Monday Poster Session
Category: Esophagus
P2888 - Megaesophagus From Achalasia: A Rare Cause of Acute Hypoxic Respiratory Failure
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- EC
Ellen Choi, DO
Englewood Hospital and Medical Center
Englewood, NJ
Presenting Author(s)
Ellen Choi, DO, Yu-Han Chen, MD, Shalva Eliava, MD, Melanie Burgos, MD, Tanganyika Barnes, DO
Englewood Hospital and Medical Center, Englewood, NJ
Introduction: Achalasia is an esophageal motility disorder defined by a failure of peristalsis and inadequate relaxation of the lower esophageal sphincter, resulting in progressive esophageal dilation. Dysphagia, regurgitation of food, and chest discomfort are the primary symptoms of achalasia. In rare cases, an enlarged esophagus can obstruct the trachea and lead to respiratory complications. We present a case of acute respiratory failure caused by megaesophagus from achalasia.
Case Description/
Methods: A 56-year-old male with a history of asthma, 20-pack-year smoking history, and recent long-distance travel presented to the emergency department with acute dyspnea. The patient was tachypneic with diffuse wheezing and an oxygen saturation of 90%. Supplemental oxygen was administered, and intravenous methylprednisolone 40 mg and nebulized bronchodilators were given. Initial laboratory work revealed an elevated white blood cell count of 12,500 cells/μL. Chest X-ray was unremarkable. Computed tomography (CT) angiography was negative for pulmonary embolism but showed significant esophageal distension with retained food debris, an abrupt caliber change at the esophagogastric junction, and mural thickening along the greater curvature of the stomach. An upper endoscopy demonstrated retained liquid and solid material, which was removed using a Roth net and suctioning. There was narrowing at the esophagogastric junction without mass or malignancy in the gastric cardia. Biopsies from irregular mucosa in the distal esophagus were negative for eosinophilic esophagitis, Helicobacter pylori, and metaplasia. Esophageal manometry confirmed the diagnosis of achalasia, and the patient subsequently underwent a peroral endoscopic myotomy without complication.
Discussion: Severe esophageal dilation can compress the trachea, leading to acute hypoxic respiratory failure. Although pulmonary embolism was initially suspected based on the patient’s history, evaluation with CT angiography identified the esophageal origin of the symptoms and allowed for prompt endoscopic intervention to reverse the patient’s hypoxia. It is important to consider atypical presentations of respiratory distress, including non-pulmonary causes such as complications arising from esophageal dilation.
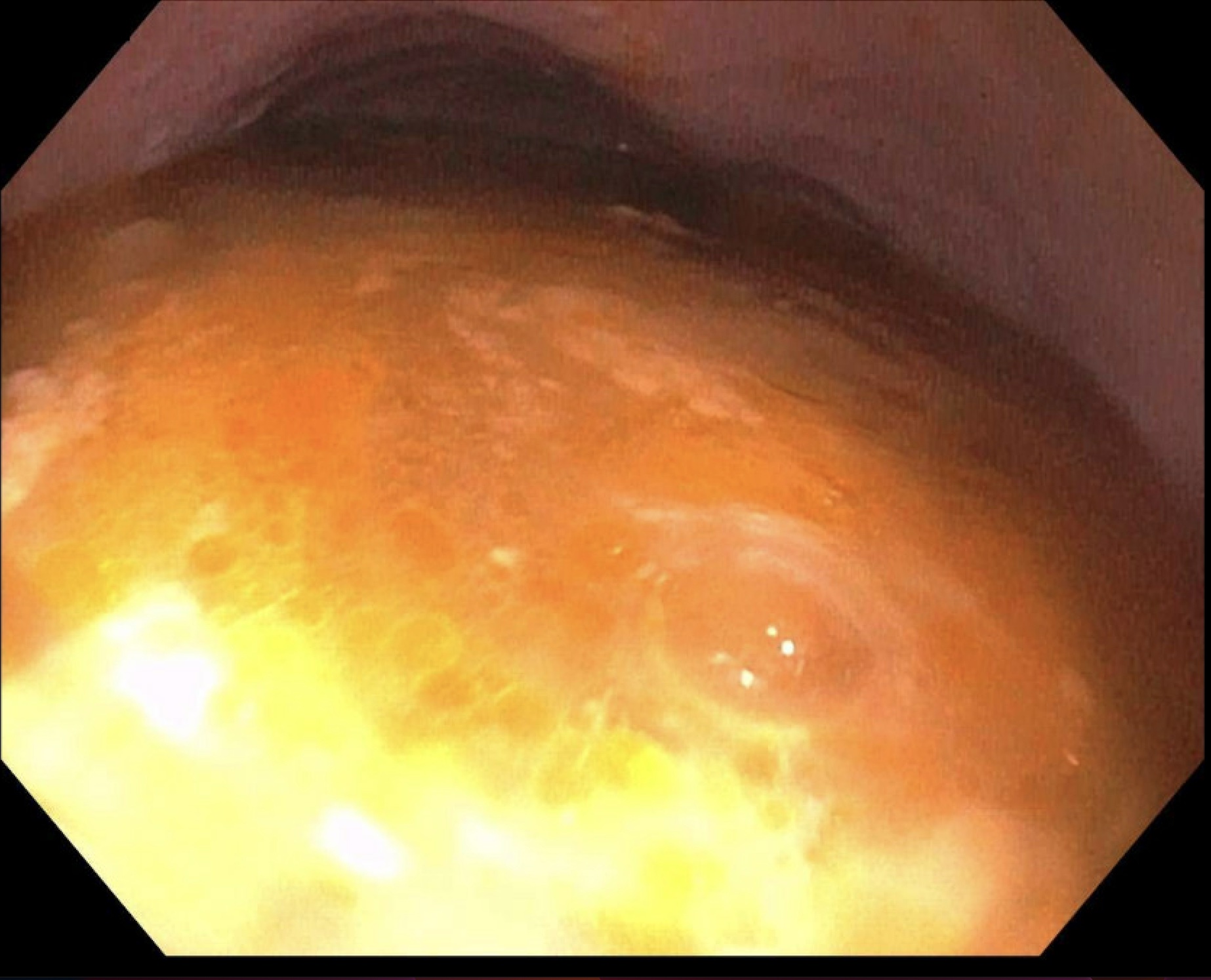
Figure: EGD demonstrates significant retention of food and fluid in the esophagus, proximal to a narrowing in the distal esophagus.
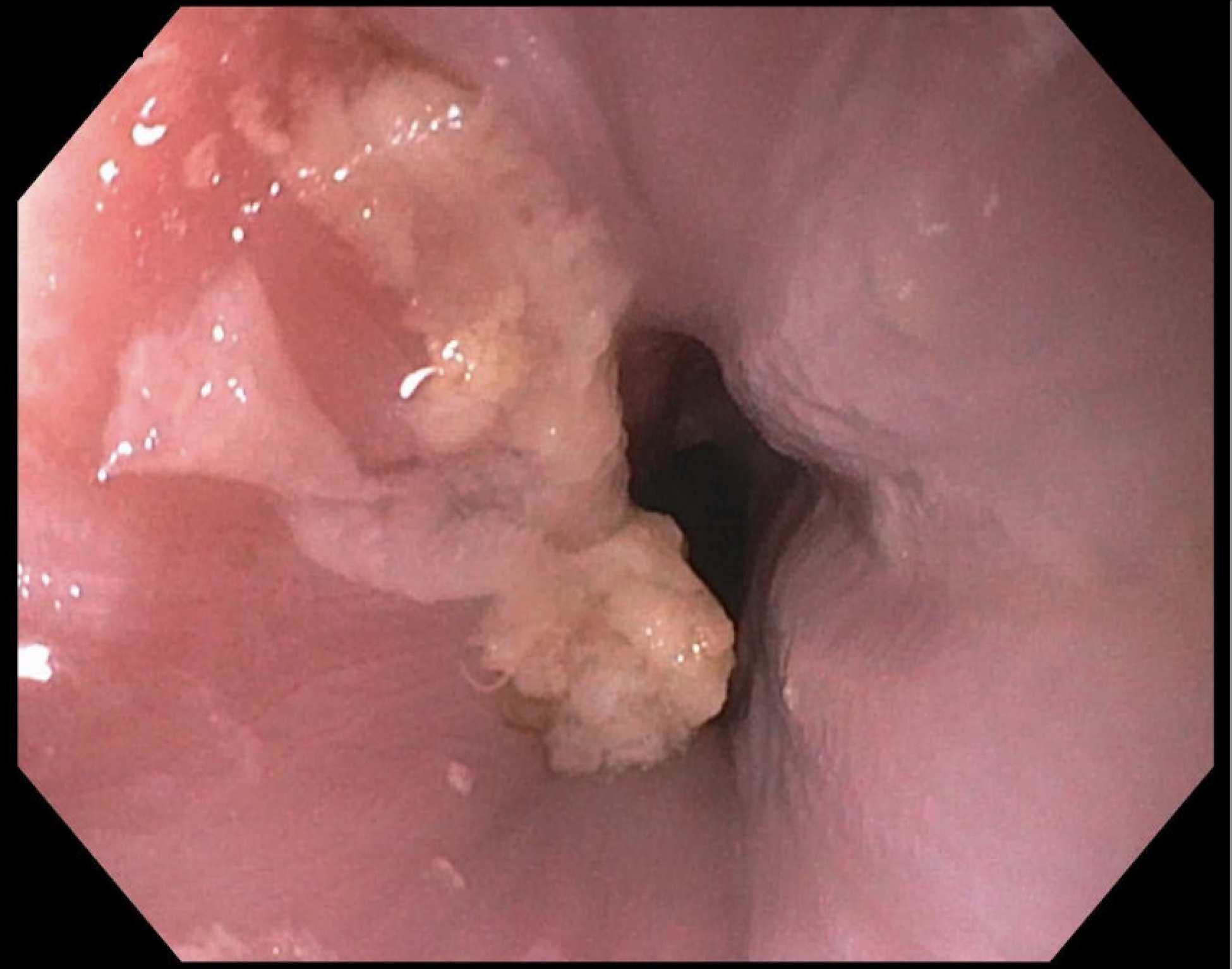
Figure: Distal esophageal luminal narrowing was visualized on EGD after food and fluid debris were removed with a Roth net.
Disclosures:
Ellen Choi indicated no relevant financial relationships.
Yu-Han Chen indicated no relevant financial relationships.
Shalva Eliava indicated no relevant financial relationships.
Melanie Burgos indicated no relevant financial relationships.
Tanganyika Barnes indicated no relevant financial relationships.
Ellen Choi, DO, Yu-Han Chen, MD, Shalva Eliava, MD, Melanie Burgos, MD, Tanganyika Barnes, DO. P2888 - Megaesophagus From Achalasia: A Rare Cause of Acute Hypoxic Respiratory Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Englewood Hospital and Medical Center, Englewood, NJ
Introduction: Achalasia is an esophageal motility disorder defined by a failure of peristalsis and inadequate relaxation of the lower esophageal sphincter, resulting in progressive esophageal dilation. Dysphagia, regurgitation of food, and chest discomfort are the primary symptoms of achalasia. In rare cases, an enlarged esophagus can obstruct the trachea and lead to respiratory complications. We present a case of acute respiratory failure caused by megaesophagus from achalasia.
Case Description/
Methods: A 56-year-old male with a history of asthma, 20-pack-year smoking history, and recent long-distance travel presented to the emergency department with acute dyspnea. The patient was tachypneic with diffuse wheezing and an oxygen saturation of 90%. Supplemental oxygen was administered, and intravenous methylprednisolone 40 mg and nebulized bronchodilators were given. Initial laboratory work revealed an elevated white blood cell count of 12,500 cells/μL. Chest X-ray was unremarkable. Computed tomography (CT) angiography was negative for pulmonary embolism but showed significant esophageal distension with retained food debris, an abrupt caliber change at the esophagogastric junction, and mural thickening along the greater curvature of the stomach. An upper endoscopy demonstrated retained liquid and solid material, which was removed using a Roth net and suctioning. There was narrowing at the esophagogastric junction without mass or malignancy in the gastric cardia. Biopsies from irregular mucosa in the distal esophagus were negative for eosinophilic esophagitis, Helicobacter pylori, and metaplasia. Esophageal manometry confirmed the diagnosis of achalasia, and the patient subsequently underwent a peroral endoscopic myotomy without complication.
Discussion: Severe esophageal dilation can compress the trachea, leading to acute hypoxic respiratory failure. Although pulmonary embolism was initially suspected based on the patient’s history, evaluation with CT angiography identified the esophageal origin of the symptoms and allowed for prompt endoscopic intervention to reverse the patient’s hypoxia. It is important to consider atypical presentations of respiratory distress, including non-pulmonary causes such as complications arising from esophageal dilation.
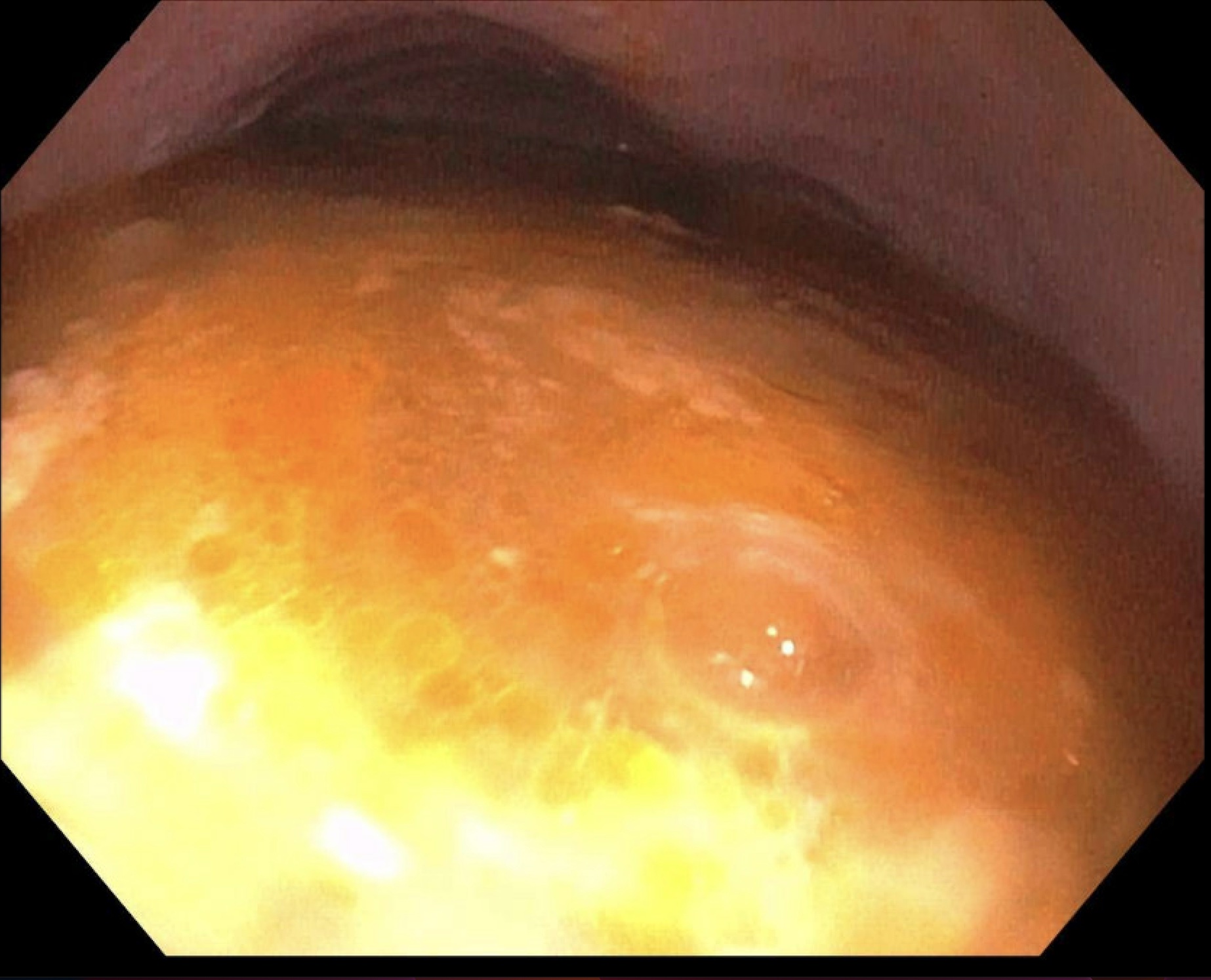
Figure: EGD demonstrates significant retention of food and fluid in the esophagus, proximal to a narrowing in the distal esophagus.
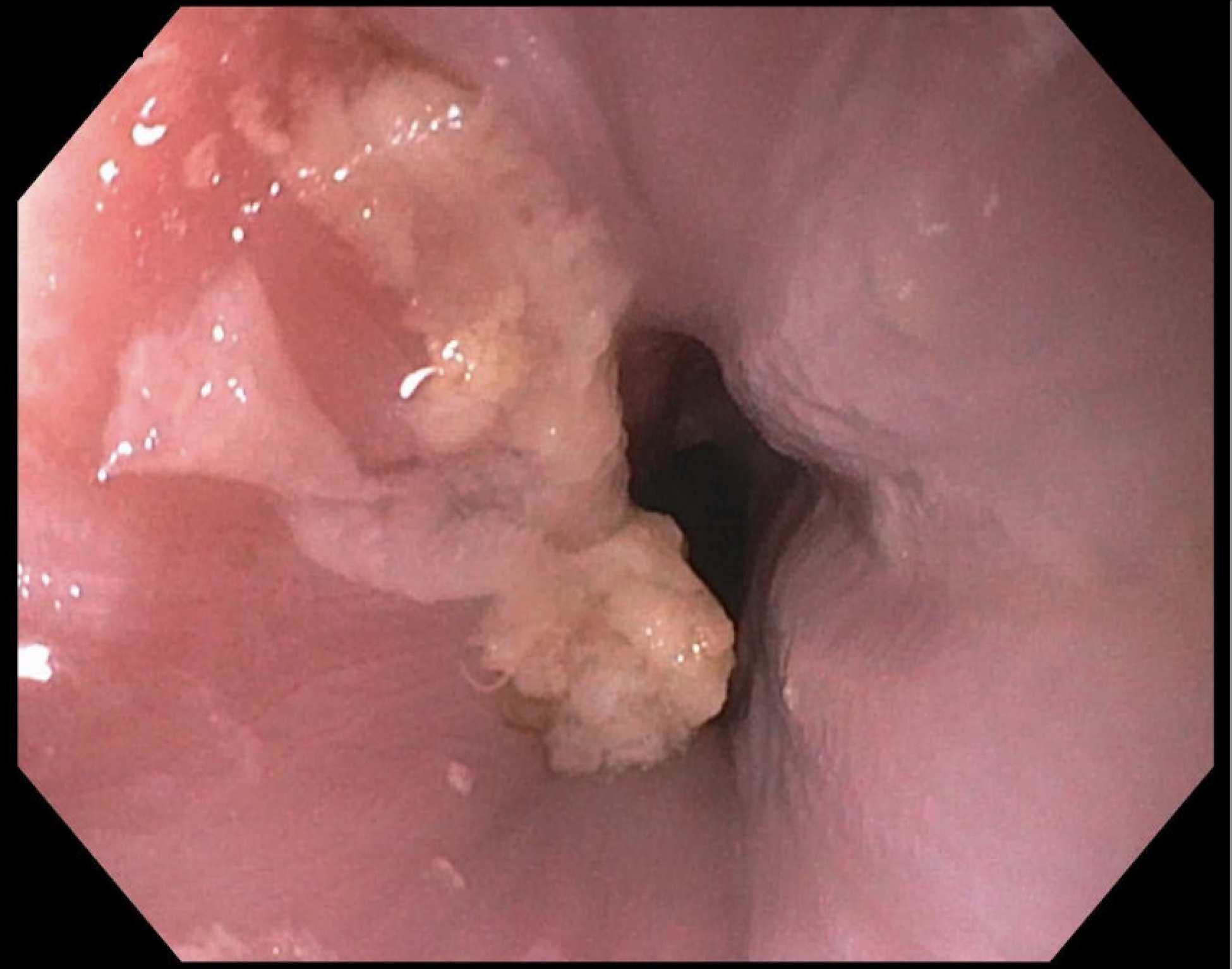
Figure: Distal esophageal luminal narrowing was visualized on EGD after food and fluid debris were removed with a Roth net.
Disclosures:
Ellen Choi indicated no relevant financial relationships.
Yu-Han Chen indicated no relevant financial relationships.
Shalva Eliava indicated no relevant financial relationships.
Melanie Burgos indicated no relevant financial relationships.
Tanganyika Barnes indicated no relevant financial relationships.
Ellen Choi, DO, Yu-Han Chen, MD, Shalva Eliava, MD, Melanie Burgos, MD, Tanganyika Barnes, DO. P2888 - Megaesophagus From Achalasia: A Rare Cause of Acute Hypoxic Respiratory Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
