Monday Poster Session
Category: Colorectal Cancer Prevention
P2611 - Colorectal Cancer Screening Trends and Disparities Across Demographics After USPSTF Guideline Updates and COVID-19 Disruptions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amer Arman, MD
MedStar Health
Detroit, MI
Presenting Author(s)
Omar Arman, MD, MPH1, Zeid Jarrar, MD2, Amer Arman, MD3, Blake Podger, MD1, Hebah Jaber, MD4, Mazen Zamzam, BS5, Osama Alshakhatreh, MD6, Jad Bou-Abdallah, MD1
1University at Buffalo, Buffalo, NY; 2University of Jordan School of Medicine, Amman, 'Amman, Jordan; 3MedStar Health, Washington, WA; 4Mutah University, Mutah, Al Karak, Jordan; 5Oakland University William Beaumont School of Medicine, Royal Oak, MI; 6Albany Medical Center, Albany, NY
Introduction: This study was designed to assess real-world colorectal cancer (CRC) screening trends during a period of evolving national focus on preventive care. In 2021, the United States Preventive Services Task Force (USPSTF) lowered the recommended CRC screening age from 50 to 45 years. While this guideline update directly expanded eligibility for younger adults, it also contributed to increased public attention and healthcare system emphasis on CRC screening overall. Since this period overlapped with the COVID-19 pandemic and persistent demographic disparities, we evaluated screening patterns from 2015 to 2023 across three distinct timeframes (pre-pandemic, pandemic onset, post-pandemic recovery), focusing on variation by race, ethnicity, sex, and age in adults aged 50–75.
Methods: We conducted a retrospective cohort study using the TriNetX database, including patients aged 50–75 without a prior CRC diagnosis. Screening was identified using CPT codes for colonoscopy, sigmoidoscopy, and fecal occult blood testing. Patients were grouped into three time periods: pre-pandemic (2015–2017), pandemic-impacted (2018–2020), and post-pandemic (2021–2023). Screening rates were assessed annually and stratified by demographic variables.
Results: Screening incidence peaked at 1.08% in 2019 but dropped by 22% to 0.84% in 2020. Although rates rebounded to 0.99% by 2023, they remained below pre-pandemic levels, despite increased national focus on CRC screening during this period. Demographic disparities persisted: Black patients showed slower recovery (1.25% in 2023 vs. 1.65% in 2019), while Hispanic patients exceeded pre-pandemic levels by 33%. Asian and American Indian/Alaskan Native populations experienced the steepest declines, with rates remaining below pre-pandemic levels through 2023.
Discussion: CRC screening trends from 2015 to 2023 reflect complex recovery patterns shaped by both the COVID-19 pandemic and increased national emphasis on screening following the USPSTF guideline update. Demographic disparities persisted, with incomplete recovery among Black patients and older adults, while Hispanic populations exceeded pre-pandemic screening levels. These findings highlight the need for adaptive, equity-focused screening strategies as healthcare systems continue to rebuild preventive care delivery.
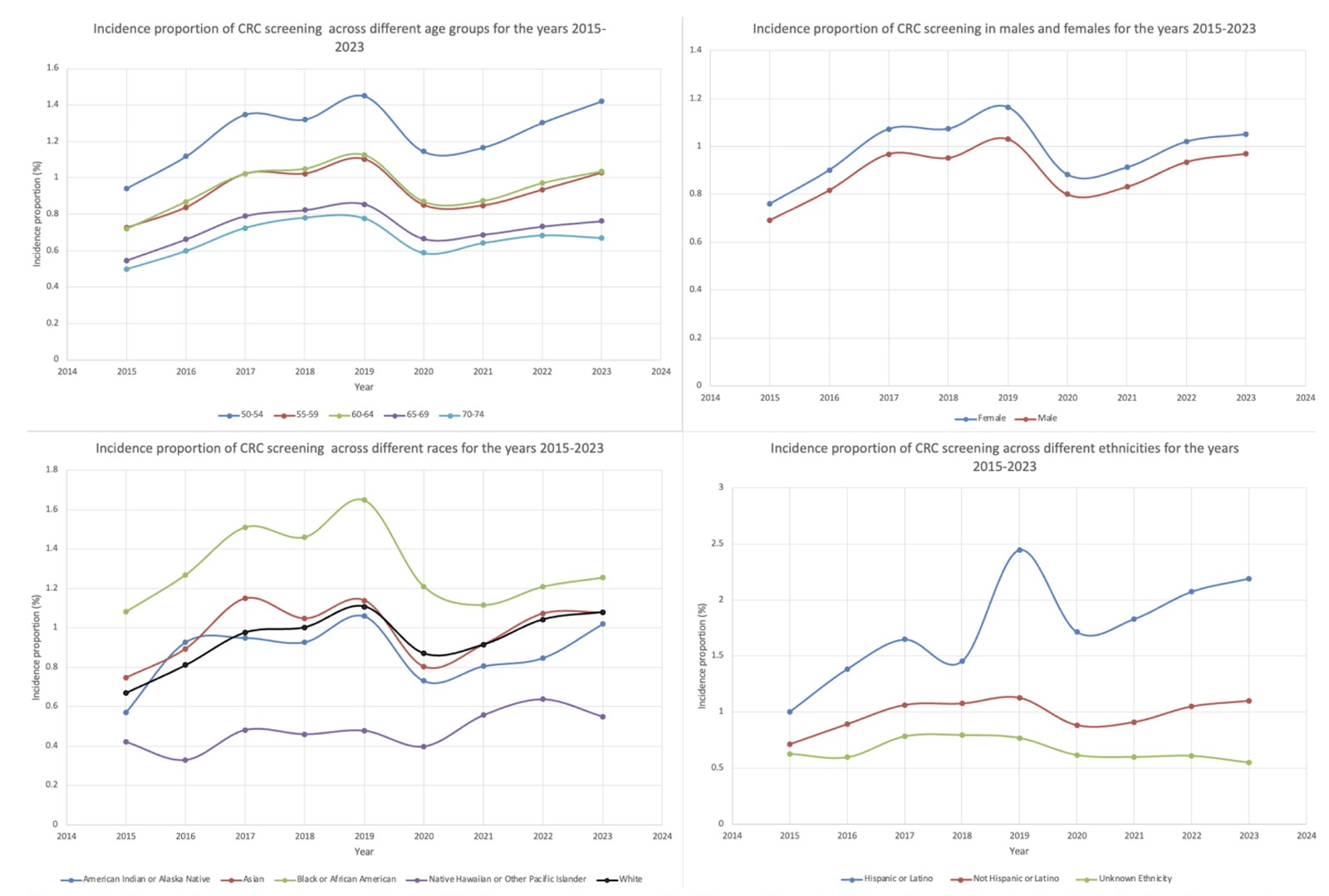
Figure: Figure 1: Incidence of CRC screening for the years 2015-2023
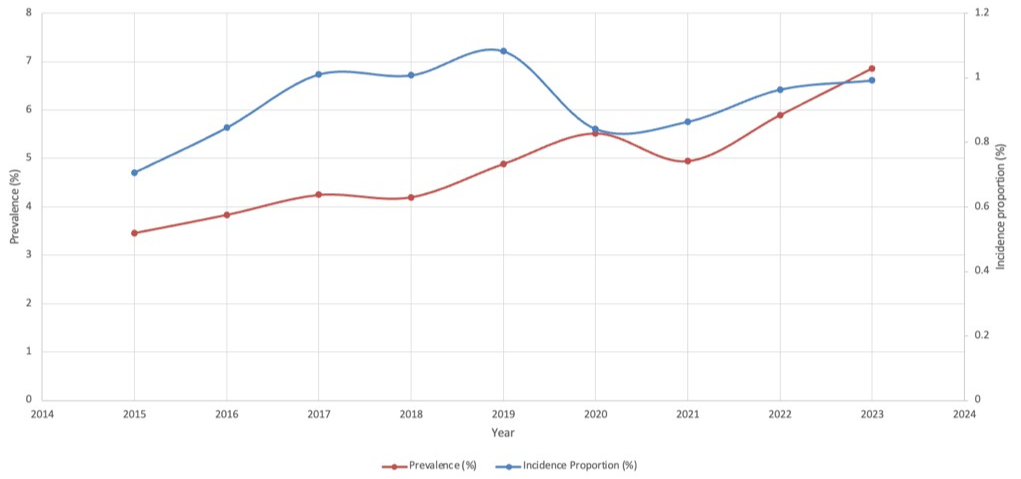
Figure: Figure 2: Incidence proportion of CRC screening stratified based on age, gender, race, and ethnicity for the years 2015-2023
Disclosures:
Omar Arman indicated no relevant financial relationships.
Zeid Jarrar indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Hebah Jaber indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Zeid Jarrar, MD2, Amer Arman, MD3, Blake Podger, MD1, Hebah Jaber, MD4, Mazen Zamzam, BS5, Osama Alshakhatreh, MD6, Jad Bou-Abdallah, MD1. P2611 - Colorectal Cancer Screening Trends and Disparities Across Demographics After USPSTF Guideline Updates and COVID-19 Disruptions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2University of Jordan School of Medicine, Amman, 'Amman, Jordan; 3MedStar Health, Washington, WA; 4Mutah University, Mutah, Al Karak, Jordan; 5Oakland University William Beaumont School of Medicine, Royal Oak, MI; 6Albany Medical Center, Albany, NY
Introduction: This study was designed to assess real-world colorectal cancer (CRC) screening trends during a period of evolving national focus on preventive care. In 2021, the United States Preventive Services Task Force (USPSTF) lowered the recommended CRC screening age from 50 to 45 years. While this guideline update directly expanded eligibility for younger adults, it also contributed to increased public attention and healthcare system emphasis on CRC screening overall. Since this period overlapped with the COVID-19 pandemic and persistent demographic disparities, we evaluated screening patterns from 2015 to 2023 across three distinct timeframes (pre-pandemic, pandemic onset, post-pandemic recovery), focusing on variation by race, ethnicity, sex, and age in adults aged 50–75.
Methods: We conducted a retrospective cohort study using the TriNetX database, including patients aged 50–75 without a prior CRC diagnosis. Screening was identified using CPT codes for colonoscopy, sigmoidoscopy, and fecal occult blood testing. Patients were grouped into three time periods: pre-pandemic (2015–2017), pandemic-impacted (2018–2020), and post-pandemic (2021–2023). Screening rates were assessed annually and stratified by demographic variables.
Results: Screening incidence peaked at 1.08% in 2019 but dropped by 22% to 0.84% in 2020. Although rates rebounded to 0.99% by 2023, they remained below pre-pandemic levels, despite increased national focus on CRC screening during this period. Demographic disparities persisted: Black patients showed slower recovery (1.25% in 2023 vs. 1.65% in 2019), while Hispanic patients exceeded pre-pandemic levels by 33%. Asian and American Indian/Alaskan Native populations experienced the steepest declines, with rates remaining below pre-pandemic levels through 2023.
Discussion: CRC screening trends from 2015 to 2023 reflect complex recovery patterns shaped by both the COVID-19 pandemic and increased national emphasis on screening following the USPSTF guideline update. Demographic disparities persisted, with incomplete recovery among Black patients and older adults, while Hispanic populations exceeded pre-pandemic screening levels. These findings highlight the need for adaptive, equity-focused screening strategies as healthcare systems continue to rebuild preventive care delivery.
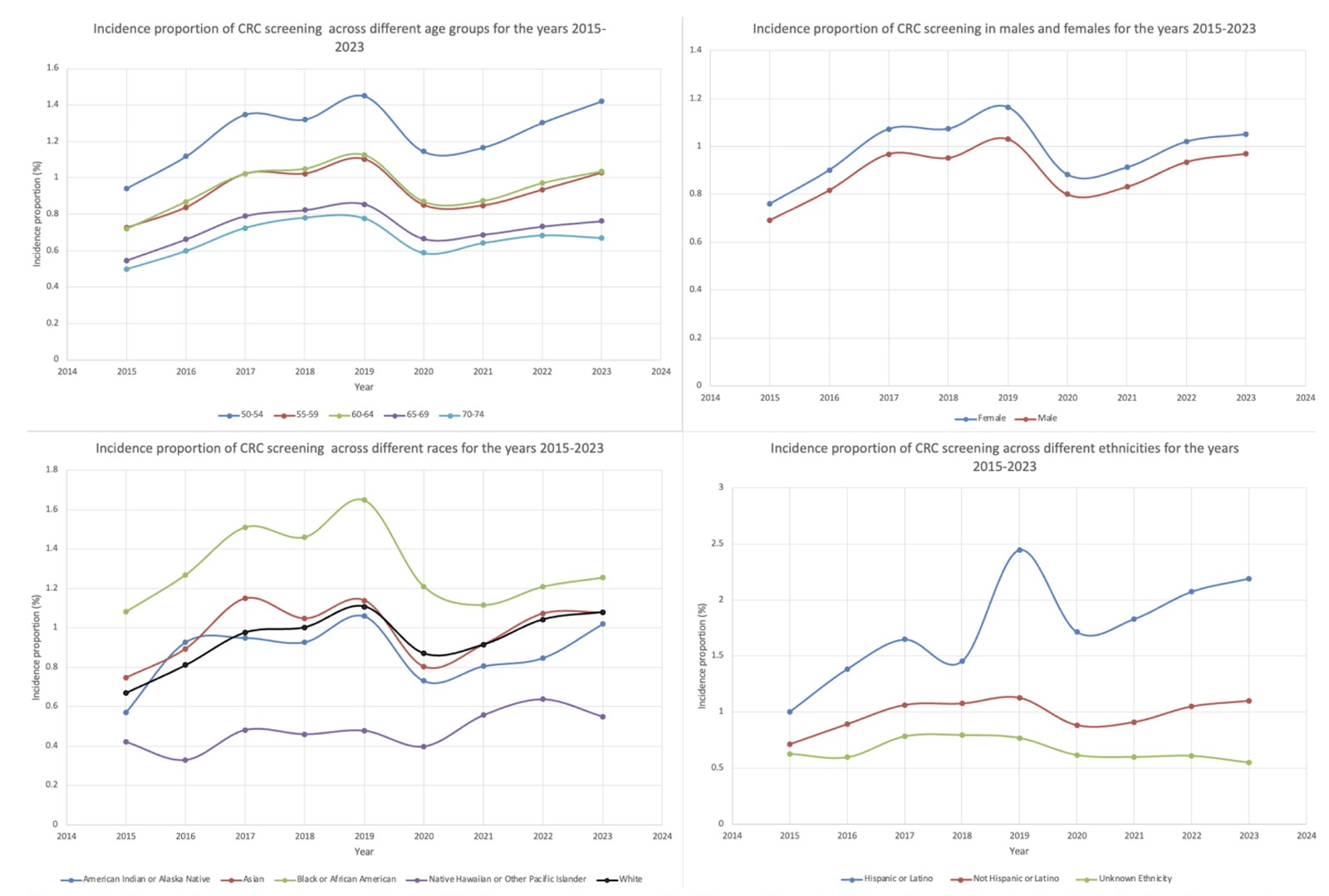
Figure: Figure 1: Incidence of CRC screening for the years 2015-2023
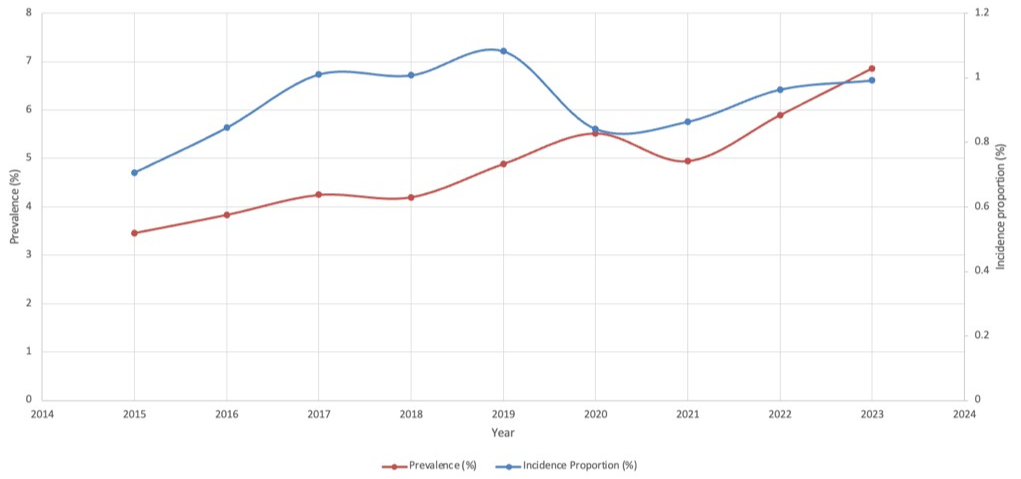
Figure: Figure 2: Incidence proportion of CRC screening stratified based on age, gender, race, and ethnicity for the years 2015-2023
Disclosures:
Omar Arman indicated no relevant financial relationships.
Zeid Jarrar indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Hebah Jaber indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Zeid Jarrar, MD2, Amer Arman, MD3, Blake Podger, MD1, Hebah Jaber, MD4, Mazen Zamzam, BS5, Osama Alshakhatreh, MD6, Jad Bou-Abdallah, MD1. P2611 - Colorectal Cancer Screening Trends and Disparities Across Demographics After USPSTF Guideline Updates and COVID-19 Disruptions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
