Monday Poster Session
Category: Esophagus
P2900 - Adenosquamous Carcinoma of the Gastroesophageal Junction: A Rare Dual Histology Case With Distinct Morphologies
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Carlos Cantu Lopez, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Carlos Cantu Lopez, MD, Maria Herrera Gonzalez, MD, Muhammad Hussain, MD, Yatinder Bains, MD
New York Medical College - Saint Michael's Medical Center, Newark, NJ
Introduction: Esophageal cancer (EC) is the ninth most common malignancy and the sixth leading cause of cancer-related mortality worldwide. Adenosquamous carcinoma (ASC) is a rare EC subtype, comprising approximately 1% of cases. It is defined by the coexistence of both glandular (adenocarcinoma) and squamous cell carcinoma components within a single lesion. ASC often presents at advanced stages, posing significant diagnostic and management challenges.
Case Description/
Methods: A 53-year-old male with no significant medical history presented with dizziness, one week of melena, and decreased appetite. Examination revealed pallor. Labs showed microcytic anemia (Hb 5.7 g/dL, MCV 78 fL, iron 29 µg/dL, ferritin 78 ng/mL). CT abdomen with IV contrast revealed a gastric mass with retroperitoneal lymphadenopathy (Figure 1). EGD demonstrated a large, ulcerated, fungating mass at the gastroesophageal (GE) junction, extending into the gastric fundus (Figure 2).
Biopsies revealed two distinct components: poorly differentiated, non-keratinizing squamous cell carcinoma in the stomach and moderately differentiated adenocarcinoma at the GE junction (Figure 2). Immunohistochemical staining of the gastric tumor was positive for p40, CK7, p16 (diffuse), and Helicobacter pylori. The GE junction tumor was p40-negative, showed wild-type p53 expression, and had a Ki-67 index of 80%. HPV in situ hybridization for types 16/18 and 31/33 was negative. The findings confirmed ASC with two histologically distinct malignant components. The patient was transfused, started on iron supplementation, and referred to oncology for outpatient management.
Discussion: ASC is a rare and aggressive malignancy of the esophagus and GE junction, with limited data available. Its diagnosis requires a high index of suspicion and thorough histologic and immunohistochemical analysis to distinguish it from other neoplasms. Dual morphology within a single tumor adds complexity and may influence treatment planning. This case highlights the importance of recognizing ASC early and coordinating multidisciplinary care to optimize outcomes.
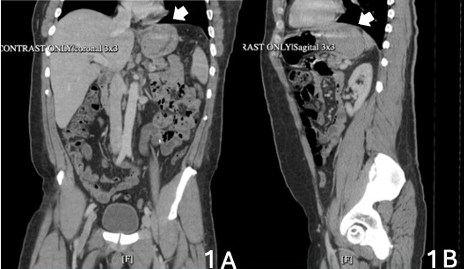
Figure: Figure 1. CT scan of the abdomen and pelvis, coronal (Figure A), and sagittal (Figure B) showing a mass-like density in the stomach fundus just below the EG junction.
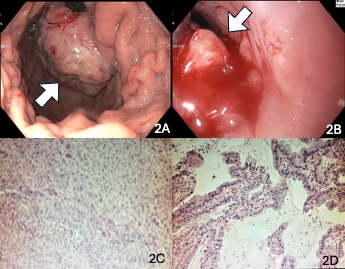
Figure: Figure 2. Large fungating and ulcerating mass at the gastroesophageal junction, protruding to the stomach and covering the entire fundus (Figure 2A). Large fungating and ulcerating mass with recent bleeding stigmata at the esophagus's lower third (Figure 2B). Stomach biopsy: Infiltrating squamous cell carcinoma, non-keratinizing type (Figure 3C). GE junction biopsy: Moderately adenocarcinoma (Figure 2D).
Disclosures:
Carlos Cantu Lopez indicated no relevant financial relationships.
Maria Herrera Gonzalez indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Carlos Cantu Lopez, MD, Maria Herrera Gonzalez, MD, Muhammad Hussain, MD, Yatinder Bains, MD. P2900 - Adenosquamous Carcinoma of the Gastroesophageal Junction: A Rare Dual Histology Case With Distinct Morphologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
New York Medical College - Saint Michael's Medical Center, Newark, NJ
Introduction: Esophageal cancer (EC) is the ninth most common malignancy and the sixth leading cause of cancer-related mortality worldwide. Adenosquamous carcinoma (ASC) is a rare EC subtype, comprising approximately 1% of cases. It is defined by the coexistence of both glandular (adenocarcinoma) and squamous cell carcinoma components within a single lesion. ASC often presents at advanced stages, posing significant diagnostic and management challenges.
Case Description/
Methods: A 53-year-old male with no significant medical history presented with dizziness, one week of melena, and decreased appetite. Examination revealed pallor. Labs showed microcytic anemia (Hb 5.7 g/dL, MCV 78 fL, iron 29 µg/dL, ferritin 78 ng/mL). CT abdomen with IV contrast revealed a gastric mass with retroperitoneal lymphadenopathy (Figure 1). EGD demonstrated a large, ulcerated, fungating mass at the gastroesophageal (GE) junction, extending into the gastric fundus (Figure 2).
Biopsies revealed two distinct components: poorly differentiated, non-keratinizing squamous cell carcinoma in the stomach and moderately differentiated adenocarcinoma at the GE junction (Figure 2). Immunohistochemical staining of the gastric tumor was positive for p40, CK7, p16 (diffuse), and Helicobacter pylori. The GE junction tumor was p40-negative, showed wild-type p53 expression, and had a Ki-67 index of 80%. HPV in situ hybridization for types 16/18 and 31/33 was negative. The findings confirmed ASC with two histologically distinct malignant components. The patient was transfused, started on iron supplementation, and referred to oncology for outpatient management.
Discussion: ASC is a rare and aggressive malignancy of the esophagus and GE junction, with limited data available. Its diagnosis requires a high index of suspicion and thorough histologic and immunohistochemical analysis to distinguish it from other neoplasms. Dual morphology within a single tumor adds complexity and may influence treatment planning. This case highlights the importance of recognizing ASC early and coordinating multidisciplinary care to optimize outcomes.
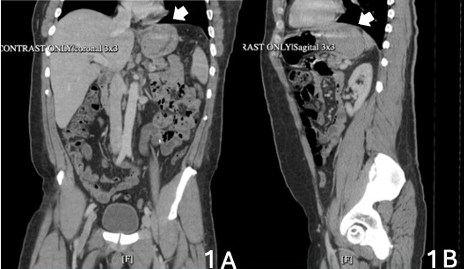
Figure: Figure 1. CT scan of the abdomen and pelvis, coronal (Figure A), and sagittal (Figure B) showing a mass-like density in the stomach fundus just below the EG junction.
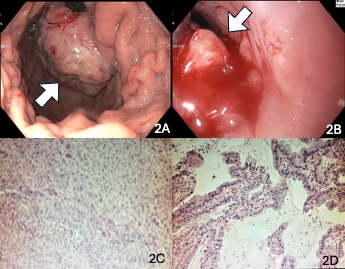
Figure: Figure 2. Large fungating and ulcerating mass at the gastroesophageal junction, protruding to the stomach and covering the entire fundus (Figure 2A). Large fungating and ulcerating mass with recent bleeding stigmata at the esophagus's lower third (Figure 2B). Stomach biopsy: Infiltrating squamous cell carcinoma, non-keratinizing type (Figure 3C). GE junction biopsy: Moderately adenocarcinoma (Figure 2D).
Disclosures:
Carlos Cantu Lopez indicated no relevant financial relationships.
Maria Herrera Gonzalez indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Carlos Cantu Lopez, MD, Maria Herrera Gonzalez, MD, Muhammad Hussain, MD, Yatinder Bains, MD. P2900 - Adenosquamous Carcinoma of the Gastroesophageal Junction: A Rare Dual Histology Case With Distinct Morphologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
