Monday Poster Session
Category: GI Bleeding
P3125 - Haemorrhage in Hiding: Blue Rubber Bleb Nevus Syndrome as the Culprit
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Sandouka
University of Nicosia Medical School
Engomi, Nicosia, Cyprus
Presenting Author(s)
Ahmad Sandouka, 1, Sayed T. Shah, 2, Barakat Aburajab Altamimi, MD3
1University of Nicosia Medical School, London, England, United Kingdom; 2University Of Nicosia Medical School, Abbotsford, BC, Canada; 3Mercy Medical Center Cedar Rapids, Cedar Rapids, IA
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is an exceptionally rare condition marked by venous malformations in both the skin and gastrointestinal (GI) tract, frequently causing recurrent GI bleeding. Its rarity makes diagnosing and treating BRBNS especially challenging.
Case Description/
Methods: The patient, an 89-year-old male, had a history of coronary artery disease (post-stenting), atrial fibrillation (managed with Ticagrelor and Apixaban), gastroesophageal reflux disease, and jejunal angiodysplasia. He presented with melena, a significant drop in hemoglobin and a history of previous jejunal bleeding. In 2020, he had undergone double balloon enteroscopy. On his current presentation, enteroscopy revealed three angiectasias in the stomach, which were treated with argon plasma coagulation (APC). A colonoscopy showed small polyps but no active bleeding. A bleeding scan revealed tracer accumulation, pointing to small bowel bleeding. This was confirmed by a capsule endoscopy, which showed multiple phlebectasias consistent with BRBNS. Interventional radiology (IR) angiography did not show active extravasation. A follow-up double balloon enteroscopy revealed multiple venous blebs in the distal duodenum and proximal jejunum. Endoscopic clip placement was done, and no active bleeding was seen. Given the widespread nature of the venous malformations and the patient’s heart-related comorbidities, further interventions, including Sirolimus therapy, were postponed as the patient was moved to hospice care.
Discussion: This case underscores the rarity of BRBNS as a cause of recurrent GI bleeding. Even with multiple health issues such as coronary artery disease and atrial fibrillation, the bleeding was attributed to venous malformations in the small bowel. While BRBNS is often recognized in dermatology, its GI symptoms are less commonly seen. This makes diagnosis more difficult. The venous malformations were diagnosed using enteroscopy and capsule endoscopy. Despite treatment with APC and endoscopic clips, the extensive nature of the malformations made standard treatments less effective. This case highlights the importance of including rare conditions like BRBNS in the differential diagnosis of recurrent GI bleeding and the need for a multidisciplinary approach to manage such complex cases effectively.
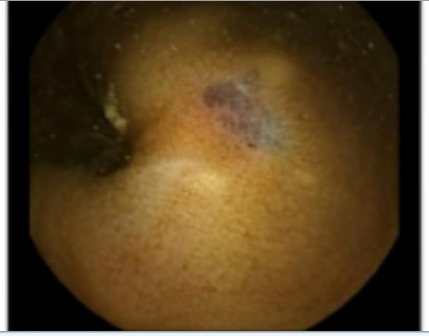
Figure: Endoscopic view showing a venous malformation with bluish discoloration, typical of BRBNS.
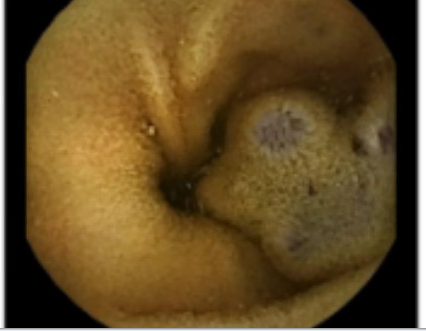
Figure: Endoscopic view of multiple venous blebs in the small bowel, characteristic of BRBNS
Disclosures:
Ahmad Sandouka indicated no relevant financial relationships.
Sayed Shah indicated no relevant financial relationships.
Barakat Aburajab Altamimi indicated no relevant financial relationships.
Ahmad Sandouka, 1, Sayed T. Shah, 2, Barakat Aburajab Altamimi, MD3. P3125 - Haemorrhage in Hiding: Blue Rubber Bleb Nevus Syndrome as the Culprit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Nicosia Medical School, London, England, United Kingdom; 2University Of Nicosia Medical School, Abbotsford, BC, Canada; 3Mercy Medical Center Cedar Rapids, Cedar Rapids, IA
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is an exceptionally rare condition marked by venous malformations in both the skin and gastrointestinal (GI) tract, frequently causing recurrent GI bleeding. Its rarity makes diagnosing and treating BRBNS especially challenging.
Case Description/
Methods: The patient, an 89-year-old male, had a history of coronary artery disease (post-stenting), atrial fibrillation (managed with Ticagrelor and Apixaban), gastroesophageal reflux disease, and jejunal angiodysplasia. He presented with melena, a significant drop in hemoglobin and a history of previous jejunal bleeding. In 2020, he had undergone double balloon enteroscopy. On his current presentation, enteroscopy revealed three angiectasias in the stomach, which were treated with argon plasma coagulation (APC). A colonoscopy showed small polyps but no active bleeding. A bleeding scan revealed tracer accumulation, pointing to small bowel bleeding. This was confirmed by a capsule endoscopy, which showed multiple phlebectasias consistent with BRBNS. Interventional radiology (IR) angiography did not show active extravasation. A follow-up double balloon enteroscopy revealed multiple venous blebs in the distal duodenum and proximal jejunum. Endoscopic clip placement was done, and no active bleeding was seen. Given the widespread nature of the venous malformations and the patient’s heart-related comorbidities, further interventions, including Sirolimus therapy, were postponed as the patient was moved to hospice care.
Discussion: This case underscores the rarity of BRBNS as a cause of recurrent GI bleeding. Even with multiple health issues such as coronary artery disease and atrial fibrillation, the bleeding was attributed to venous malformations in the small bowel. While BRBNS is often recognized in dermatology, its GI symptoms are less commonly seen. This makes diagnosis more difficult. The venous malformations were diagnosed using enteroscopy and capsule endoscopy. Despite treatment with APC and endoscopic clips, the extensive nature of the malformations made standard treatments less effective. This case highlights the importance of including rare conditions like BRBNS in the differential diagnosis of recurrent GI bleeding and the need for a multidisciplinary approach to manage such complex cases effectively.
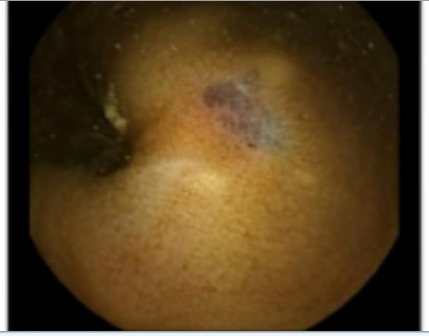
Figure: Endoscopic view showing a venous malformation with bluish discoloration, typical of BRBNS.
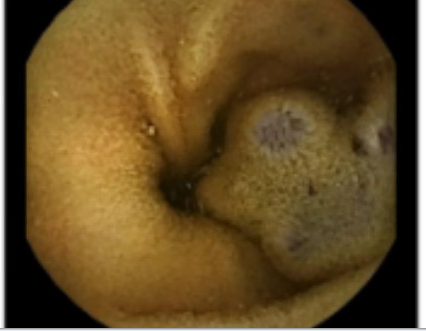
Figure: Endoscopic view of multiple venous blebs in the small bowel, characteristic of BRBNS
Disclosures:
Ahmad Sandouka indicated no relevant financial relationships.
Sayed Shah indicated no relevant financial relationships.
Barakat Aburajab Altamimi indicated no relevant financial relationships.
Ahmad Sandouka, 1, Sayed T. Shah, 2, Barakat Aburajab Altamimi, MD3. P3125 - Haemorrhage in Hiding: Blue Rubber Bleb Nevus Syndrome as the Culprit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
