Monday Poster Session
Category: GI Bleeding
P3134 - POSTER WITHDRAWN
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Claire Wang, 1, Samiksha Pandey, MD2, Jimmi Mangla, MD3, Michael Duffy, MD3, Nika Bakshi, 1, Inayat Gill, MD3
1Oakland University William Beaumont School of Medicine, Royal Oak, MI; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI; 3Corewell Health, Royal Oak, MI
Introduction: Jejunal diverticula are rare and often asymptomatic, but can sometimes lead to serious complications such as gastrointestinal bleeding. Diagnosing bleeding from the small intestine, especially the distal jejunum, is particularly challenging due to limited endoscopic access and intermittent bleeding.
Case Description/
Methods: An 82-year-old woman presented to the emergency department with lightheadedness and a gastrointestinal (GI) bleeding for a day. Following initial resuscitation and transfusion of two units of packed red blood cells, a computed tomography angiogram (CTA) of the abdomen and pelvis with intravenous contrast demonstrated no active bleeding. Esophagogastroduodenoscopy (EGD) and colonoscopy were initially planned; however, the patient developed hemodynamic instability, necessitating an emergent repeat CTA. The subsequent imaging revealed active contrast extravasation from a presumed jejunal diverticulum (Figure 1). Selective mesenteric arteriography failed to demonstrate active bleeding but was empirically embolized at the site correlating with the CTA findings. Due to ongoing clinical deterioration, an exploratory laparotomy was performed. Although the bowel appeared grossly normal, transillumination revealed a bleeding jejunal diverticulum on the mesenteric side (Figure 2). Segmental small bowel resection was completed, and histopathologic evaluation confirmed a benign diverticulum.
Discussion: This case illustrates the difficulty in identifying small bowel bleeding, especially when intermittent and imaging is inconclusive. Endoscopy has a limited role in managing jejunal bleeding. While CT angiography for an upper GI bleed has a sensitivity of 50–70%, it is insufficient to detect intermittent bleeding. Similarly, interventional angiography, with 40–86% sensitivity, can fail if no active bleeding occurs during the procedure. In our case, surgical exploration was necessary as the patient continued to bleed clinically. Additionally, transillumination was crucial in localizing the bleeding diverticulum, which otherwise would have been invisible. This case highlights the importance of acting promptly and using an interdisciplinary approach to manage complex gastrointestinal bleeding. When noninvasive imaging is inconclusive and the patient deteriorates despite minimally invasive approaches, surgical exploration should be considered without delay. This case underscores the role of gastroenterology, interventional radiology, and surgery in effective patient management.
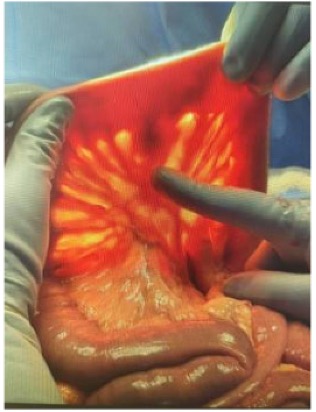
Figure: Figure 1. Sagittal CT angiography (CTA) images showing active jejunal diverticular bleeding (yellow arrows).
(A) Initial sagittal slice showing contrast extravasation in the jejunum.
(B) Adjacent sagittal slice highlighting the same bleed at a slightly different level.
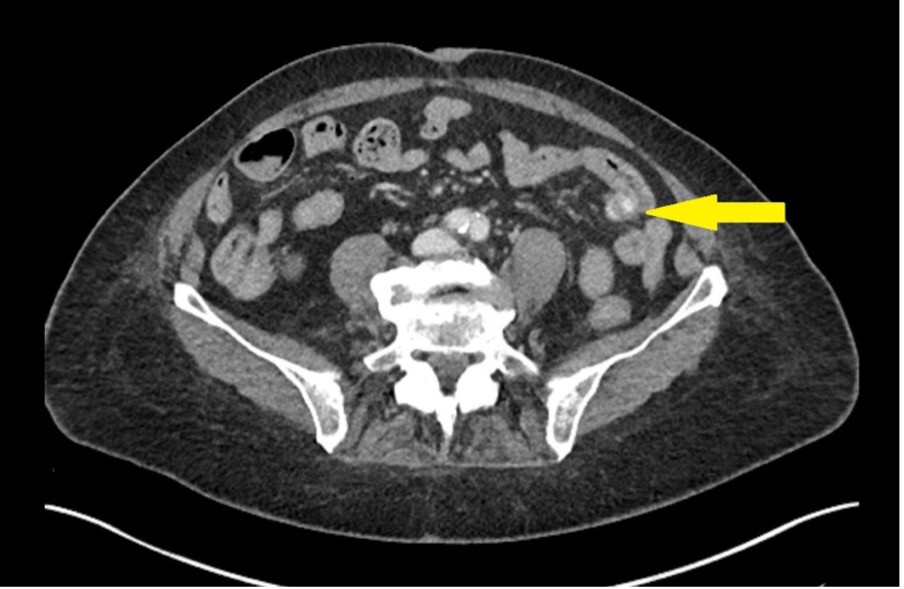
Figure: Figure 2. Intraoperative image showing a jejunal diverticulum on the antimesenteric border of the small intestine.
Disclosures:
Claire Wang indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Jimmi Mangla indicated no relevant financial relationships.
Michael Duffy indicated no relevant financial relationships.
Nika Bakshi indicated no relevant financial relationships.
Inayat Gill indicated no relevant financial relationships.
Claire Wang, 1, Samiksha Pandey, MD2, Jimmi Mangla, MD3, Michael Duffy, MD3, Nika Bakshi, 1, Inayat Gill, MD3. P3134 - Hidden in Plain Sight: Jejunal Diverticular Hemorrhage Unmasked, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Oakland University William Beaumont School of Medicine, Royal Oak, MI; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI; 3Corewell Health, Royal Oak, MI
Introduction: Jejunal diverticula are rare and often asymptomatic, but can sometimes lead to serious complications such as gastrointestinal bleeding. Diagnosing bleeding from the small intestine, especially the distal jejunum, is particularly challenging due to limited endoscopic access and intermittent bleeding.
Case Description/
Methods: An 82-year-old woman presented to the emergency department with lightheadedness and a gastrointestinal (GI) bleeding for a day. Following initial resuscitation and transfusion of two units of packed red blood cells, a computed tomography angiogram (CTA) of the abdomen and pelvis with intravenous contrast demonstrated no active bleeding. Esophagogastroduodenoscopy (EGD) and colonoscopy were initially planned; however, the patient developed hemodynamic instability, necessitating an emergent repeat CTA. The subsequent imaging revealed active contrast extravasation from a presumed jejunal diverticulum (Figure 1). Selective mesenteric arteriography failed to demonstrate active bleeding but was empirically embolized at the site correlating with the CTA findings. Due to ongoing clinical deterioration, an exploratory laparotomy was performed. Although the bowel appeared grossly normal, transillumination revealed a bleeding jejunal diverticulum on the mesenteric side (Figure 2). Segmental small bowel resection was completed, and histopathologic evaluation confirmed a benign diverticulum.
Discussion: This case illustrates the difficulty in identifying small bowel bleeding, especially when intermittent and imaging is inconclusive. Endoscopy has a limited role in managing jejunal bleeding. While CT angiography for an upper GI bleed has a sensitivity of 50–70%, it is insufficient to detect intermittent bleeding. Similarly, interventional angiography, with 40–86% sensitivity, can fail if no active bleeding occurs during the procedure. In our case, surgical exploration was necessary as the patient continued to bleed clinically. Additionally, transillumination was crucial in localizing the bleeding diverticulum, which otherwise would have been invisible. This case highlights the importance of acting promptly and using an interdisciplinary approach to manage complex gastrointestinal bleeding. When noninvasive imaging is inconclusive and the patient deteriorates despite minimally invasive approaches, surgical exploration should be considered without delay. This case underscores the role of gastroenterology, interventional radiology, and surgery in effective patient management.
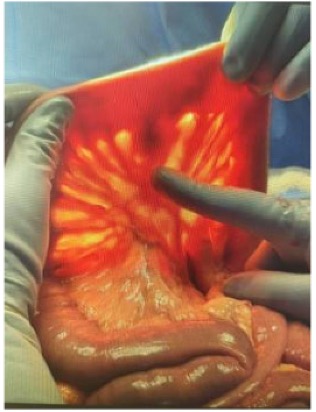
Figure: Figure 1. Sagittal CT angiography (CTA) images showing active jejunal diverticular bleeding (yellow arrows).
(A) Initial sagittal slice showing contrast extravasation in the jejunum.
(B) Adjacent sagittal slice highlighting the same bleed at a slightly different level.
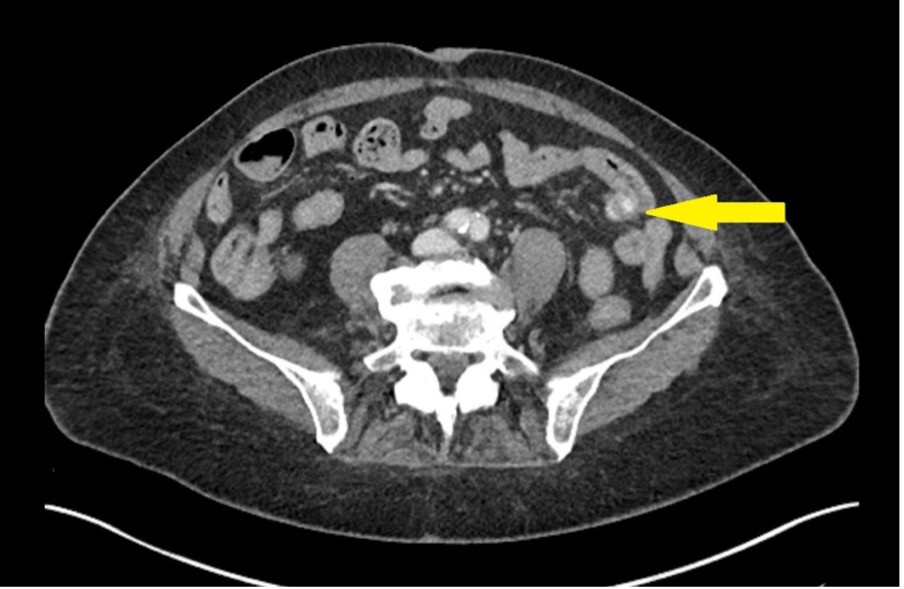
Figure: Figure 2. Intraoperative image showing a jejunal diverticulum on the antimesenteric border of the small intestine.
Disclosures:
Claire Wang indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Jimmi Mangla indicated no relevant financial relationships.
Michael Duffy indicated no relevant financial relationships.
Nika Bakshi indicated no relevant financial relationships.
Inayat Gill indicated no relevant financial relationships.
Claire Wang, 1, Samiksha Pandey, MD2, Jimmi Mangla, MD3, Michael Duffy, MD3, Nika Bakshi, 1, Inayat Gill, MD3. P3134 - Hidden in Plain Sight: Jejunal Diverticular Hemorrhage Unmasked, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
