Monday Poster Session
Category: Esophagus
P2887 - Acute Esophageal Necrosis and Herpes Esophagitis: Questioning a Possible Connection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- BK
Bhavjeet Kahlon, MD
Washington State University Elson S. Floyd School of Medicine
Everett, WA
Presenting Author(s)
Bhavjeet Kahlon, MD, Yeu-Yao Cheng, MD
Washington State University Elson S. Floyd School of Medicine, Everett, WA
Introduction: Acute esophageal necrosis (AEN) is a rare but severe clinical diagnosis that typically arises from a low vascular state, which predisposes the esophagus to injury by infections and toxins. Herpes esophagitis is commonly associated with immunocompromised status which in rare cases can progress to esophageal necrosis. This report describes a case of AEN with histological evidence of herpes simplex virus (HSV) prompting a discussion on whether the herpes infection was the cause or the consequence of AEN.
Case Description/
Methods: A 75 year-old female with hypertension, diabetes mellitus, COPD, diastolic heart failure, and dementia was found covered in feces during a welfare check. She was hypotensive (84/palp) and had new-onset atrial fibrillation (Afib) with a rapid ventricular rate. Her hospital course was notable for fluctuations in her mental status, mild rhabdomyolysis, sepsis secondary to a urinary tract infection, and left lower extremity deep venous thrombosis for which she was promptly started on anticoagulation in the setting of concomitant Afib. When her cognition transiently improved, she declined artificial feeding in particular after discussion with palliative care.When diet was advanced, she endorsed dysphagia and odynophagia. Upper endoscopy revealed circumferential blackening of the esophagus abruptly terminating at the gastroesophageal junction and two duodenal ulcers. Histopathology showed acute inflammation with fibrinopurulent exudate and HSV positive stain. Parenteral nutrition was not pursued given her expressed wishes and she transitioned to comfort care. She passed away four days after the endoscopic evaluation after.
Discussion: This case illustrates the two-hit hypothesis linked to the pathogenesis of esophageal necrosis wherein hypotension in the context of sepsis and atrial fibrillation, led to compromised esophageal mucosal perfusion, aggravated by multiple co-existing comorbidities. The second hit in this case could have been the HSV causing an opportunistic infection in an already necrotic tissue. It remains uncertain though, as HSV could have been the primary etiological factor driving the necrosis as observed in some case studies. In conclusion, this case emphasizes the multifactorial mature of AEN, the role of potential infectious etiologies like, HSV and the importance of involving palliative care as interventions may not always align with patients’ values and/or their prognosis, specifically in high risk complex cases.
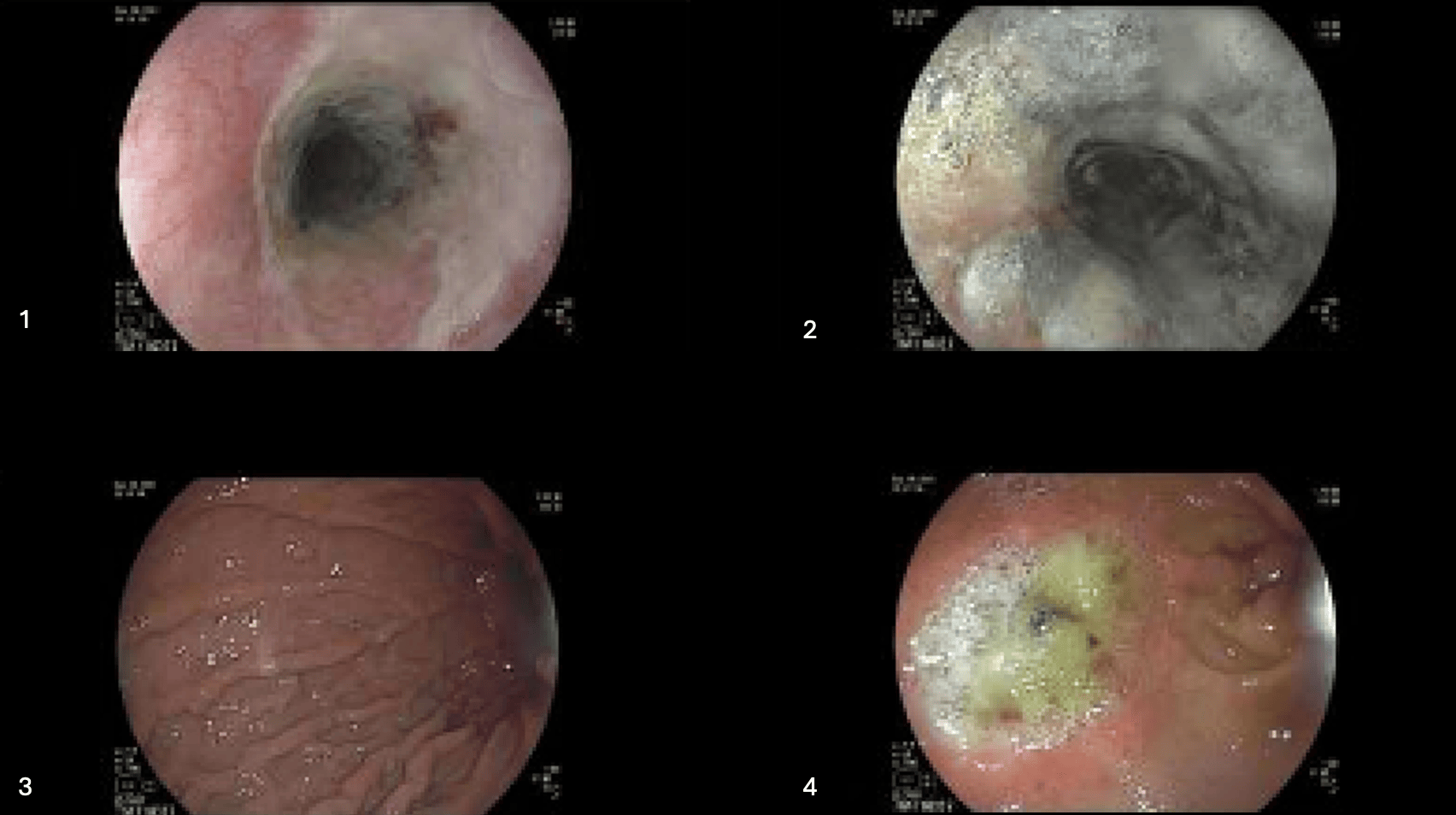
Figure: Figures 1-4. Endoscopy pictures showing relatively preserved upper third of esophagus (figure 1), necrotic lower esophagus (figure 2) and normal gastric mucosa (figure 3). Duodenal ulcer is shown in figure 4.
Disclosures:
Bhavjeet Kahlon indicated no relevant financial relationships.
Yeu-Yao Cheng indicated no relevant financial relationships.
Bhavjeet Kahlon, MD, Yeu-Yao Cheng, MD. P2887 - Acute Esophageal Necrosis and Herpes Esophagitis: Questioning a Possible Connection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Washington State University Elson S. Floyd School of Medicine, Everett, WA
Introduction: Acute esophageal necrosis (AEN) is a rare but severe clinical diagnosis that typically arises from a low vascular state, which predisposes the esophagus to injury by infections and toxins. Herpes esophagitis is commonly associated with immunocompromised status which in rare cases can progress to esophageal necrosis. This report describes a case of AEN with histological evidence of herpes simplex virus (HSV) prompting a discussion on whether the herpes infection was the cause or the consequence of AEN.
Case Description/
Methods: A 75 year-old female with hypertension, diabetes mellitus, COPD, diastolic heart failure, and dementia was found covered in feces during a welfare check. She was hypotensive (84/palp) and had new-onset atrial fibrillation (Afib) with a rapid ventricular rate. Her hospital course was notable for fluctuations in her mental status, mild rhabdomyolysis, sepsis secondary to a urinary tract infection, and left lower extremity deep venous thrombosis for which she was promptly started on anticoagulation in the setting of concomitant Afib. When her cognition transiently improved, she declined artificial feeding in particular after discussion with palliative care.When diet was advanced, she endorsed dysphagia and odynophagia. Upper endoscopy revealed circumferential blackening of the esophagus abruptly terminating at the gastroesophageal junction and two duodenal ulcers. Histopathology showed acute inflammation with fibrinopurulent exudate and HSV positive stain. Parenteral nutrition was not pursued given her expressed wishes and she transitioned to comfort care. She passed away four days after the endoscopic evaluation after.
Discussion: This case illustrates the two-hit hypothesis linked to the pathogenesis of esophageal necrosis wherein hypotension in the context of sepsis and atrial fibrillation, led to compromised esophageal mucosal perfusion, aggravated by multiple co-existing comorbidities. The second hit in this case could have been the HSV causing an opportunistic infection in an already necrotic tissue. It remains uncertain though, as HSV could have been the primary etiological factor driving the necrosis as observed in some case studies. In conclusion, this case emphasizes the multifactorial mature of AEN, the role of potential infectious etiologies like, HSV and the importance of involving palliative care as interventions may not always align with patients’ values and/or their prognosis, specifically in high risk complex cases.
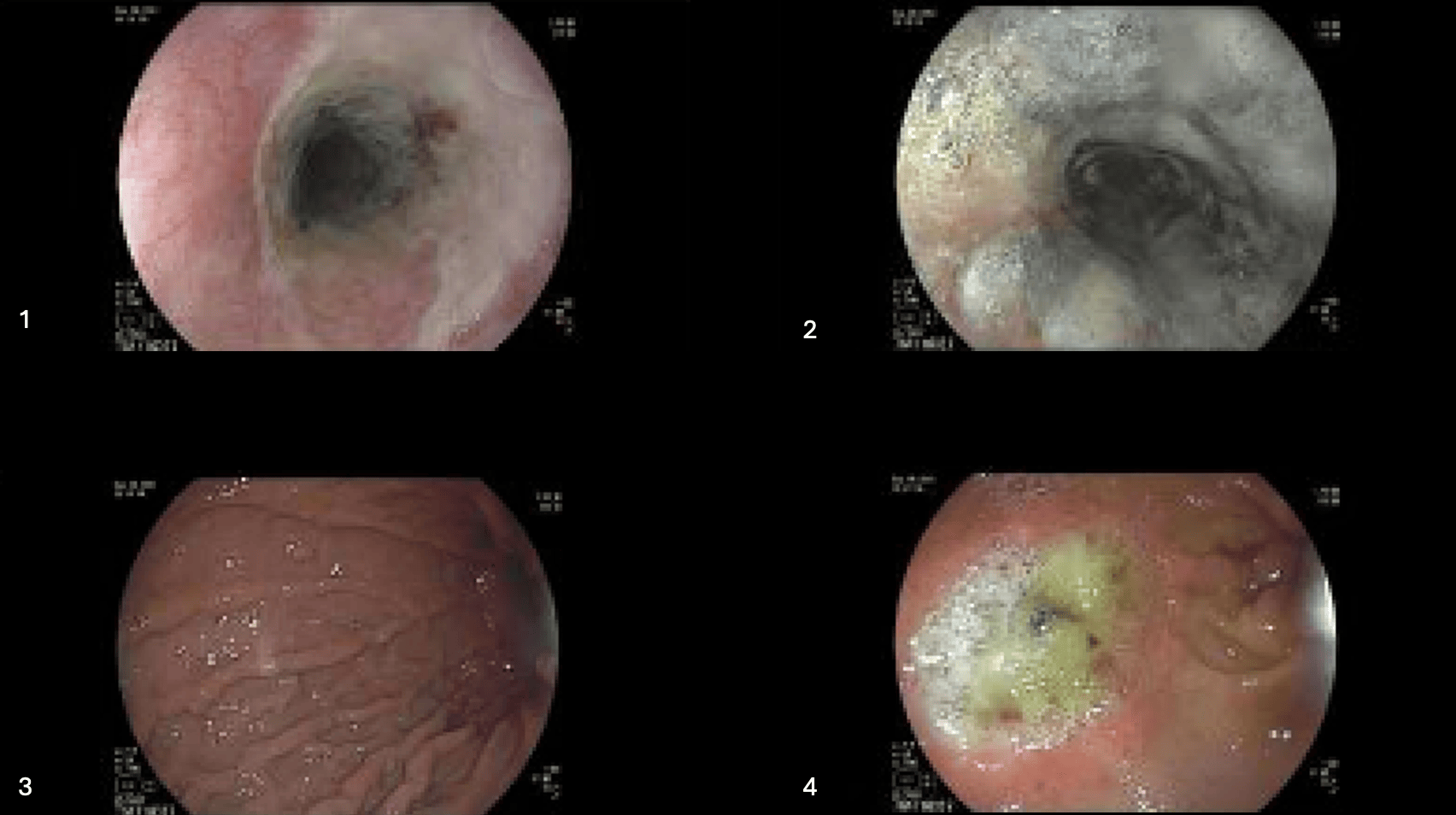
Figure: Figures 1-4. Endoscopy pictures showing relatively preserved upper third of esophagus (figure 1), necrotic lower esophagus (figure 2) and normal gastric mucosa (figure 3). Duodenal ulcer is shown in figure 4.
Disclosures:
Bhavjeet Kahlon indicated no relevant financial relationships.
Yeu-Yao Cheng indicated no relevant financial relationships.
Bhavjeet Kahlon, MD, Yeu-Yao Cheng, MD. P2887 - Acute Esophageal Necrosis and Herpes Esophagitis: Questioning a Possible Connection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
