Monday Poster Session
Category: Colon
P2460 - Inflammatory Indices as Markers of Diagnostic Accuracy for Distant Metastasis in Colorectal Cancer in a Resource-Limited Setting
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AF
Andre J. Fuentes Yufra, MD (he/him/his)
Universidad Privada de Tacna
Tacna, Tacna, Peru
Presenting Author(s)
Andre J.. Fuentes Yufra, MD1, Claudia P.. Pinto Narvaez, MD2, Allison N.. Ortiz Pardo, MD3, Jose M.. Vela Ruiz, MD4
1Universidad Privada de Tacna, Tacna, Tacna, Peru; 2Universidad Ricardo Palma, Lima, Lima, Peru; 3Peruvian American Medical Society, Lima, Lima, Peru; 4Universidad Ricardo Palma, Lima, Lima, Lima, Peru
Introduction: Colorectal cancer (CRC) is the third most common malignancy worldwide and the second leading cause of cancer-related mortality. Its incidence has shown a significant increase in developing regions. Approximately 70% of cases are diagnosed at advanced stages, and 20% present with distant metastases at diagnosis. Therefore, early detection is critical; however, in low- and middle-income countries, the availability of advanced diagnostic tools is limited due to high costs. Thus, the objective of this study was to evaluate the diagnostic accuracy of the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) for detecting distant metastases in CRC patients.
Methods: An observational, analytical, and cross-sectional study was conducted, including all CRC patients over 18 years of age treated at María Auxiliadora Hospital (Lima, Peru) from 2016 to 2020. Patients with autoimmune or infectious diseases were excluded.
Diagnostic accuracy was assessed using the receiver operating characteristic (ROC) curve and the area under the ROC curve (AUROC), with 95% confidence intervals and optimal cut-off points determined by the Youden index.
Results: Of the 116 CRC patients, 19 were excluded due to incomplete medical records. Of the remaining, 51.55% were male and 20% were older than 70 years. Distant metastases were present in 19.6% of cases.
The optimal NLR cut-off was 3.55, yielding a sensitivity of 57.9%, specificity of 66.7%, positive predictive value (PPV) of 29.7%, negative predictive value (NPV) of 86.7%, and AUROC of 0.62 (95% CI: 0.50–0.75).
For PLR, the cut-off was 192, with a sensitivity of 84.2%, specificity of 50%, PPV of 29.1%, NPV of 92.9%, and AUROC of 0.67 (95% CI: 0.57–0.77).
CEA ≥5 ng/ml showed a sensitivity of 78.9% and specificity of 52.6%, with AUROC of 0.66 (95% CI: 0.55–0.77), while serum albumin < 3.5 g/dL had an AUROC of 0.75 (95% CI: 0.67–0.82), with sensitivity of 94.7% (95% CI: 74–99.9) and specificity of 55.1% (95% CI: 43.4–66.4).
Discussion: A prevalence of 19.6% of CRC with distant metastasis was found. PLR and serum albumin stood out for their high sensitivity and NPV, highlighting their potential as accessible and low-cost markers for use in resource-limited settings.
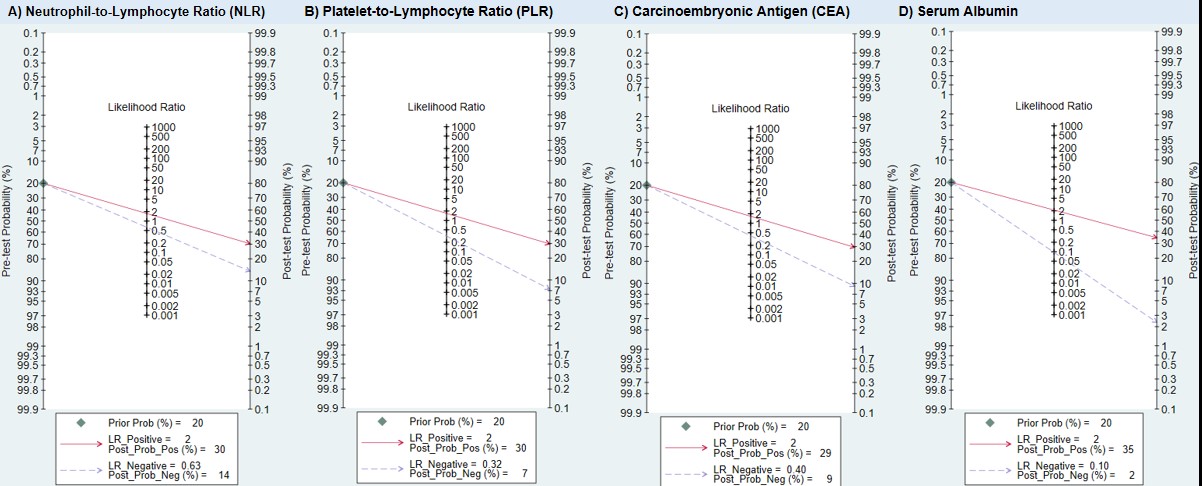
Figure: Figure 1: ROC curves for the detection of distant metastases in colorectal cancer patients based on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, carcinoembryonic antigen, and serum albumin
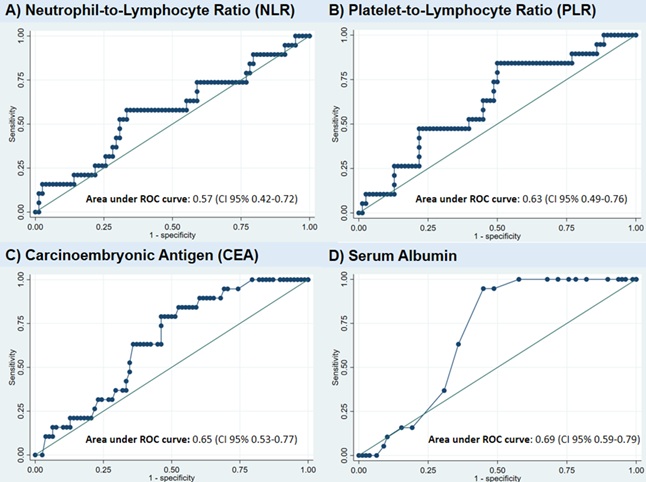
Figure: Figure 2: Fagan nomograms for the evaluation of post-test probability of distant metastases in colorectal cancer patients based on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, carcinoembryonic antigen, and serum albumin
Disclosures:
Andre Fuentes Yufra indicated no relevant financial relationships.
Claudia Pinto Narvaez indicated no relevant financial relationships.
Allison Ortiz Pardo indicated no relevant financial relationships.
Jose Vela Ruiz indicated no relevant financial relationships.
Andre J.. Fuentes Yufra, MD1, Claudia P.. Pinto Narvaez, MD2, Allison N.. Ortiz Pardo, MD3, Jose M.. Vela Ruiz, MD4. P2460 - Inflammatory Indices as Markers of Diagnostic Accuracy for Distant Metastasis in Colorectal Cancer in a Resource-Limited Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Universidad Privada de Tacna, Tacna, Tacna, Peru; 2Universidad Ricardo Palma, Lima, Lima, Peru; 3Peruvian American Medical Society, Lima, Lima, Peru; 4Universidad Ricardo Palma, Lima, Lima, Lima, Peru
Introduction: Colorectal cancer (CRC) is the third most common malignancy worldwide and the second leading cause of cancer-related mortality. Its incidence has shown a significant increase in developing regions. Approximately 70% of cases are diagnosed at advanced stages, and 20% present with distant metastases at diagnosis. Therefore, early detection is critical; however, in low- and middle-income countries, the availability of advanced diagnostic tools is limited due to high costs. Thus, the objective of this study was to evaluate the diagnostic accuracy of the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) for detecting distant metastases in CRC patients.
Methods: An observational, analytical, and cross-sectional study was conducted, including all CRC patients over 18 years of age treated at María Auxiliadora Hospital (Lima, Peru) from 2016 to 2020. Patients with autoimmune or infectious diseases were excluded.
Diagnostic accuracy was assessed using the receiver operating characteristic (ROC) curve and the area under the ROC curve (AUROC), with 95% confidence intervals and optimal cut-off points determined by the Youden index.
Results: Of the 116 CRC patients, 19 were excluded due to incomplete medical records. Of the remaining, 51.55% were male and 20% were older than 70 years. Distant metastases were present in 19.6% of cases.
The optimal NLR cut-off was 3.55, yielding a sensitivity of 57.9%, specificity of 66.7%, positive predictive value (PPV) of 29.7%, negative predictive value (NPV) of 86.7%, and AUROC of 0.62 (95% CI: 0.50–0.75).
For PLR, the cut-off was 192, with a sensitivity of 84.2%, specificity of 50%, PPV of 29.1%, NPV of 92.9%, and AUROC of 0.67 (95% CI: 0.57–0.77).
CEA ≥5 ng/ml showed a sensitivity of 78.9% and specificity of 52.6%, with AUROC of 0.66 (95% CI: 0.55–0.77), while serum albumin < 3.5 g/dL had an AUROC of 0.75 (95% CI: 0.67–0.82), with sensitivity of 94.7% (95% CI: 74–99.9) and specificity of 55.1% (95% CI: 43.4–66.4).
Discussion: A prevalence of 19.6% of CRC with distant metastasis was found. PLR and serum albumin stood out for their high sensitivity and NPV, highlighting their potential as accessible and low-cost markers for use in resource-limited settings.
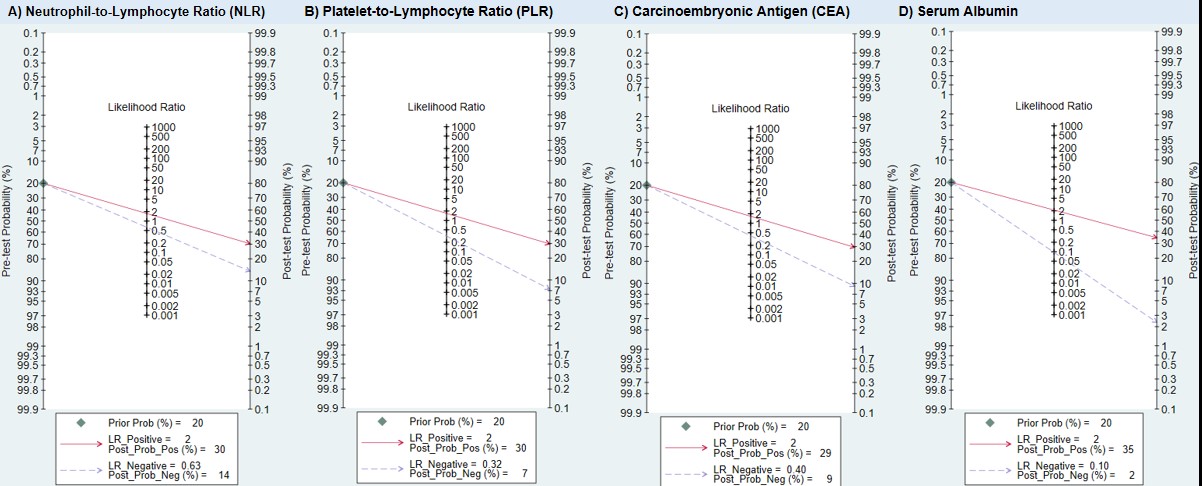
Figure: Figure 1: ROC curves for the detection of distant metastases in colorectal cancer patients based on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, carcinoembryonic antigen, and serum albumin
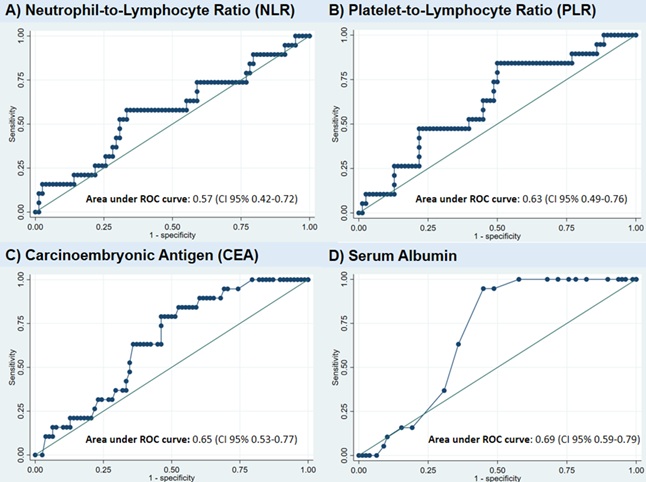
Figure: Figure 2: Fagan nomograms for the evaluation of post-test probability of distant metastases in colorectal cancer patients based on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, carcinoembryonic antigen, and serum albumin
Disclosures:
Andre Fuentes Yufra indicated no relevant financial relationships.
Claudia Pinto Narvaez indicated no relevant financial relationships.
Allison Ortiz Pardo indicated no relevant financial relationships.
Jose Vela Ruiz indicated no relevant financial relationships.
Andre J.. Fuentes Yufra, MD1, Claudia P.. Pinto Narvaez, MD2, Allison N.. Ortiz Pardo, MD3, Jose M.. Vela Ruiz, MD4. P2460 - Inflammatory Indices as Markers of Diagnostic Accuracy for Distant Metastasis in Colorectal Cancer in a Resource-Limited Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
