Monday Poster Session
Category: General Endoscopy
P3027 - A Rare Case of Cronkhite-Canada Syndrome in a Young Male: Diagnostic and Therapeutic Challenges
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Maryam Salma Babar, MD (she/her/hers)
Cleveland Clinic Abu Dhabi
Al Reem Island, Abu Dhabi, United Arab Emirates
Presenting Author(s)
Maryam Salma. Babar, MD1, Anas Algammaz, MD2
1Cleveland Clinic Abu Dhabi, Al Reem Island, Abu Dhabi, United Arab Emirates; 2Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Cronkhite–Canada Syndrome (CCS) is a rare, nonhereditary gastrointestinal polyposis disorder characterized by chronic diarrhea, weight loss, and ectodermal changes such as alopecia and hyperpigmentation. Its pathogenesis remains unclear, and diagnosis relies on clinical, endoscopic, and histological findings
Case Description/
Methods: A 38-year-old male presented with a two-month history of postprandial diarrhea, nausea, vomiting, and generalized weakness, along with a 15 kg unintentional weight loss. He reported chronic abdominal pain worsened by meals and occasional blood-streaked stools, without melena or hematemesis. Physical examination revealed signs of malnutrition and ectodermal changes, including alopecia, nail dystrophy, and hyperpigmentation of the palms and soles. Laboratory workup showed hypoalbuminemia and iron deficiency anemia. Infectious screening, including stool cultures, Clostridioides difficile toxin, ova and parasite testing, and viral panels, was negative.
Endoscopic evaluation revealed erythematous mucosa in the stomach, duodenum, terminal ileum, and colon. Biopsies showed polypoid mucosa with cystically dilated glands, edematous lamina propria, and mixed inflammatory infiltrates rich in eosinophils and mononuclear cells, without dysplasia. Video capsule endoscopy demonstrated diffusely edematous and nodular gastric mucosa, elongated villi throughout the small bowel, and dark blood in the proximal ileum without a clear bleeding source. These findings supported a diagnosis of Cronkhite–Canada Syndrome.
The patient was started on a short course of intravenous corticosteroids, followed by oral prednisolone and azathioprine (Imuran) as a steroid-sparing agent. He also received nutritional support, proton pump inhibitors, and pancreatic enzyme supplements.At follow-up, the patient reported marked improvement in diarrhea, suggesting a positive response to immunosuppressive therapy. He remains under surveillance with routine labs and a scheduled endoscopy to assess mucosal healing
Discussion: This case underscores the importance of early diagnosis and multidisciplinary care in managing Cronkhite–Canada Syndrome, a rare but serious gastrointestinal polyposis disorder. The patient’s clinical improvement on steroids and azathioprine highlights the role of immunosuppression in addressing the inflammatory nature of CCS. Prompt treatment, nutritional support, and close surveillance are key to improving outcomes and reducing the risk of complications such as malnutrition and malignancy
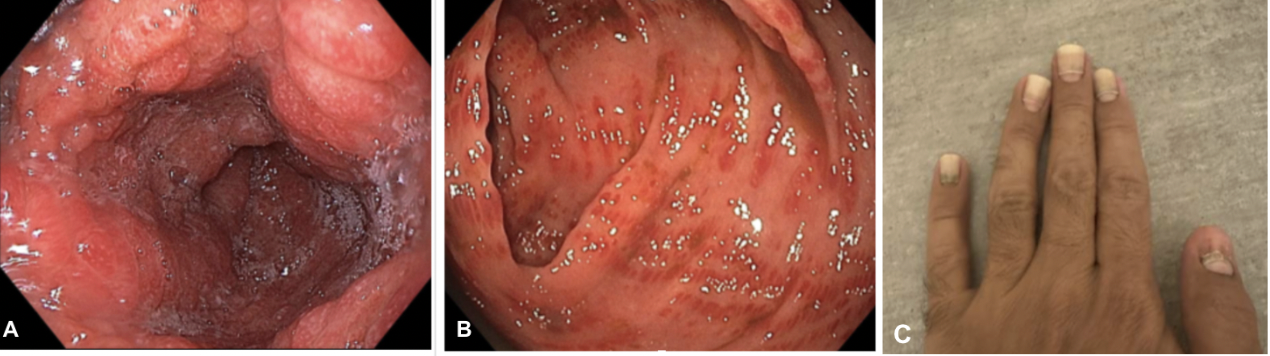
Figure: (A) Esophagogastroduodenoscopy (EGD) showing diffusely erythematous and edematous gastric mucosa.
(B) Colonoscopy revealing patchy erythema and mucosal edema throughout the colon.
(C) Fingernail atrophy characterized by thinning, ridging, and nail plate dystrophy, consistent with ectodermal changes seen in Cronkhite–Canada Syndrome
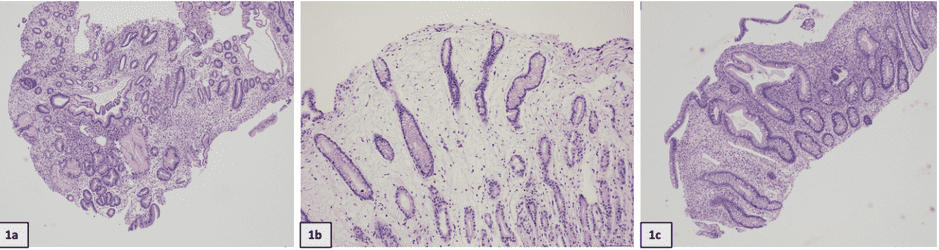
Figure:
Duodenal type mucosa with lamina propria edema, mixed inflammatory infiltrate, blunting with mixed chronic inflammatory infiltrate and focal superficial erosion (1a).
Gastric antral mucosa with lamina propria distension by bland uniform spindled cells in a loose fibromyxoid background associated with an eosinophil-rich inflammatory infiltrate (1b)
Polypoid colonic type mucosa with lamina propria edema, mixed inflammatory infiltrate, focal crypt branching with mixed chronic inflammatory infiltrate and focal superficial erosion (1c)
Disclosures:
Maryam Babar indicated no relevant financial relationships.
Anas Algammaz indicated no relevant financial relationships.
Maryam Salma. Babar, MD1, Anas Algammaz, MD2. P3027 - A Rare Case of Cronkhite-Canada Syndrome in a Young Male: Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Abu Dhabi, Al Reem Island, Abu Dhabi, United Arab Emirates; 2Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Cronkhite–Canada Syndrome (CCS) is a rare, nonhereditary gastrointestinal polyposis disorder characterized by chronic diarrhea, weight loss, and ectodermal changes such as alopecia and hyperpigmentation. Its pathogenesis remains unclear, and diagnosis relies on clinical, endoscopic, and histological findings
Case Description/
Methods: A 38-year-old male presented with a two-month history of postprandial diarrhea, nausea, vomiting, and generalized weakness, along with a 15 kg unintentional weight loss. He reported chronic abdominal pain worsened by meals and occasional blood-streaked stools, without melena or hematemesis. Physical examination revealed signs of malnutrition and ectodermal changes, including alopecia, nail dystrophy, and hyperpigmentation of the palms and soles. Laboratory workup showed hypoalbuminemia and iron deficiency anemia. Infectious screening, including stool cultures, Clostridioides difficile toxin, ova and parasite testing, and viral panels, was negative.
Endoscopic evaluation revealed erythematous mucosa in the stomach, duodenum, terminal ileum, and colon. Biopsies showed polypoid mucosa with cystically dilated glands, edematous lamina propria, and mixed inflammatory infiltrates rich in eosinophils and mononuclear cells, without dysplasia. Video capsule endoscopy demonstrated diffusely edematous and nodular gastric mucosa, elongated villi throughout the small bowel, and dark blood in the proximal ileum without a clear bleeding source. These findings supported a diagnosis of Cronkhite–Canada Syndrome.
The patient was started on a short course of intravenous corticosteroids, followed by oral prednisolone and azathioprine (Imuran) as a steroid-sparing agent. He also received nutritional support, proton pump inhibitors, and pancreatic enzyme supplements.At follow-up, the patient reported marked improvement in diarrhea, suggesting a positive response to immunosuppressive therapy. He remains under surveillance with routine labs and a scheduled endoscopy to assess mucosal healing
Discussion: This case underscores the importance of early diagnosis and multidisciplinary care in managing Cronkhite–Canada Syndrome, a rare but serious gastrointestinal polyposis disorder. The patient’s clinical improvement on steroids and azathioprine highlights the role of immunosuppression in addressing the inflammatory nature of CCS. Prompt treatment, nutritional support, and close surveillance are key to improving outcomes and reducing the risk of complications such as malnutrition and malignancy
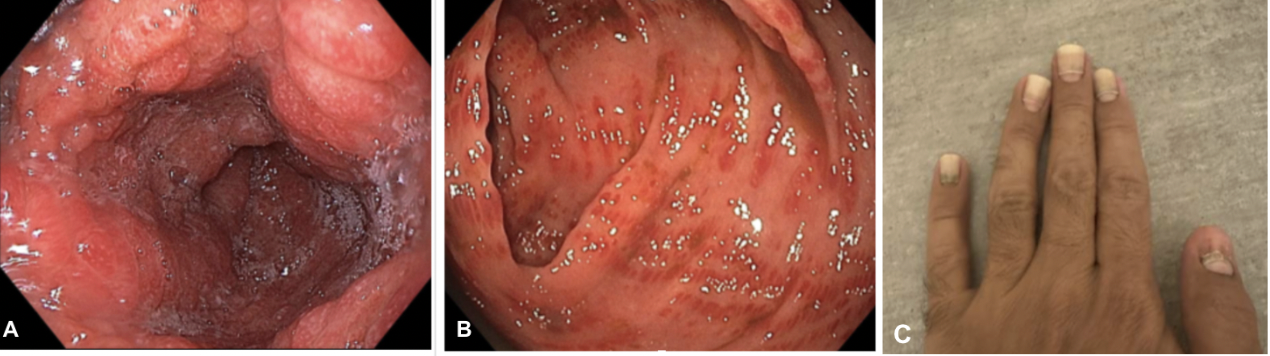
Figure: (A) Esophagogastroduodenoscopy (EGD) showing diffusely erythematous and edematous gastric mucosa.
(B) Colonoscopy revealing patchy erythema and mucosal edema throughout the colon.
(C) Fingernail atrophy characterized by thinning, ridging, and nail plate dystrophy, consistent with ectodermal changes seen in Cronkhite–Canada Syndrome
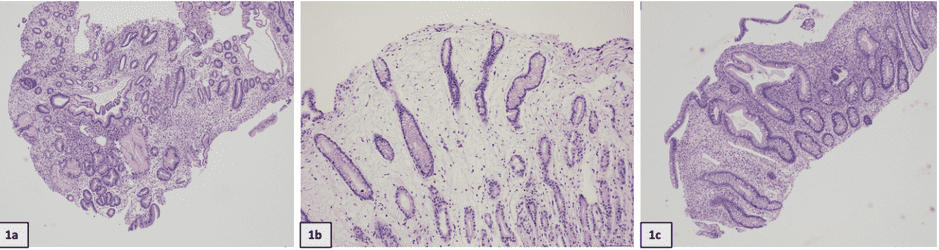
Figure:
Duodenal type mucosa with lamina propria edema, mixed inflammatory infiltrate, blunting with mixed chronic inflammatory infiltrate and focal superficial erosion (1a).
Gastric antral mucosa with lamina propria distension by bland uniform spindled cells in a loose fibromyxoid background associated with an eosinophil-rich inflammatory infiltrate (1b)
Polypoid colonic type mucosa with lamina propria edema, mixed inflammatory infiltrate, focal crypt branching with mixed chronic inflammatory infiltrate and focal superficial erosion (1c)
Disclosures:
Maryam Babar indicated no relevant financial relationships.
Anas Algammaz indicated no relevant financial relationships.
Maryam Salma. Babar, MD1, Anas Algammaz, MD2. P3027 - A Rare Case of Cronkhite-Canada Syndrome in a Young Male: Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
