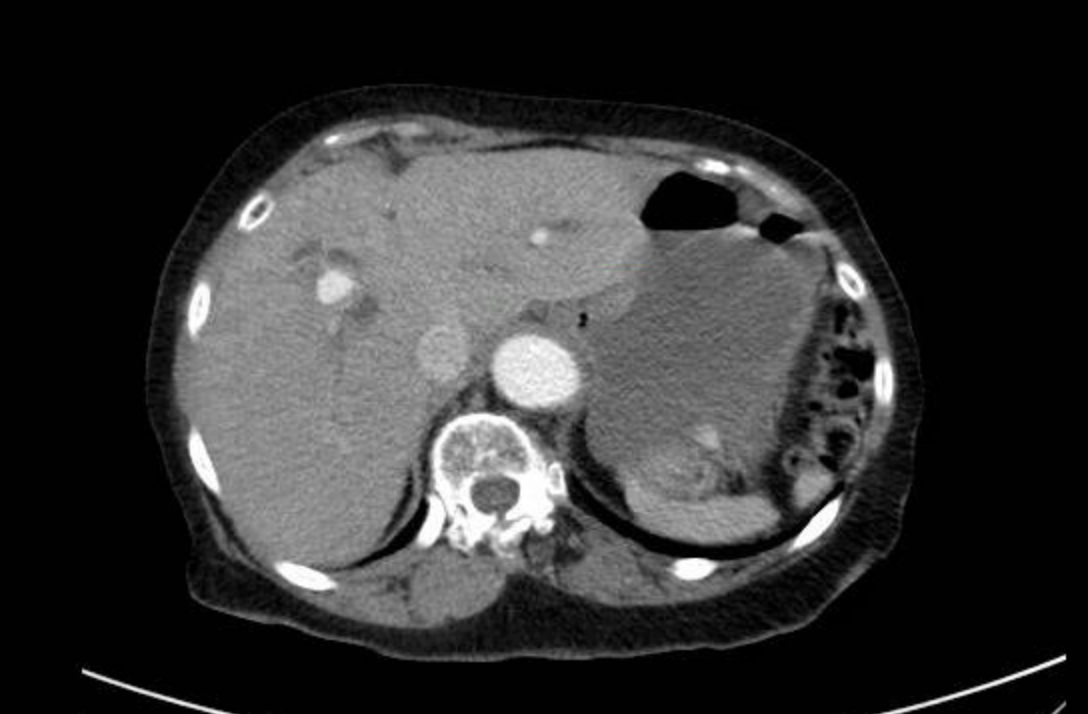
Figure: 6mm Hepatic artery pseudoaneurysm
Disclosures:
Susan Feldman indicated no relevant financial relationships.
Aidan Warner indicated no relevant financial relationships.
Gabriella Gee indicated no relevant financial relationships.
Susan Feldman, MD, Aidan Warner, MD, Gabriella Gee, BS. P2359 - An Unusual Cause of Biliary Obstruction: Hepatic Artery Pseudoaneurysm – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of South Carolina School of Medicine, Columbia, SC
Introduction: Hepatic artery pseudoaneurysms (HAPs) are rare vascular abnormalities that can present with life-threatening complications. While most HAPs occur secondary to hepatobiliary procedures or trauma, less common etiologies include malignancy and infection. A subset of HAPs can rupture into the biliary tract, resulting in hemobilia—a rare cause of upper gastrointestinal bleeding and obstructive jaundice. We present a case of HAP rupture resulting in hemobilia and biliary obstruction.
Case Description/
Methods: An 88-year-old woman with chronic lymphocytic leukemia (CLL) presented with melena and progressive jaundice. She had sustained a mechanical fall three days prior. Labs revealed anemia (Hgb 9.6), thrombocytopenia (Plt 27), leukocytosis (WBC 27.1), and a cholestatic liver injury pattern: AST 710, ALT 747, total bilirubin 8.9, direct bilirubin 6.7. ERCP revealed blood and sludge within the biliary tree; plastic stents were placed in the common bile duct and pancreatic duct. CT imaging showed an enhancing lesion concerning for a ruptured hepatic artery aneurysm. Interventional radiology confirmed a right hepatic artery pseudoaneurysm, which was successfully embolized with coils. Post-procedure, the patient developed worsening transaminitis and hyperbilirubinemia, consistent with hepatic ischemia. Despite supportive care, the patient was unable to recover.
Discussion: HAPs are exceedingly rare, comprising less than 20% of all visceral artery aneurysms, with rupture posing a high mortality risk. When ruptured into the biliary tract, they may cause "Quincke’s triad," described as jaundice, upper GI bleeding, and right upper quadrant pain. In this case, the patient’s CLL-associated thrombocytopenia likely exacerbated bleeding. Furthermore, embolization, while life-saving and necessary to this patient, carries its own risk for hepatic ischemia. This case highlights the need for considering vascular sources in atypical GI bleeds with cholestatic labs and highlights the rapid deterioration possible with HAP rupture. Timely diagnosis with cross-sectional imaging and prompt endovascular intervention remain essential to improve outcomes.
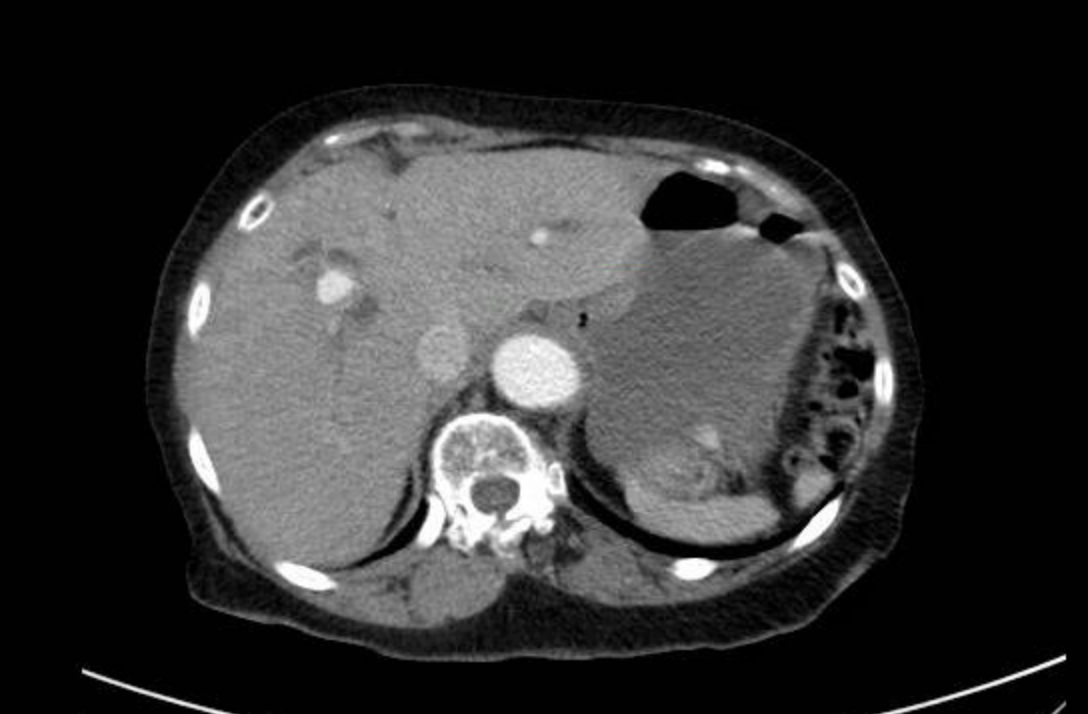
Figure: 6mm Hepatic artery pseudoaneurysm
Disclosures:
Susan Feldman indicated no relevant financial relationships.
Aidan Warner indicated no relevant financial relationships.
Gabriella Gee indicated no relevant financial relationships.
Susan Feldman, MD, Aidan Warner, MD, Gabriella Gee, BS. P2359 - An Unusual Cause of Biliary Obstruction: Hepatic Artery Pseudoaneurysm – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
