Monday Poster Session
Category: Biliary/Pancreas
P2348 - A Comparative Analysis of Rural and Urban Disparities in Acute Pancreatitis Outcomes: Insights From the National Inpatient Sample Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Evelyn Inga, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Evelyn Inga, MD1, Christopher Chang, MD, PhD2, Niloy Ghosh, MD1, Kara Eileen. Rieth, DO3, Mohammed Quazi, PhD3, Amir Sohail, MD, MSc4, Abu Baker Sheikh, MD1
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico School of Medicine, Albuquerque, NM; 3UNM, Albuquerque, NM; 4University of New Mexico, Albuquerque, NM
Introduction: The generic causes, algorithmic management, and treatments of acute pancreatitis (AP) are well-studied, but significant disparities between rural and urban population groups have yet to be researched. With this study, we aim to evaluate the differences in the outcomes of AP between rural and urban patients. The outcomes compared were in-hospital mortality (IHM), acute kidney injury (AKI), vasopressor use, invasive mechanical ventilation (IMV), non-invasive mechanical ventilation (NIMV), hemodialysis (HD), acute respiratory distress syndrome (ARDS), acute liver failure (ALF), necrotizing pancreatitis (NP), transfusion of packed red blood cell (pRBC), overall mean inflation adjusted cost in dollars ($) (IAC) and mean length of stay (LOS).
Case Description/
Methods: This retrospective cohort study utilized the National Inpatient Sample (NIS) database from 2016 to 2021, analyzing 1,549,845 adult patients diagnosed with AP, stratified by urban (n=1,289,970, 83.23%) and rural (n=259,875, 16.77%) geographic locations. We utilized a multivariable logistic and linear regression model adjusted for patient demographics, hospital demographics, hospital bed size, patient comorbidities and disposition to evaluate in-hospital outcomes. Outcomes analyzed were depicted as adjusted Odds ratio (OR) and the combined means.
Discussion: Rural patients demonstrated a significantly higher complication rate, OR for rural including: In-hospital mortality (OR 1.38, p-value < 0.001, CI 1.18-1.62), AKI (OR 1.06, p-value 0.016, CI 1.01-1.10), vasopressor use (OR 1.55, p-value < 0.001, CI 1.20-2.00), IMV (OR 1.46, p-value < 0.001, CI 1.32-1.62), NIMV (OR 1.37, p-value <0.001, CI 1.17-1.60), HD (OR 1.31, p-value < 0.001, CI 1.17-1.46), ARDS (OR 1.41, p-value 0.002, CI 1.14-1.74), ALF (OR 1.27, p-value 0.003, CI 1.08-1.49), NP (OR 1.61,p-value < 0.001, CI 1.48-1.76), transfusion of pRBC’s (OR 1.22, p-value 0.002, CI 1.08-1.39). However, mean LOS and mean IAC ($) were lower for rural vs urban patients, the overall mean IAC dollars (urban: $47,057.99 versus rural: $33,230.87), adjusted mean IAC = $11,343.80 lower for rural, p-value 0.005), mean LOS (urban 4.31 days versus rural 4.06 days, p-value < 0.001).
Rural populations with AP have worse outcomes compared to urban populations, but rural patients have a lower healthcare expenditure. Earlier transfer to higher levels of care and more healthcare dollar expenditure in rural health programs may improve care and outcomes for patients with AP.
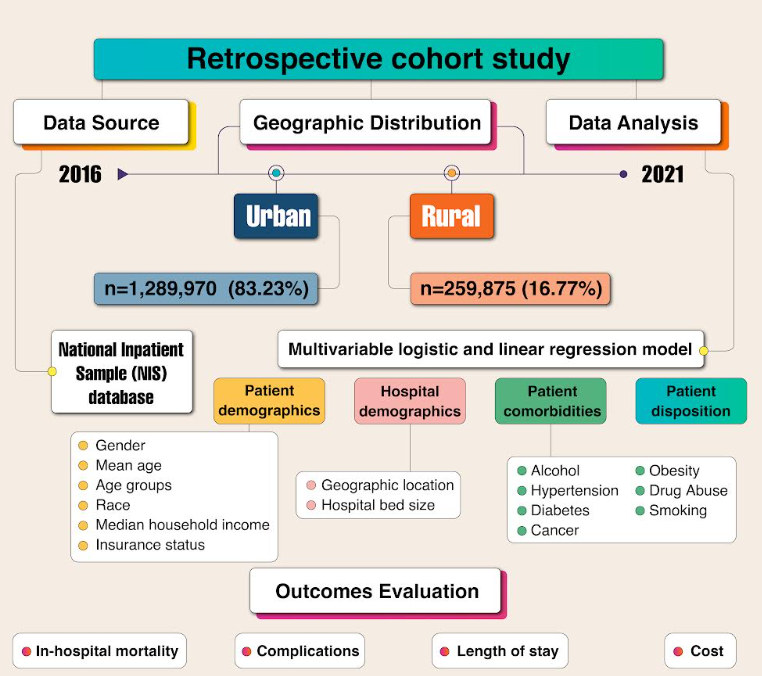
Figure: Pancreatitis Design of Study
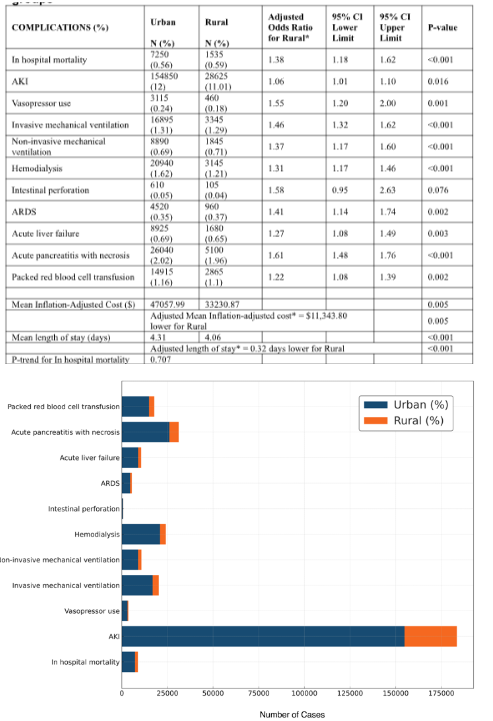
Figure: Complications and other outcomes stratified by the urban and the rural groups.
(Adjusted for Age, Hospital bed size, Race, Gender, Hospital region, Median Household Income, Expected primary payer [insurance status], and Elixhauser comorbidities.)
Complications in Acute Pancreatitis Patients (Urban vs Rural)
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Niloy Ghosh indicated no relevant financial relationships.
Kara Rieth indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Evelyn Inga, MD1, Christopher Chang, MD, PhD2, Niloy Ghosh, MD1, Kara Eileen. Rieth, DO3, Mohammed Quazi, PhD3, Amir Sohail, MD, MSc4, Abu Baker Sheikh, MD1. P2348 - A Comparative Analysis of Rural and Urban Disparities in Acute Pancreatitis Outcomes: Insights From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico School of Medicine, Albuquerque, NM; 3UNM, Albuquerque, NM; 4University of New Mexico, Albuquerque, NM
Introduction: The generic causes, algorithmic management, and treatments of acute pancreatitis (AP) are well-studied, but significant disparities between rural and urban population groups have yet to be researched. With this study, we aim to evaluate the differences in the outcomes of AP between rural and urban patients. The outcomes compared were in-hospital mortality (IHM), acute kidney injury (AKI), vasopressor use, invasive mechanical ventilation (IMV), non-invasive mechanical ventilation (NIMV), hemodialysis (HD), acute respiratory distress syndrome (ARDS), acute liver failure (ALF), necrotizing pancreatitis (NP), transfusion of packed red blood cell (pRBC), overall mean inflation adjusted cost in dollars ($) (IAC) and mean length of stay (LOS).
Case Description/
Methods: This retrospective cohort study utilized the National Inpatient Sample (NIS) database from 2016 to 2021, analyzing 1,549,845 adult patients diagnosed with AP, stratified by urban (n=1,289,970, 83.23%) and rural (n=259,875, 16.77%) geographic locations. We utilized a multivariable logistic and linear regression model adjusted for patient demographics, hospital demographics, hospital bed size, patient comorbidities and disposition to evaluate in-hospital outcomes. Outcomes analyzed were depicted as adjusted Odds ratio (OR) and the combined means.
Discussion: Rural patients demonstrated a significantly higher complication rate, OR for rural including: In-hospital mortality (OR 1.38, p-value < 0.001, CI 1.18-1.62), AKI (OR 1.06, p-value 0.016, CI 1.01-1.10), vasopressor use (OR 1.55, p-value < 0.001, CI 1.20-2.00), IMV (OR 1.46, p-value < 0.001, CI 1.32-1.62), NIMV (OR 1.37, p-value <0.001, CI 1.17-1.60), HD (OR 1.31, p-value < 0.001, CI 1.17-1.46), ARDS (OR 1.41, p-value 0.002, CI 1.14-1.74), ALF (OR 1.27, p-value 0.003, CI 1.08-1.49), NP (OR 1.61,p-value < 0.001, CI 1.48-1.76), transfusion of pRBC’s (OR 1.22, p-value 0.002, CI 1.08-1.39). However, mean LOS and mean IAC ($) were lower for rural vs urban patients, the overall mean IAC dollars (urban: $47,057.99 versus rural: $33,230.87), adjusted mean IAC = $11,343.80 lower for rural, p-value 0.005), mean LOS (urban 4.31 days versus rural 4.06 days, p-value < 0.001).
Rural populations with AP have worse outcomes compared to urban populations, but rural patients have a lower healthcare expenditure. Earlier transfer to higher levels of care and more healthcare dollar expenditure in rural health programs may improve care and outcomes for patients with AP.
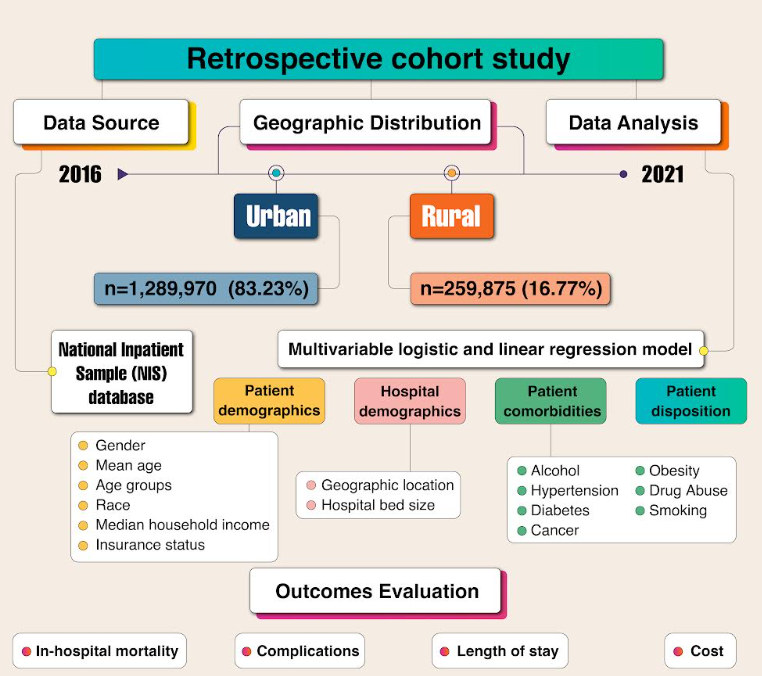
Figure: Pancreatitis Design of Study
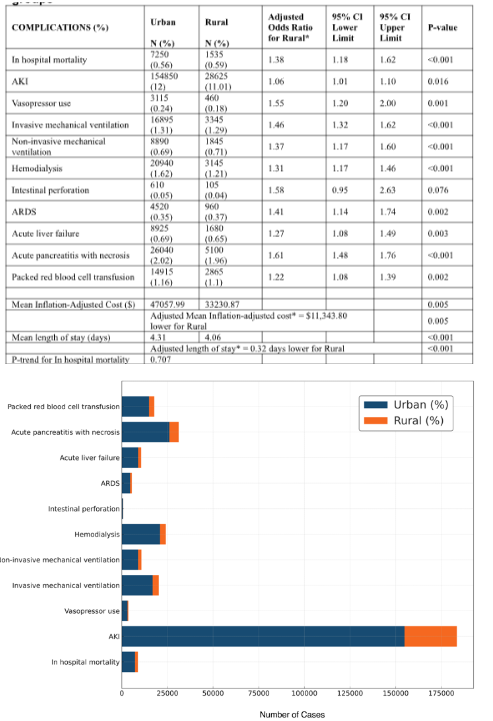
Figure: Complications and other outcomes stratified by the urban and the rural groups.
(Adjusted for Age, Hospital bed size, Race, Gender, Hospital region, Median Household Income, Expected primary payer [insurance status], and Elixhauser comorbidities.)
Complications in Acute Pancreatitis Patients (Urban vs Rural)
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Niloy Ghosh indicated no relevant financial relationships.
Kara Rieth indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Evelyn Inga, MD1, Christopher Chang, MD, PhD2, Niloy Ghosh, MD1, Kara Eileen. Rieth, DO3, Mohammed Quazi, PhD3, Amir Sohail, MD, MSc4, Abu Baker Sheikh, MD1. P2348 - A Comparative Analysis of Rural and Urban Disparities in Acute Pancreatitis Outcomes: Insights From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
