Monday Poster Session
Category: Colon
P2556 - Hidden in the Vein: A Rare Culprit of Refractory Colitis
- AV
Ananya Venkatesh, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 3Thomas Jefferson University Hospital (Philadelphia, PA), Philadelphia, PA
Introduction: Idiopathic Myointimal Hyperplasia of the Mesenteric Veins (IMHMV) is a rare and underrecognized cause of ischemic colitis characterized by smooth muscle proliferation within the intima and media of small to medium sized mesenteric veins. Clinically, IMHMV often mimics inflammatory bowel disease (IBD) or more common etiologies of ischemic colitis, rendering diagnosis particularly challenging. We present a case of IMHMV in a 70-year-old male who presented with abdominal pain.
Case Description/
Methods:
A 70-year-old male presented with three weeks of abdominal pain, tenesmus, and hematochezia. Physical examination revealed periumbilical tenderness with guarding. Laboratory studies demonstrated an ESR 21 mm/hr, CRP 62.9 mg/L, and fecal calprotectin 503 µg/g. Complete blood count, rheumatologic panel, and infectious stool studies were unremarkable. Contrast-enhanced CT showed bowel wall thickening from the distal descending colon to the rectum with pericolonic fat stranding. He was initially managed with antibiotics and bowel rest.
Subsequent CT angiography demonstrated patent mesenteric arteries but notable ectasia and tortuosity of several inferior mesenteric artery branches. Colonoscopy showed mucosal edema, erythema, and ulcerations from the rectum to the descending colon. Intravenous methylprednisolone was initiated for a presumed diagnosis of IBD. However, histopathology revealed colonic mucosa with severe ischemic injury and necrosis, with features suggestive of IMHMV (Figure 1). Due to clinical deterioration despite maximal medical therapy, the patient underwent sigmoid colectomy. The resected specimen demonstrated cardinal features of IMHMV such as marked thickening of the mesenteric veins with associated luminal narrowing. (Figure 2).
Discussion: IMHMV is a rare, non-thrombotic, non-inflammatory vascular disorder causing ischemic colitis. Its clinical presentation and diagnostic imaging often overlap with IBD, infectious colitis, and other ischemic colitis variants, frequently leading to misdiagnosis. Importantly, there are no effective medical therapies for IMHMV; surgical resection of the affected bowel remains the definitive treatment. Delays in diagnosis and intervention increase the risk of serious complications such as bowel necrosis and perforation. This case highlights the need to consider IMHMV in patients with colitis who fail to respond to conventional medical therapies. Early recognition and timely surgical management are paramount to improving clinical outcomes.
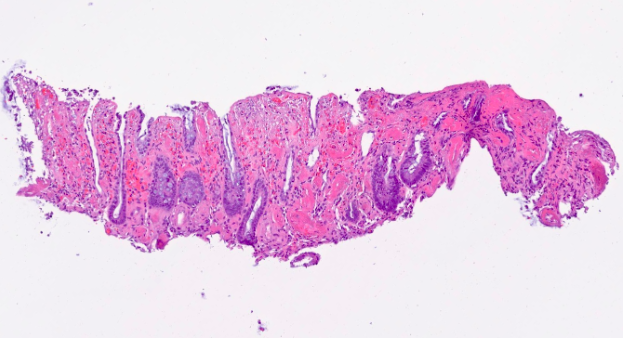
Figure: Figure 1: The biopsy showed ischemic pattern of injury characterized by surface epithelial damage with ulcers, withering crypts, and prominent capillary thrombi
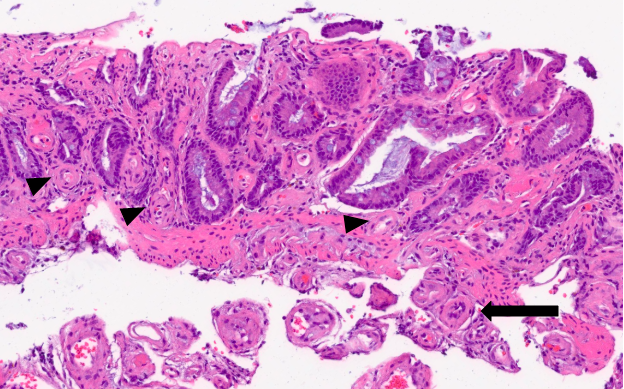
Figure: Figure 2: The mucosal capillaries (arrowhead) and small submucosal veins (arrow) are abnormally thickened (‘arteriolized’).
Disclosures:
Ananya Venkatesh indicated no relevant financial relationships.
Dustin Sneed indicated no relevant financial relationships.
Drake Kienzle indicated no relevant financial relationships.
Nikita Chaubal indicated no relevant financial relationships.
Anna Chen indicated no relevant financial relationships.
Maria Mostyka indicated no relevant financial relationships.
Cuckoo Choudhary indicated no relevant financial relationships.
Ananya Venkatesh, MD1, Dustin Sneed, MD1, Drake Kienzle, BA2, Nikita Chaubal, BS2, Anna Chen, MD1, Maria Mostyka, DO1, Cuckoo Choudhary, MD3. P2556 - Hidden in the Vein: A Rare Culprit of Refractory Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
