Monday Poster Session
Category: Colon
P2536 - Emerging Gastrointestinal Risks of GLP-1 Receptor Agonists: A Case of Ischemic Colitis in a Young Woman on Semaglutide
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NM
Nancy Mayer, DO
Riverside Medical Center
Bourbonnais, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Nancy Mayer, DO1, Matthew Sutherland, DO1, Suchitra Muralidharan, MB, BS2, Dhaval Patel, DO3
1Riverside Medical Center, Bourbonnais, IL; 2Riverside Medical Center, Kankakee, IL; 3Digestive Disease Consultants, Kankakee, IL
Introduction: With the increasing use of GLP-1 receptor agonists for weight loss and glycemic control, rare adverse effects are emerging. We present a case of ischemic colitis in a young woman with no significant comorbidities, raising concern for a potential drug-related complication.
Case Description/
Methods: A 37-year-old woman with obesity on semaglutide presented with two days of intractable left-sided abdominal pain, constipation, nausea, and vomiting. Labs showed leukocytosis (WBC 14,300/mm3), and CT imaging demonstrated mild colonic wall thickening with adjacent stranding at the splenic flexure. She denied sick contacts, travel, dietary changes, or new medications. Her last semaglutide dose was three days prior. Workup, including C. difficile, norovirus, rotavirus, and fecal calprotectin, was negative. Colonoscopy revealed mild erythema in the transverse colon and cobblestoning with white exudate in the left colon. Her symptoms improved with supportive care, and she was discharged. However, she returned three days later with recurrent abdominal pain. Histopathology of the transverse and left colon confirmed acute-on-chronic ischemic colitis. CT angiography abdomen/pelvis showed no evidence of reduced perfusion, stenosis, or vascular abnormalities. Autoimmune workup for vasculitis (ANA, ANCA, C3/C4) was negative. Semaglutide was discontinued, and symptoms gradually resolved. In the absence of comorbidities or identifiable risk factors, semaglutide-induced ischemic colitis appears the likely etiology.
Discussion: Ischemic colitis typically affects older adults with comorbidities such as atherosclerosis, chronic kidney disease, and diabetes mellitus. Our patient, a 37-year-old woman with no such risk factors, presented with biopsy-confirmed ischemic colitis. Notably, the only identifiable risk factor was the use of semaglutide, a GLP-1 receptor agonist. The mechanism by which GLP-1 receptor agonists may lead to ischemic colitis remains unclear. Proposed mechanisms include delayed colonic transit leading to increased intraluminal pressure and reduced mucosal perfusion, hypotension from decreased intake and vomiting, and direct effects on vascular tone. While ischemic colitis is not a widely recognized adverse effect of GLP-1 receptor agonists, a growing number of case reports, currently five in literature, have proposed a potential link. With rising use of GLP-1 receptor agonists in younger, low-risk patients, clinicians should maintain a high index of suspicion for medication-associated ischemic colitis.
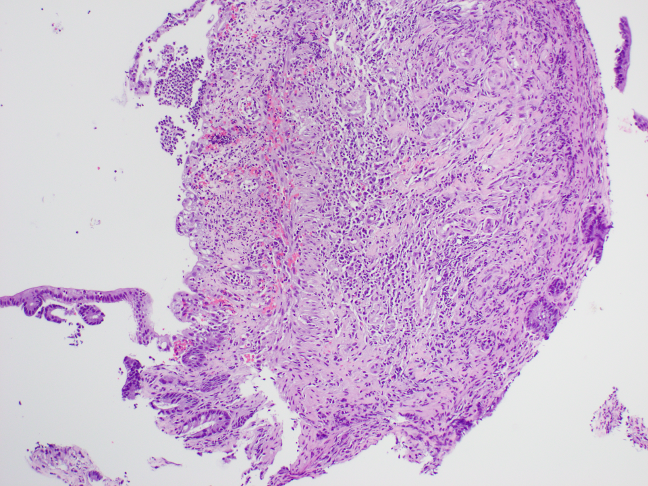
Figure: White exudate and cobblestone appearance of mucosa of the left colon consistent with ischemic colitis
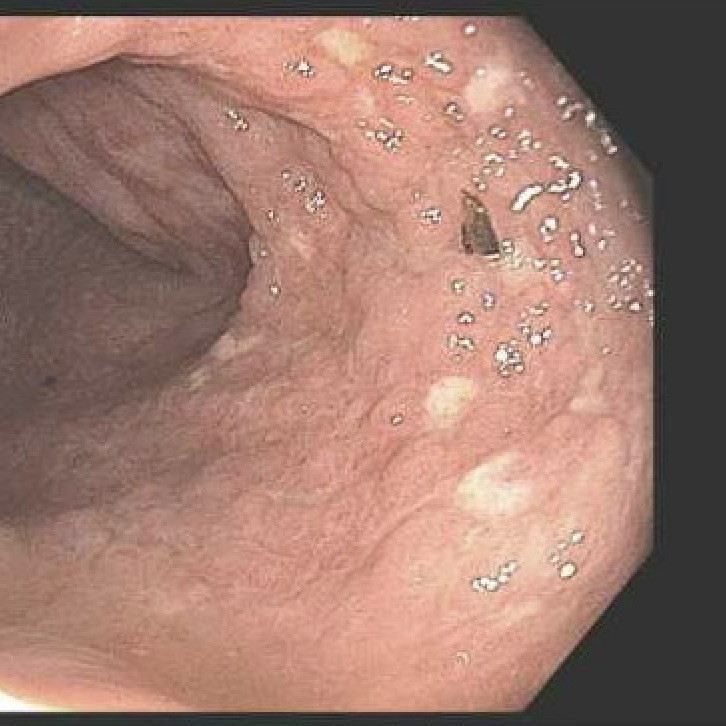
Figure: Colonic mucosa showing ulceration, withering crypts, crypt dropout, and lamina propria and submucosal hyalinization consistent with ischemic colitis (10X)
Disclosures:
Nancy Mayer indicated no relevant financial relationships.
Matthew Sutherland indicated no relevant financial relationships.
Suchitra Muralidharan indicated no relevant financial relationships.
Dhaval Patel indicated no relevant financial relationships.
Nancy Mayer, DO1, Matthew Sutherland, DO1, Suchitra Muralidharan, MB, BS2, Dhaval Patel, DO3. P2536 - Emerging Gastrointestinal Risks of GLP-1 Receptor Agonists: A Case of Ischemic Colitis in a Young Woman on Semaglutide, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Nancy Mayer, DO1, Matthew Sutherland, DO1, Suchitra Muralidharan, MB, BS2, Dhaval Patel, DO3
1Riverside Medical Center, Bourbonnais, IL; 2Riverside Medical Center, Kankakee, IL; 3Digestive Disease Consultants, Kankakee, IL
Introduction: With the increasing use of GLP-1 receptor agonists for weight loss and glycemic control, rare adverse effects are emerging. We present a case of ischemic colitis in a young woman with no significant comorbidities, raising concern for a potential drug-related complication.
Case Description/
Methods: A 37-year-old woman with obesity on semaglutide presented with two days of intractable left-sided abdominal pain, constipation, nausea, and vomiting. Labs showed leukocytosis (WBC 14,300/mm3), and CT imaging demonstrated mild colonic wall thickening with adjacent stranding at the splenic flexure. She denied sick contacts, travel, dietary changes, or new medications. Her last semaglutide dose was three days prior. Workup, including C. difficile, norovirus, rotavirus, and fecal calprotectin, was negative. Colonoscopy revealed mild erythema in the transverse colon and cobblestoning with white exudate in the left colon. Her symptoms improved with supportive care, and she was discharged. However, she returned three days later with recurrent abdominal pain. Histopathology of the transverse and left colon confirmed acute-on-chronic ischemic colitis. CT angiography abdomen/pelvis showed no evidence of reduced perfusion, stenosis, or vascular abnormalities. Autoimmune workup for vasculitis (ANA, ANCA, C3/C4) was negative. Semaglutide was discontinued, and symptoms gradually resolved. In the absence of comorbidities or identifiable risk factors, semaglutide-induced ischemic colitis appears the likely etiology.
Discussion: Ischemic colitis typically affects older adults with comorbidities such as atherosclerosis, chronic kidney disease, and diabetes mellitus. Our patient, a 37-year-old woman with no such risk factors, presented with biopsy-confirmed ischemic colitis. Notably, the only identifiable risk factor was the use of semaglutide, a GLP-1 receptor agonist. The mechanism by which GLP-1 receptor agonists may lead to ischemic colitis remains unclear. Proposed mechanisms include delayed colonic transit leading to increased intraluminal pressure and reduced mucosal perfusion, hypotension from decreased intake and vomiting, and direct effects on vascular tone. While ischemic colitis is not a widely recognized adverse effect of GLP-1 receptor agonists, a growing number of case reports, currently five in literature, have proposed a potential link. With rising use of GLP-1 receptor agonists in younger, low-risk patients, clinicians should maintain a high index of suspicion for medication-associated ischemic colitis.
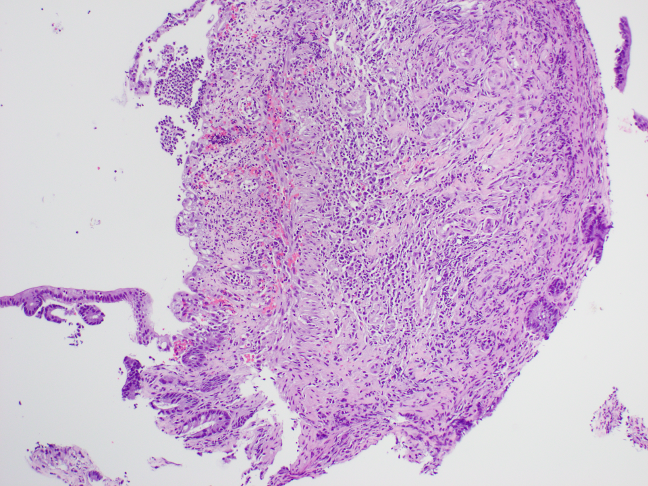
Figure: White exudate and cobblestone appearance of mucosa of the left colon consistent with ischemic colitis
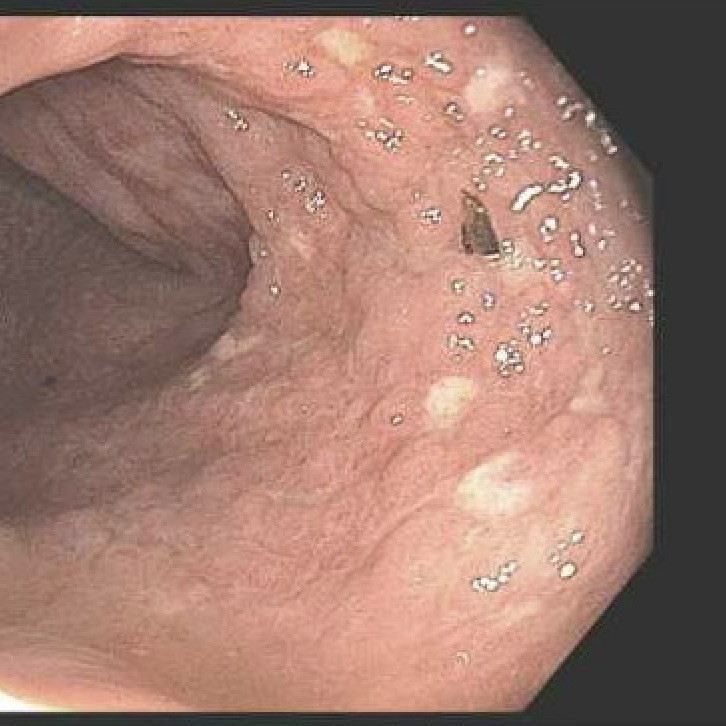
Figure: Colonic mucosa showing ulceration, withering crypts, crypt dropout, and lamina propria and submucosal hyalinization consistent with ischemic colitis (10X)
Disclosures:
Nancy Mayer indicated no relevant financial relationships.
Matthew Sutherland indicated no relevant financial relationships.
Suchitra Muralidharan indicated no relevant financial relationships.
Dhaval Patel indicated no relevant financial relationships.
Nancy Mayer, DO1, Matthew Sutherland, DO1, Suchitra Muralidharan, MB, BS2, Dhaval Patel, DO3. P2536 - Emerging Gastrointestinal Risks of GLP-1 Receptor Agonists: A Case of Ischemic Colitis in a Young Woman on Semaglutide, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


