Monday Poster Session
Category: Biliary/Pancreas
P2340 - Giant Hemorrhagic Pancreatic Pseudocyst: A Rare and Dangerous Complication
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Erika Haviland, DO (she/her/hers)
Louisiana State University
New Orleans, LA
Presenting Author(s)
Erika Haviland, DO1, Kristen Williams, MD1, Hunter Hall, MD1, Stephen Landreneau, MD, FACG2
1Louisiana State University, New Orleans, LA; 2LSU Health Sciences Center New Orleans, New Orleans, LA
Introduction: Hemorrhage of a pancreatic pseudocyst is a rare complication of pancreatitis caused by erosion from the arterial wall opposing the pseudocyst, most commonly the splenic artery, and less commonly the gastric artery2. It is associated with a high mortality rate between 34-52% and requires emergent intervention1.
Case Description/
Methods: A 26-year-old male with a history of motor vehicle accident one year ago complicated by gastrostomy tube and necrotizing biliary pancreatitis with recent outpatient cholecystectomy, presented from outside hospital with abdominal pain, nausea, and non-bloody vomiting for 3 weeks. Computed Tomography (CT) of the abdomen showed increased size of a complicated intrapancreatic pseudocyst versus walled-off necrosis replacing the body and tail of the pancreas with a questionable hemorrhagic component but no discrete pseudoaneurysm was seen. There was displacement of the stomach with gastric edema and compromise of the portal system, with multiple engorged perigastric collaterals with interposition between the stomach wall. Patient became tachycardic to the 140s, febrile, and hypotensive. Initial hemoglobin of 10.0 gm/dL was repeated and found to be 6.8 gm/dL and mass transfusion protocol was initiated for suspected hemorrhagic shock. Interventional radiology successfully embolized the left gastric artery with gelfoam and coil embolization of the gastroduodenal artery. Later during his course, endoscopic ultrasound showed the 10 cm pancreatic collection with extrinsic compression on gastric body. A cystogastrostomy was performed with placement of a 10 French x 3cm double pigtail stent with a large interval decrease in the size of the cyst. Patient was subsequently discharge and returned two weeks later for removal of the stent without complication.
Discussion: This case highlights an emergent complication of pancreatitis, which while rare, bleeding caused by pancreatic pseudocysts is associated with high mortality and morbidity.2
1. Evans RP, Mourad MM, Pall G, Fisher SG, Bramhall SR. Pancreatitis: Preventing catastrophic haemorrhage. World J Gastroenterol 2017; 23(30): 5460-5468 [PMID: 28852306 DOI: 10.3748/wjg.v23.i30.5460]
2. Jain, S. K., Rajendran, V., Jain, M. K., & Kori, R. (2015). Hemorrhagic Pseudocyst of Pancreas Treated with Coil Embolization of Gastroduodenal Artery: A Case Report and Review of Literature. Case Reports in Surgery, 2015.https://doi.org/10.1155/2015/480605
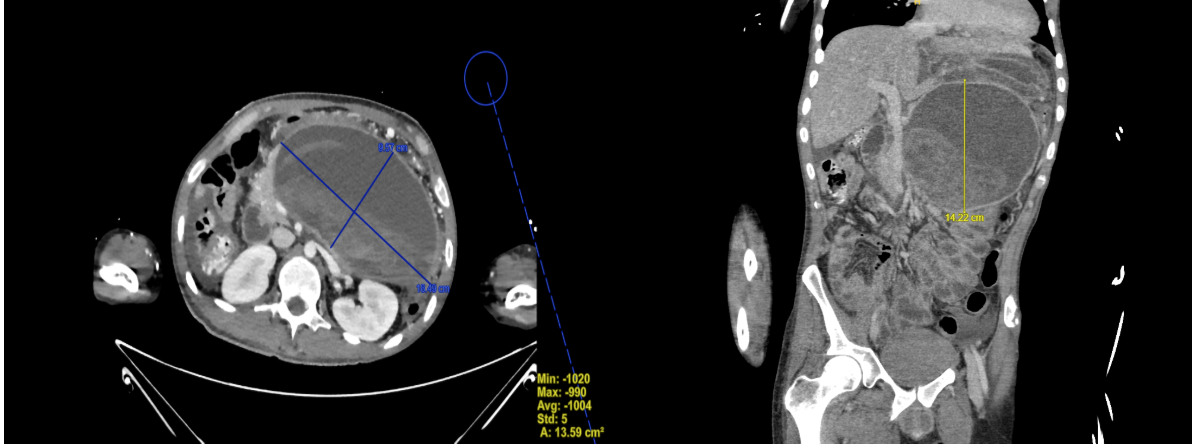
Figure: Large complex collection with well-defined wall replacing the pancreatic body and tail with high attenuation layering internal debris measuring 18.5 x 9.6 x 14 cm. There is compression of the splenic vein, which is patent.
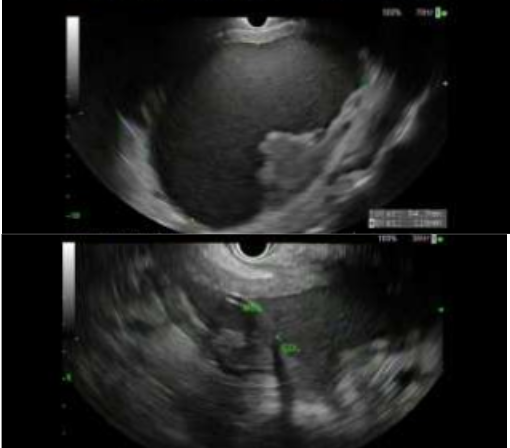
Figure: Cystic mass in the pancreatic body seen on endoscopic ultrasound before (above) and after (below) the lumen apposing metal stent (LAMS) was placed.
Disclosures:
Erika Haviland indicated no relevant financial relationships.
Kristen Williams indicated no relevant financial relationships.
Hunter Hall indicated no relevant financial relationships.
Stephen Landreneau indicated no relevant financial relationships.
Erika Haviland, DO1, Kristen Williams, MD1, Hunter Hall, MD1, Stephen Landreneau, MD, FACG2. P2340 - Giant Hemorrhagic Pancreatic Pseudocyst: A Rare and Dangerous Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University, New Orleans, LA; 2LSU Health Sciences Center New Orleans, New Orleans, LA
Introduction: Hemorrhage of a pancreatic pseudocyst is a rare complication of pancreatitis caused by erosion from the arterial wall opposing the pseudocyst, most commonly the splenic artery, and less commonly the gastric artery2. It is associated with a high mortality rate between 34-52% and requires emergent intervention1.
Case Description/
Methods: A 26-year-old male with a history of motor vehicle accident one year ago complicated by gastrostomy tube and necrotizing biliary pancreatitis with recent outpatient cholecystectomy, presented from outside hospital with abdominal pain, nausea, and non-bloody vomiting for 3 weeks. Computed Tomography (CT) of the abdomen showed increased size of a complicated intrapancreatic pseudocyst versus walled-off necrosis replacing the body and tail of the pancreas with a questionable hemorrhagic component but no discrete pseudoaneurysm was seen. There was displacement of the stomach with gastric edema and compromise of the portal system, with multiple engorged perigastric collaterals with interposition between the stomach wall. Patient became tachycardic to the 140s, febrile, and hypotensive. Initial hemoglobin of 10.0 gm/dL was repeated and found to be 6.8 gm/dL and mass transfusion protocol was initiated for suspected hemorrhagic shock. Interventional radiology successfully embolized the left gastric artery with gelfoam and coil embolization of the gastroduodenal artery. Later during his course, endoscopic ultrasound showed the 10 cm pancreatic collection with extrinsic compression on gastric body. A cystogastrostomy was performed with placement of a 10 French x 3cm double pigtail stent with a large interval decrease in the size of the cyst. Patient was subsequently discharge and returned two weeks later for removal of the stent without complication.
Discussion: This case highlights an emergent complication of pancreatitis, which while rare, bleeding caused by pancreatic pseudocysts is associated with high mortality and morbidity.2
1. Evans RP, Mourad MM, Pall G, Fisher SG, Bramhall SR. Pancreatitis: Preventing catastrophic haemorrhage. World J Gastroenterol 2017; 23(30): 5460-5468 [PMID: 28852306 DOI: 10.3748/wjg.v23.i30.5460]
2. Jain, S. K., Rajendran, V., Jain, M. K., & Kori, R. (2015). Hemorrhagic Pseudocyst of Pancreas Treated with Coil Embolization of Gastroduodenal Artery: A Case Report and Review of Literature. Case Reports in Surgery, 2015.https://doi.org/10.1155/2015/480605
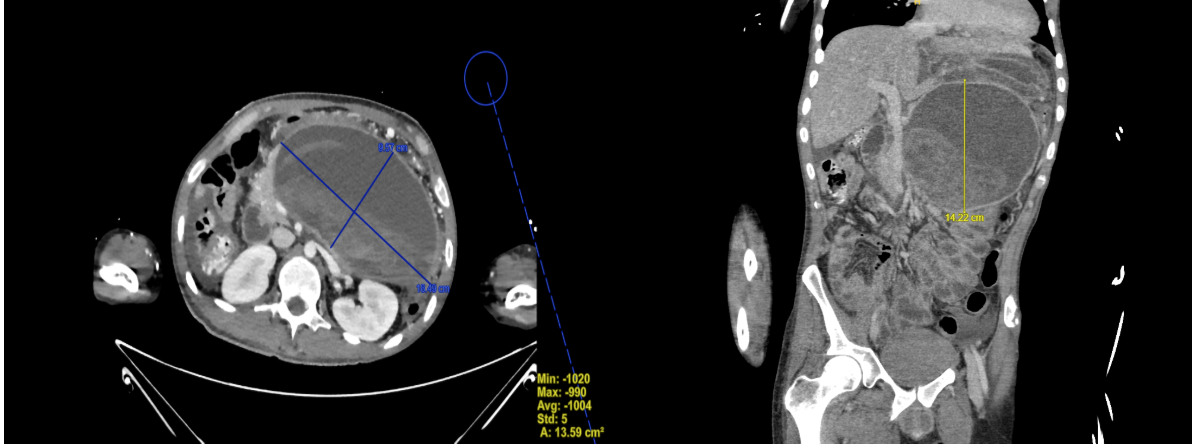
Figure: Large complex collection with well-defined wall replacing the pancreatic body and tail with high attenuation layering internal debris measuring 18.5 x 9.6 x 14 cm. There is compression of the splenic vein, which is patent.
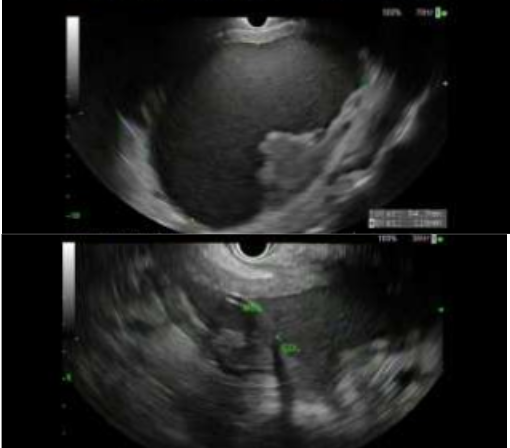
Figure: Cystic mass in the pancreatic body seen on endoscopic ultrasound before (above) and after (below) the lumen apposing metal stent (LAMS) was placed.
Disclosures:
Erika Haviland indicated no relevant financial relationships.
Kristen Williams indicated no relevant financial relationships.
Hunter Hall indicated no relevant financial relationships.
Stephen Landreneau indicated no relevant financial relationships.
Erika Haviland, DO1, Kristen Williams, MD1, Hunter Hall, MD1, Stephen Landreneau, MD, FACG2. P2340 - Giant Hemorrhagic Pancreatic Pseudocyst: A Rare and Dangerous Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
